Co-infection of Tuberculous and Cryptococcus Meningitis in a Pediatric Patient: A Rare Case Report from Sukkur, Sindh, Pakistan
Waqar Ahmed*, Fareeda, Amber Shabir, Parveen Wassan, Arbab Ali, Saba Pahore and Nosheen
Sindh institute of child health and neonatology (SICHN), Sukkur, Pakistan
Received Date: 30/04/2025; Published Date: 30/05/2025
*Corresponding author: Waqar Ahmed, Sindh institute of child health and neonatology (SICHN), Sukkur, Pakistan
Abstract
This case report describes a rare case of co-infection with Cryptococcus neoformans and Mycobacterium tuberculosis in a previously healthy child, highlighting the diagnostic and therapeutic challenges in such a complex case. The patient initially presented with fever, seizures, and signs of meningitis, and was diagnosed through cerebrospinal fluid analysis and neuroimaging. Despite the rarity of such co-infections in immunocompetent pediatric patients, the child showed clinical improvement following antifungal and anti-tuberculosis therapy. This case underscores the importance of early recognition, advanced immunodeficiency workup, and the need for multidisciplinary management, especially in regions with a high prevalence of tuberculosis. The report also emphasizes the necessity of developing specialized care facilities for managing complex infections in the pediatric population.
Keywords: Cryptococcosis; Tuberculosis; Coinfection; HIV; Opportunistic Infections; Pakistan; SICHN
Introduction
Tuberculosis remains one of the most common infectious diseases, particularly in developing countries, such as Pakistan. Although it is a preventable condition, more than one million children under the age of 15 are affected each year [1]. Globally, tuberculosis is responsible for approximately 239,000 childhood deaths annually [2]. Due to its paucibacillary nature, diagnosing tuberculosis in the pediatric population remains a significant challenge. Tuberculous Meningitis (TBM) is the most severe form of tuberculosis, often presenting with nonspecific clinical features. Children affected by TBM are at a significantly increased risk of both mortality and long-term neurological morbidity [3]. Diagnosing TBM is challenging; therefore, a combination of radiological and laboratory investigations is required. Cerebrospinal Fluid (CSF) analysis, including CSF GeneXpert, CSF DR, and CSF culture, was performed. Among these, CSF culture remains the gold standard for confirming the diagnosis of tuberculous meningitis [4].
Similar to tuberculous meningitis, cryptococcal meningitis is a serious life-threatening infection involving the central nervous system. It is caused by Cryptococcus neoformans, an encapsulated fungal organism [5]. Cryptococcal infections primarily occur in immunocompromised patients, particularly those with organ transplantation or AIDS. Involvement in immunocompetent children or adults is rare [6].
Co-infection with cryptococcal meningitis and tuberculous meningitis is very rare, although a few case reports and case series have been documented, primarily in adult populations. However, there is limited literature describing such co-infections in the pediatric population, especially in our region. We report a rare case of cryptococcal and tuberculous meningitis co-infection in an immunocompetent child, highlighting diagnostic challenges and management considerations.
Case Summary
In April 2025, a previously healthy 6-year-old male child, fully vaccinated and with appropriate developmental milestones, presented with a three weeks history of high-grade intermittent fever followed by generalized seizures for two weeks. The fever had a sudden onset, occurred in multiple daily episodes, and was treated symptomatically by a local practitioner. Due to persistent fever spikes, the child developed seizures—initially focal on the left side, later progressing to generalized tonic-clonic activity lasting approximately 30 minutes, with up-rolling of the eyes and generalized stiffness.
He was admitted to a secondary facility and managed presumptively for meningitis with parenteral antibiotics. Despite fourteen days of inpatient care, his condition deteriorated, with persistent fever and seizures, and he was referred to our tertiary care center, Children’s Hospital, Sukkur.
