Unusual Hematologic Presentations: Priapism in Chronic Myeloid Leukemia
Hamza Khan1,*, Muhammad Younas Sujra2, Rashid Ashraf2, Muhammad Hammad Razzaq2 and Zunaira Aamir3*
1Senior Registrar, Haematology department, Indus Hospital & Health Network, Karachi, Pakistan
2Bahria University Health Sciences Campus, Karachi, Pakistan
3Consultant Clinical Haematologist, Indus Hospital & Health Network, Karachi, Pakistan
Received Date: 07/04/2025; Published Date: 28/05/2025
*Corresponding author: Dr. Hamza Khan, Senior Registrar Haematology, Indus Hospital & Health Network, Karachi, Pakistan
Abstract
Priapism is a prolonged penile erection lasting for more than 4 hours without any sexual stimulus. Due to different treatment modalities for different types of priapism, it’s crucial to identify and classify the type prior to initiation of therapy. Chronic Myeloid Leukemia (CML) patients usually present in the out-patient-department (OPD) with symptoms of weakness and abdominal distension. Priapism is a rare presentation of CML which occurs due to hyperviscosity and leukocytosis, causing the patient to land in Emergency Room (ER). We present a case of an 18-years-old male patient, having no known co-morbid, presented in ER with urinary hesitancy and burning micturition for 3 days. On examination there was palpable spleen and priapism, and rest of the systemic examination was unremarkable. CBC reported hyper leucocytosis with absolute basophilia. PCR and karyotype were positive for BCR::ABL fusion gene and Philadelphia chromosome respectively and treatment was started. Bone marrow biopsy was performed and he was diagnosed as chronic phase CML. He is currently on follow-up and show hematological as well as molecular recovery. This case shows importance of recognizing priapism as an initial manifestation of CML. Early diagnosis and management can significantly improve outcomes and prevent erectile dysfunction.
Keywords: Priapism; Chronic Myeloid Leukemia; Hyper leucocytosis; Hyper viscosity
Introduction
Priapism is a prolonged penile erection lasting for more than 4 hours without any sexual stimulus. Generally, it is classified into three main types; arterial (non ischemic), venous (ischemic) and stuttering (intermittent). Veno-occlusive is the most common among all and accounts for about 90-95% of the cases. Due to different treatment options for different types of priapism, it’s crucial to identify and classify the type prior to initiation of therapy [1]. 60% of the priapism cases are idiopathic with no clear cause, while 40% of the cases are related to leukemia, sickle cell anemia, penile trauma, spinal cord trauma, use of certain medications (trazodone, alcohol, psychotropic agents etc) or after intra-cavernous injection of vasoactive agents such as papaverine and phentolamine [2]. Priapism resulting from a hematologic malignancy is most likely caused by venous obstruction from micro emboli and hyperviscosity caused by increased number of leukocytes or malignant cells [1]. It is a urological emergency requiring an immediate intervention to prevent long-term complications, particularly erectile dysfunction [1]. It is a rare presentation of chronic myeloid leukemia (CML) [3]. Here we report a case of an 18-year-old CML patient who presented with priapism as the initial clinical manifestation
Case Presentation
An 18-years-old male patient, unmarried, with no known co-morbids, presented in ER with complaints of urinary hesitancy and burning micturition for 3 days. General physical examination revealed abdominal distention with palpable spleen and priapism, rest of the systemic examinations were unremarkable. Patient was vitally stable and well oriented to time, place and person. CBC reported Hb of 7.6 g/dl, WBC count of 457.6 x 10^9/L and Platelet count of 111 x 10^9/L, so there was hyperleucocytosis and bicytopenia. Differential count showed 48% neutrophils, 6% lymphocytes, 5% metamyelocytes, 29% myelocytes, 5% basophils, 4% eosniophils, 2% monocytes 1% blasts and 6 NRBCs per 100 WBCs. Basophilia was present with absolute count of 22.9 x 10^9/L. The presenting complain of priapism was attributed to hyperviscosity secondary to hyperleucocytosis. Ultrasound abdomen showed mildly enlarged liver with size of 16.9 cm having normal parenchymal echotexture. Spleen was bulky and enlarged having span of 17.1 cm. Ultrasound testes revealed right-sided epididymitis with reactionary minimal septated hydrocele and scrotal wall thickening. Ultrasound KUB (Kidney Ureter Bladder) was unremarkable. Serum electrolytes were normal. Urology team was taken on board, they catheterized the patient and symptomatic management was given. As the CBC and peripheral smear findings were suggestive of chronic myeloproliferative process, PCR was done to look for and if present, quantify BCR/ABL1 gene fusion transcripts, and it reported 50.55% positivity, thus the patient was diagnosed as CML. Karyotype was performed to screen for additional chromosomal abnormalities and it showed presence of Philadelphia chromosome as the single anomaly. His LDH was markedly raised (1428 U/L), uric acid was marginally increased (9.0 mg/dl) while LFTs, urea and creatinine were normal. Bone marrow biopsy was then performed for the confirmation of phase of disease. Aspirate showed myeloid hyperplasia (myeloid to erythroid ratio was 8:1) and 2% blasts. Trephine revealed hyper cellular marrow with 95-100% cellularity, exhibiting myeloid hyperplasia, prominent dwarf-sized megakaryocytes with no evidence of focus of blasts. Hence the case was concluded as chronic phase CML as per the WHO Classification 2022 criteria.
