Ankylosing Septic Arthritis of the TMJ
Nini K*, Ghazoui H, Bennaoui Y, Aziz Z, Fawzi S and Mansouri Hattab N
Oral and Maxillofacial Surgery Department, Cadi Ayyad University, Morocco
Received Date: 28/04/2025; Published Date: 02/06/2025
*Corresponding author: Nini Khaoula, Oral and Maxillofacial Surgery Department, Cadi Ayyad University, Morocco
Introduction
Septic arthritis of the temporomandibular joint (TMJ) is a rare infection of the joint space, which can be caused by bacteria or fungi [1]. The most common pathogens responsible for this infection include Staphylococcus aureus, Neisseria gonorrhoeae, Haemophilus influenzae, and Streptococcus [2]. Despite its clinical significance, the pathogenesis of TMJ septic arthritis remains poorly understood [3]. This condition often arises from the direct extension of infections in the head and neck region, though hematogenous dissemination can occasionally be the source. Clinical manifestations include TMJ pain, swelling, trismus, and malocclusion. However, these symptoms are often less typical than in the past, likely due to the widespread use of antibiotics[4].
Delayed treatment of TMJ septic arthritis can lead to severe complications, both systemic, such as septic shock, and local, particularly temporomandibular ankylosis [3]. These complications underscore the importance of early diagnosis and intervention.
In this article, we report the case of a patient who presented with facial cellulitis complicated by septic ankylosis of the temporomandibular joint. To date, there have been no published reports of septic arthritis of the TMJ leading to ankylosis and its subsequent surgical management, making this case an important addition to the literature.
Case Report
A 62-year-old female patient presented to the emergency department with a history of high blood pressure and blindness, along with swelling of the left cheek associated with a toothache. The patient reported that the swelling had been evolving for a month and had not subsided despite dental treatment. She had also consulted traditional practitioners who applied a cocktail of medicinal plants to the left cheek.
Upon examination, the patient was stable, with no dyspnea, dysphagia, or fever. She had multiple ulcerative skin lesions on the cheek and temporal region, identified as burns due to the application of the herbal treatment, along with a tender and red swelling of the left cheek centered around a fistula leaking pus (Figure 1). An intraoral examination revealed limited mouth opening and multiple carious lesions, particularly affecting the left upper third molar.
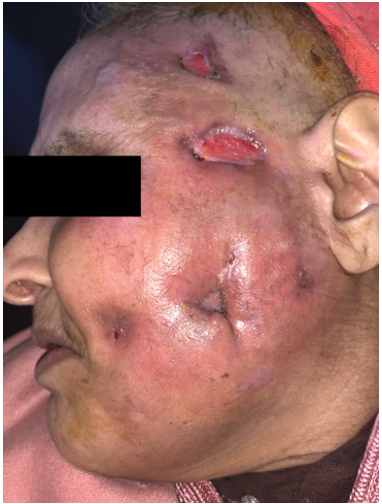
Figure 1: Initial presentation showing ulcerative skin lesions on the cheek and temporal region, with tender erythematous swelling of the left cheek centered around a draining fistula.
Laboratory tests showed neutrophilic leukocytosis, with a CRP level of 21. A facial CT scan revealed infiltration of the masseter and cutaneous tissues of the cheek with emphysema and bone demineralization of the TMJ and the left mandibular ramus (Figure 2).

Figure 2: Coronal view of CT scan of the face showing infiltration of the masseter and cutaneous tissues of the cheek with emphysema and bone demineralization of the TMJ and the left mandibular ramus.
The patient underwent surgical drainage in the operating room and was hospitalized. She was started on amoxicillin-clavulanic acid and metronidazole. The fistulas were surgically removed, and the burns were treated with daily wound care and dressings. The bacteriological study of the pus revealed a polymicrobial flora.
Due to her limited mouth opening, tooth extraction was not immediately possible. Physiotherapy was recommended to improve mouth opening before extraction. The patient showed favorable progress and was discharged after 15 days of hospitalization.
Two weeks later, she returned to the emergency department with swelling of the left temporal region (Figure 3) and pus leakage. At this point, her mouth opening was reduced to 1 cm, and she had developed a fever.