Upon admission, the child was in a semi-conscious state with a GCS score of 9/15. Neurological examination revealed hypotonia, reduced muscle bulk, and marked right-sided hemiparesis (power 2/5 in both the upper and lower limbs). Deep tendon reflexes were grade II bilaterally, plantar reflexes were extensor reflexes, and superficial reflexes were preserved. Meningeal signs were positive, and fundoscopy revealed bilateral optic disc pallor. Sensory modalities cannot be reliably assessed because of altered consciousness.
Baseline laboratory tests were conducted, along with neuroimaging and Cerebrospinal Fluid (CSF) analysis. Brain magnetic resonance imaging revealed basal and leptomeningeal enhancement, chronic infarcts in the left basal ganglia, and microhemorrhage. The opening pressure was not documented during lumbar puncture. CSF analysis showed pleocytosis (WBC 64/cmm; neutrophils 44%, lymphocytes 66%), elevated protein (91 mg/dL), and low glucose (31 mg/dL). India ink staining was positive, and the fungal culture confirmed Cryptococcus neoformans. The CSF bacterial culture was negative. Ziehl-Neelsen staining and cultures for Mycobacterium tuberculosis in the CSF were also negative.
The child underwent EEG, which showed right focal centro-temporal epileptiform discharges. This supported the diagnosis of seizure disorder in the context of CNS infection (Figure 2).
Immunological workup included serum immunoglobulin levels, which were within normal limits. HIV testing was also performed and the results were found to be negative. However, advanced tests, such as phagocytic function assays, T-cell function tests, and B- and T-cell enumeration, could not be performed because of the unavailability of these facilities in our setup and the financial constraints faced by the family.
The gastric aspirate GeneXpert was positive for Mycobacterium tuberculosis with indeterminate rifampicin resistance. Chest X-ray and brain CT (from the prior hospital) were reported to be normal. Abdominal ultrasonography and carotid Doppler performed at our center were also normal. A transthoracic echocardiogram was also performed to rule out cardiac involvement and was found to be normal.
Based on the clinical presentation and confirmatory investigations, cryptococcal meningitis with tuberculous co-infection was diagnosed. The child was managed in the pediatric ICU with multidisciplinary inputs from neurology, infectious diseases, and physiotherapy.
Initial supportive care included Nasogastric (NG) feeding, oxygen therapy (initially required), and physiotherapy. Antiepileptic medications were administered to control seizures, and neuroprotective strategies were implemented to maintain normoglycemia, normothermia, and adequate cerebral perfusion. The patient was started on induction-phase antifungal therapy with Amphotericin B and high-dose fluconazole alongside first-line Anti-Tuberculous Therapy (ATT) and corticosteroids.
Over the course of four weeks, the patient showed marked improvement. He became afebrile, seizures ceased, consciousness level improved (GCS now 12/15), and he was weaned off oxygen. A follow-up CSF examination revealed normalization of the parameters.
The child remains admitted for ongoing care but is clinically stable. The discharge planning is ongoing. The family has been extensively counseled. Follow-up will continue in pediatric neurology, infectious disease, and physiotherapy clinics. Long-term antifungal and anti-TB therapy will be continued with close outpatient monitoring.