Patient was prescribed 1st line TKI (Imatinib) PO 400 mg OD, along with iron supplement (PO FeSO4 200 mg BD) and Allopurinol PO 300 mg OD. Three months later, PCR for BCR/ABL quantification was repeated to assess treatment response and it reported 16.64% positivity, after which the dose of Imatinib was increased to 600 mg OD, as the optimum response which is less than 10% BCR/ABL transcripts could not be achieved. During this time period, patient was asymptomatic. Follow up CBCs reported progressive improvement in hemoglobin and decline in WBC count. However, platelets initially recovered but again showed a fall in count. Patient was continued with the same medicines. PCR quantification after a further 3 months reported 0.65% positivity, consistent with optimum response. Patient remained asymptomatic. Repeat PCR after a further 6 months (i.e., 1 year after treatment initiation) reported 0.66% positive, thus the major molecular response (MMR) could not be achieved. Patient is being continued with the same treatment, so far, he has been asymptomatic with no treatment related side effects. Platelet count also increased and is now normal. His latest CBC reported Hb of 12.6 g/dl, WBC count of 6.20 x 10^9/L and platelet count of 217 x 10^9/L.
Discussion
Priapism is defined as an erection that persists for more than four hours without sexual stimulation. Priapism can occur at any age but it has a bimodal age distribution, one peak is noted at 5-10 years and second peak tends to occurs in 20-50 years of age [4]. The occurrence of priapism as a first presentation of CML is described in very few case reports. It occurs in 1-2% of male patients with CML. Priapism is classified into two types: ischemic and non-ischemic. Ischemic priapism (low-flow) is the most common subtype and it is a urological emergency caused by venous stasis, while non-ischemic priapism (high-flow), results from arterial flow dysregulation. Identification of the specific subtype is essential for the appropriate management [1]. A complete history, physical examination, Doppler ultrasonography and intra-cavernosal blood gas analysis are helpful to delineate the subtype. On the basis of blood gas values Ischemic priapism shows pO2 <30 mmHg, pCO2 >60 mmHg and a pH of < 7.25. While non-ischemic type shows pO2 >40 mmHg, pCO2 between 40–50 mmHg and a pH ranging from 7.35 to 7.40 [5].
A comparison is given below, summarizing case reports where priapism was the main presentation leading to the diagnosis of CML, along with the different treatment options offered:
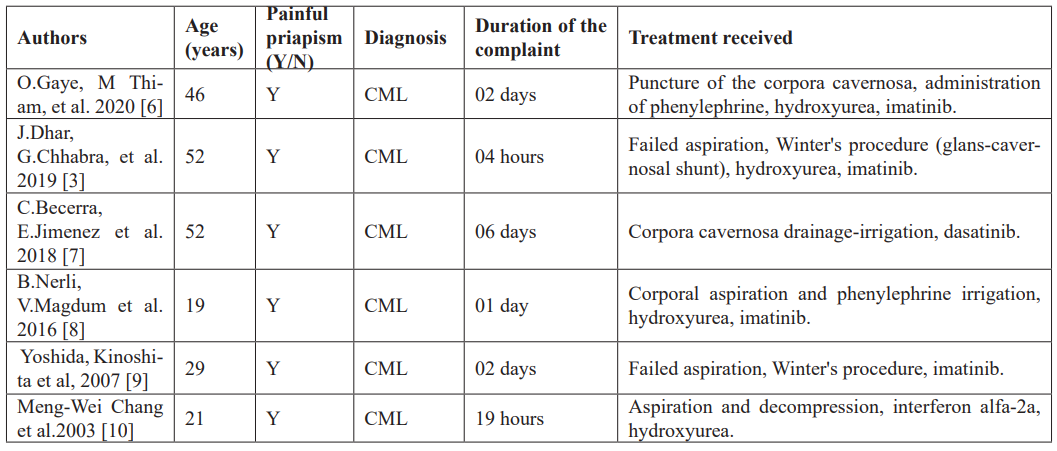
Because the number of reported cases of priapism in patients with CML is relatively small, so there is no standardized treatment protocol. However, the American Urological Association has published practice guidelines recommending the combined use of systemic cytoreductive therapy and local cavernosal decompression for CML to preserve erectile function, based on expert panel discussion and review of the limited available data [1]. Systemic treatment includes (hydroxyurea and analgesia), hydration and TKI (on confirmation of CML). Apart from systemic management, penile aspiration, instillation of sympathomimetic drugs such as phenylephrine and penile shunt procedures are also helpful in bringing down the penile swelling [11]. Some case reports have