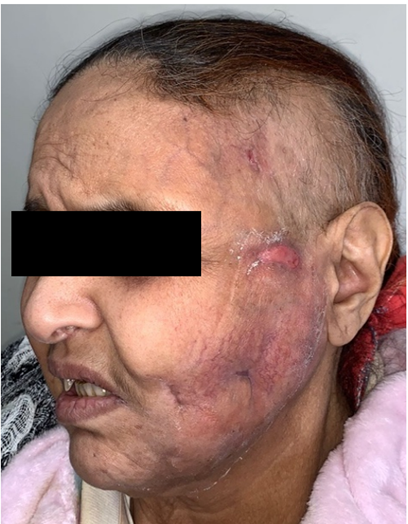
Figure 3: Patient appearance two weeks after initial management, showing left temporal swelling and purulent discharge.
The patient was scheduled for exploratory TMJ surgery via a preauricular approach. Upon opening the temporal space, pus was drained and sent for further examination. The head of the condyle appeared gray and was fused to the lytic zygomatic arch. A condylectomy and cavity lavage were performed (Figure 4), along with the extraction of tooth 28 (FDI nomenclature). At this stage, the patient was treated with ceftriaxone and metronidazole.
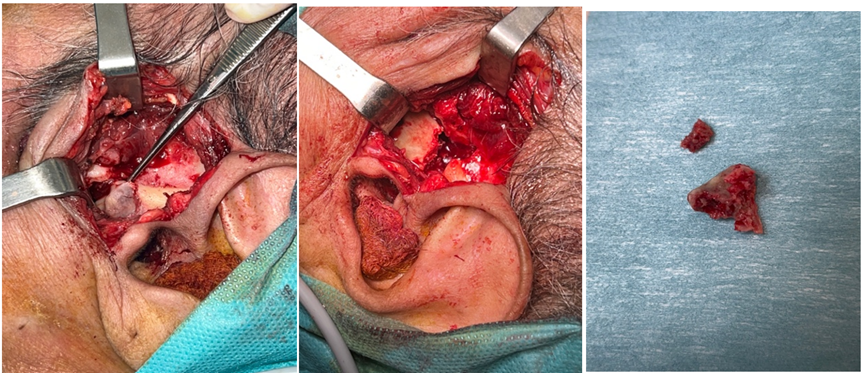
Figure 4: Intraoperative views of the right temporomandibular joint (TMJ). The first image shows a grey, necrotic condylar head fused to the lytic zygomatic arch. The following images depict the condylectomy procedure.
Histopathological examination revealed inflammatory changes and bacterial analysis identified a multi-resistant Morganella morganii, sensitive only to imipenem and ertapenem. The patient's treatment was adjusted accordingly.
Unfortunately, despite treatment, the patient did not respond and developed cerebral empyema two weeks later. She passed away 10 days after.
Discussion
Septic arthritis of the Temporomandibular Joint (TMJ) is rarely reported in the literature [4]. This low incidence is likely due to both the rarity of these infections and the potential for diagnostic errors. Common symptoms include TMJ pain, trismus, signs of dental articulation disorder, and occasionally, local or systemic infectious symptoms. The diagnosis of TMJ septic arthritis and condylar osteoarthritis is established through a combination of clinical evaluation, radiological imaging, and cytobacterial analysis of intra-articular fluid [3].
Susceptible patients are those with diabetes, systemic lupus erythematosus, rheumatic arthritis, or other immunosuppressive diseases [5]. Contamination may result from the extension of an adjacent infection in soft tissues or bone (dental or ENT), hematogenous spread of bacteria from a distant infection or intravenous drug use, or direct inoculation through traumatic or intra-operative penetration of the joint space. Recent studies have shown that microorganisms are most commonly seeded hematogenously, although the original infectious sites are often occult. Staphylococcus aureus is the most commonly isolated organism from patients with septic arthritis of the temporomandibular joint (TMJ), although Streptococcus species, Neisseria, and Haemophilus influenzae have also been reported in the literature [4]. In our case, the infection caused by Morganella morganii, a nosocomial bacterium, was likely disseminated during the initial drainage, facilitating the implantation of this multi-resistant organism and aggravating the infection's progression. Morganella morganii is a gram-negative bacterium from the Enterobacteriaceae family. It is typically facultatively anaerobic and can thrive under a wide range of cultural conditions. This bacterium is often part of the normal intestinal flora of humans and animals but can become pathogenic when it enters sterile areas or occurs under conditions of immunosuppression[6].
If septic arthritis is suspected, prompt computed tomography (CT) is recommended, as delayed treatment is associated with significant morbidity. Further evaluation with magnetic resonance imaging (MRI) should be considered if the CT results are inconclusive but clinical suspicion remains high. If imaging confirms the presence of an effusion, joint aspiration is necessary [7]. The aspirate should be assessed for color and turbidity as initial indicators of infection, and microscopically examined for joint fluid analysis. Additionally, the fluid should be sent for Gram stain, culture, and sensitivity testing to identify the causative organism [1].