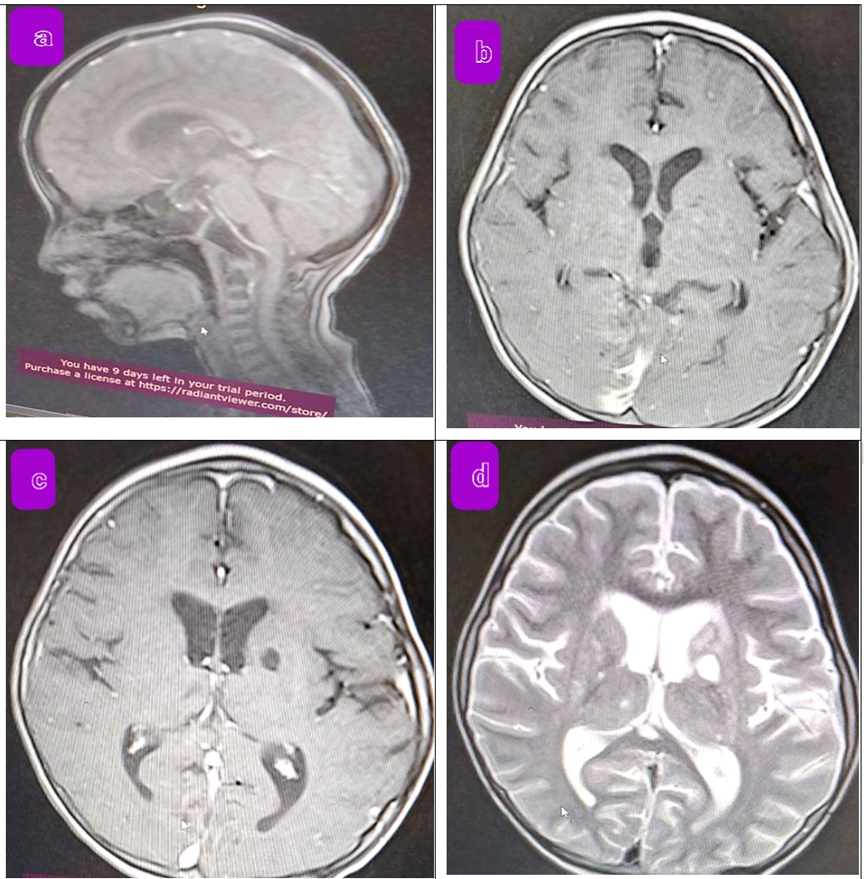
Figure 1: MRI Brain Findings in a Child with Suspected Tuberculous and Cryptococcal Meningitis.
T1-weighted mid sagittal image of brain and cervical spine showing leptomeningeal enhancement
b. T1-weighted axial image showing basal meningeal enhancement involving supratentorial and infratentoroial regions
c. FLAIR image demonstrating chronic infarcts and leptomeningeal enhancement with tiny micro hemorrhages
d. T2-weighted image showing symmetrical ventriculomegaly with periventricular T2 hyperintensities, showing infarct low on T1 and high on T2 areas

Figure 2: Abnormal EEG findings suggestive of right focal centro-temporal epileptiform discharges.
Discussion
This case highlights an unusual presentation of cryptococcal meningitis in an immunocompetent child, manifesting with fever and seizures, and confirmed through CSF analysis. Although cryptococcal meningitis is typically observed in immunocompromised individuals, its occurrence in immunocompetent children is rare. Similar cases have been reported, such as a 5-year-old immunocompetent girl from India who presented with prolonged fever and headache and was eventually diagnosed with cryptococcal meningitis [7].
Following the IDSA guidelines, we initiated the induction phase of treatment with amphotericin B and high-dose fluconazole to manage the infection effectively [8].
In our case, the diagnosis was further complicated by a co-infection with Mycobacterium tuberculosis (TB). Dual infections such as these are exceedingly uncommon in the pediatric population and are usually observed in the context of immunosuppression. A case in Mexico involved a 9-year-old girl with systemic lupus erythematosus on immunosuppressive therapy who developed concurrent cryptococcal and TB meningitis [9]. Additionally, a retrospective study from South India found similar cases in adults, all associated with immunocompromised states [10]
Despite negative CSF-DR and Gene Expert results, we are treating this patient with tuberculosis meningitis (TBM) based on clinical CNS manifestations and neuroimaging findings revealing basal meningeal enhancement and infarcts—features consistent with TBM [11]. A positive gastric aspirate Gene Expert further supported this diagnosis. Negative CSF results can occur because of factors such as prior antibiotic use or the low bacillary nature of TBM. The literature empirically supports the diagnosis of TBM, particularly when other samples, such as gastric aspirates, test positive despite negative CSF findings [12].
Following the confirmed diagnosis, intensive treatment for tuberculous meningitis (TBM) was initiated. This was in addition to the previously started antifungal therapy with amphotericin B and fluconazole for suspected cryptococcal meningitis, which was administered according to the IDSA guidelines. Anti-tuberculosis therapy (ATT) was initiated along with adjunctive dexamethasone in line with standard TBM protocols [13].