described the use of non-evidence-based interventions in the management of priapism. For example, Megan et al. reported a case involving a 20-year-old patient in which priapism was successfully resolved through localized penile radiotherapy, after conventional treatments like aspiration and phenylephrine injections [12]. Similarly, Gupta et al. presented a case of a 12-year-old boy who experienced intermittent priapism for 2 weeks, which became persistent in the last 48 hours. This condition was successfully resolved following the TKI in conjunction with subcutaneous administration of terbutaline [13].
Conclusion
This case report highlights an unusual presentation of chronic myeloid leukemia (CML) manifesting as priapism, underscoring the importance of considering hematological disorders in patients presenting with this condition. Our findings suggest that priapism may serve as an early indicator of underlying systemic pathology, prompting further investigation into hematological malignancies. Awareness of such atypical manifestations is crucial for timely diagnosis and intervention, which may significantly impact patient outcomes. Continued research and clinical vigilance are essential to better understand the complex relationship between CML and rare presentations such as priapism.
References
- Abd El Salam M, Ibrahim N, Hassan S. Discontinuation of treatment in a chronic myeloid leukemia patient caused priapism: A case report. Hum Androl, 2019; 9(1): 21–23.
- Gani A, Jailani M. Priapism in Patients Chronic Myeloid Leukemia. Budapest Int Res Exact Sci J, 2020; 2(4): 443–451.
- Dhar J, Chhabra G, Khandelwal L, Batra A, Gupta N. Priapism as a debut presentation of chronic myeloid leukemia. J Coll Physicians Surg Pakistan, 2019; 29(1): 78–80.
- Amalia Y, Notopuro PB. Priapism on Chronic Myeloid Leukemia with BCR-ABL1 Fusion gene Identified by Molecular Test: A Case Report. Res J Pharm Technol, 2023; 16(5): 2229–2232.
- Zahid M. Acute Priapism as a First Manifestation of Chronic Phase CML; A Case Report, 2023; 3(2): 104–106.
- Gaye O, Thiam NM, Cassell A, Gueye SM, Sow Y, Fall B, et al. Unusual Presentation of Priapism Associated with Acute and Chronic Myeloid Leukemia in Two Patients: Emergency Management. Case Rep Urol, 2020; 2020(Figure 1): 1–5.
- Becerra-Pedraza LC, Jiménez-Martínez LE, Peña-Morfin I, Nava-Esquivel R, Villegas-Martínez JA. Priapism as the initial sign in hematologic disease: Case report and literature review. Int J Surg Case Rep, 2018; 43: 13–17.
- Nerli RB, Magdum PV, Hiremath SC, Patil AY, Pai S V, Handigund RS, et al. Priapism - A Rare Presentation in Chronic Myeloid Leukemia: Case Report. Urol Case Reports, 2016; 4: 8–10.
- Chang MW, Tang CC, Chang SS. Priapism - A rare presentation in chronic myeloid leukemia: Case report and review of the literature. Chang Gung Med J, 2003; 26(4): 288–292.
- Mishra K, Jandial A, Singh V, Radotra B, Malhotra P. Priapism in chronic myeloid leukemia: Meeting at the crossroads and heading in different directions. Indian J Med Paediatr Oncol, 2020; 41(3): 418–420.
- Manuel MB, Leak A, Carroll SA. Priapism in the oncology setting. Clin J Oncol Nurs, 2007; 11(1): 23–25.
- Gupta A, Seth T, Gupta A. Successful use of terbutaline in persistent priapism in a 12-year-old boy with chronic myeloid leukemia. Pediatr Hematol Oncol, 2009; 26(1): 70–73.