Given the limited number of reported cases and the absence of controlled trials, a clear consensus on the most effective treatment for TMJ septic arthritis remains elusive. However, a combination of antimicrobial therapy, adequate drainage, and joint rest are critical components of management. Since Staphylococcus aureus is the most commonly identified pathogen in TMJ septic arthritis, empiric therapy with an antistaphylococcal antibiotic should be initiated immediately after obtaining aspirate and blood cultures [8].
Several studies have shown that when a joint abscess has developed, drainage should be performed immediately, as the proximity of the temporomandibular joint (TMJ) to the skull base increases the potential for intracranial spread of infection. Exploration of the TMJ is necessary, and if bone erosion is suspected, a condylectomy should be carried out. This approach has demonstrated better outcomes, with the ability to maintain an open mouth and preserve dental articulation[9]. In this case, a delayed diagnosis, along with delayed abscess drainage and condylectomy, resulted in resistance to medical treatment and the development of a cerebral empyema, which led to the patient's death.
Complications of TMJ septic arthritis include a high incidence of local infection spread,recurrent infections, damage to the joint's articular surfaces, and fibrous or bony ankylosis of the joint [8]. In cases of severe joint destruction, such as in osteomyelitis-associated disease or when conservative drainage approaches fail, surgical interventions like condylar shaving or condylectomy may be required [1].
Conclusion
Septic arthritis of the temporomandibular joint is a rare but serious condition that can lead to life-threatening complications if not promptly diagnosed and treated. This case illustrates the importance of early intervention, appropriate antimicrobial therapy, and timely surgical management. This report contributes to the limited body of literature on TMJ septic arthritis and emphasizes the need for heightened clinical suspicion, especially in immunocompromised or medically complex patients.
References
- Dias Ferraz A, Spagnol G, Alves Maciel F, Monteiro Pinotti M, et al Septic arthritis of the temporomandibular joint: Case series and literature review, CRANIO®, 2021; 39(no 6): p. 541‑548. doi: 10.1080/08869634.2019.1661943.
- Wittig J, Borumandi F, Gaggl A, et al. Septic arthritis of the temporomandibular joint leading to an epidural abscess », BMJ Case Reports, 2018; p. bcr-2017-223563. doi: 10.1136/bcr-2017-223563.
- Constant M, Nicot R, Maes JM, Raoul G, et al. Arthrite septique temporomandibulaire avec résorption condylienne secondaire, Revue de Stomatologie, de Chirurgie Maxillo-faciale et de Chirurgie Orale, 2016; 117(no 4): p. 294‑297. doi: 10.1016/j.revsto.2016.07.018.
- Ayachi S, Mziou Z, Moatemri R, et al. Bilateral septic arthritis of the temporo mandibular joint: case report », Pan Afr Med J, 2016; 25. doi: 10.11604/pamj.2016.25.100.7943.
- Winslow CP, Dichard A, et al. Osteomyelitis of the temporomandibular joint », American Journal of Otolaryngology, 2001; 22(no 2): p. 142‑145. doi: 10.1053/ajot.2001.22577.
- Zaric RZ, Jankovic S, Zaric M, Milosavljevic M, Stojadinovic M, et al. Antimicrobial treatment of Morganella morganii invasive infections: Systematic review », Indian Journal of Medical Microbiology, 2021; 39(no 4): p. 404‑412. doi: 10.1016/j.ijmmb.2021.06.005.
- Al-Khalisy H, Nikiforov I, Mansoora Q, Goldman J, et al. Septic arthritis in the temporomandibular joint », North Am J Med Sci, 2015; 7(no 10): p. 480. doi: 10.4103/1947-2714.168678.
- Gayle EA, Young SM, McKenna SJ, et al. Septic Arthritis of the Temporomandibular Joint: Case Reports and Review of the Literature, The Journal of Emergency Medicine, 2013; 45(no 5): p. 674‑678. doi: 10.1016/j.jemermed.2013.01.034.
- Xiao D, Feng X, Huang H, et al. Severe septic arthritis of the temporomandibular joint with pyogenic orofacial infections: A case report and review of the literature, Experimental and Therapeutic Medicine, 2017; 14(no1): p. 141‑146. doi: 10.3892/etm.2017.4510.