The patient had completed four weeks of antifungal therapy with amphotericin B and high-dose fluconazole, and three weeks of intensive-phase anti-tuberculosis treatment, with no observed complications. Repeat CSF is clear, with negative Indian ink and culture results. Clinically, the patient is stable, off oxygen, neurologically improved, and tolerating NG feeds well. The family has been counseled on home-based care, including physiotherapy, feeding, and adherence to TB treatment. Discharge is planned with follow-up in neurology, ID, and physiotherapy clinics.
Conclusion
This case presents a rare co-infection with Cryptococcus neoformans and Mycobacterium tuberculosis in a pediatric patient, marking the first such occurrence in our region. Despite conducting a basic immunodeficiency workup, this case highlights the need for more advanced immune testing to explore the potential underlying factors. Although the patient has shown significant improvement, the ongoing development of advanced diagnostic and therapeutic facilities is essential to enhance our ability to manage complex infections. This case also underscores the importance of early recognition and multidisciplinary management of pediatric co-infections.
References
- World Health Organization. Report of the first meeting of the WHO Diagnostic Technical Advisory Group for Neglected Tropical Diseases, Geneva, Switzerland, 30–31 October 2019. World Health Organization, 2020.
- Brooks MB, Malik A, Khan S, Ahmed JF, Siddiqui S, Jaswal M, Saleem S, Amanullah F, Becerra MC, Hussain H. Predictors of unsuccessful tuberculosis treatment outcomes in children from a prospective cohort study in Pakistan. Journal of global health, 2021; 11: 04011.
- Donald PR, Schoeman JF. Central nervous system tuberculosis in children. Chapter 38, 413–423 in textbook; Tuberculosis, a comprehensive clinical reference by H Simon Schaaf and Alimuddin I Zumla.
- Thwaites GE, Cahu TTH, Farrar JJ. Improving the bacterialogical diagnosis of Tuberculous meningitis. Int J Tuberc Lung Dis, 2004; 42: 378–379. doi: 10.1128/JCM.42.1.378-379.2004.
- Yuanjie Z, Jianghan C, Nan X, Xiaojun W, Hai W, Wanqing L, et al. Cryptococcal meningitis in immunocompetent children. Mycoses, 2012; 55(2): 168-171.
- Speed BR, Kaldor J. Rarity of cryptococcal infection in children. Pediatr Infect Dis J, 1997; 16: 536–537.
- Othman N, Abdullah NA, Wahab ZA. Cryptococcal meningitis in an immunocompetent child: a case report and literature review. Southeast Asian J Trop Med Public Health, 2004; 35(4): 930-934.
- Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clinical infectious diseases, 2010; 50(3): 291-322.
- Martinez-Longoria CA, Rubio-Perez NE, Rios-Solis JE, Garcia-Rodriguez F. Severe meningoencephalitis co-infection due to Cryptococcus neoformans and Mycobacterium tuberculosis in a child with systemic lupus erythematosus. International Journal of Infectious Diseases, 2015; 33: 106-108.
- Suresh CS, Ninan MM, Zachariah A, Michael JS. Cryptococcosis with tuberculosis: overlooked coinfections. Journal of global infectious diseases, 2021; 13(3): 139-141.
- Soni N, Kumar S, Shimle A, Ora M, Bathla G, Mishra P. Cerebrovascular complications in tuberculous meningitis—A magnetic resonance imaging study in 90 patients from a tertiary care hospital. The Neuroradiology Journal, 2020; 33(1): 3-16.
- Liu Z, Zhu X, Zhang S, Li D, Wang D, Wang Y, et al. Comparative study of pathogen detection methods for central nervous system infections: laboratory testing of tuberculous meningitis. BMC infectious diseases, 2024; 24(1): 1172.
- World Health Organization. WHO operational handbook on tuberculosis. Module 1: prevention-tuberculosis preventive treatment. World Health Organization, 2024.

