Obstructive Phytobezoar of the Small Bowel: Surgical Treatment Without Enterotomy
Abdelhak Ettaoussi, Malik Zarhouni Baallal*, Aziz Moussahim, A. EL Bakouri and Khalid El Hattabi
Department of Visceral Surgery, Ibn Rochd University Hospital, Hassane II University, Faculty of Medicine and Pharmacy (FMPC), Casablanca Morocco
Received Date: 02/04/2025; Published Date: 23/05/2025
*Corresponding author: Zarhouni Baallal Malik, Department of Visceral Surgery, Ibn Rochd University Hospital, Hassane II University, Faculty of Medicine and Pharmacy (FMPC), Casablanca, Morocco
Abstract
Intestinal bezoars are a rare cause of obstruction. Their treatment is surgical and consists of extraction by enterotomy.
We report a case of small bowel obstruction on a phytobezoar treated by manual expression. The patient was 19 years old and had no previous medical or surgical history. He was admitted with an acute intestinal obstruction.
An unprepared abdominal X-ray revealed hydroaeric levels in the small intestine.
Abdominal and pelvic CT showed significant distension of the small intestines with hydroaerosal levels in favour of an occlusive syndrome with a transitional zone at the level of the last ileal loop. Biological tests were normal.
Surgical exploration revealed an obstructive phytobezoar of the small bowel, which was treated by manual expression without enterotomy, a moderate peritoneal effusion of ascites fluid, and a catarrhal appendix in the mesocoeliac position.
Keywords: Intestinal obstruction; Phytobezoar; Appendicitis; Oxyurosis
Introduction
Phytobezoar is a concretion of ingested plant substances stagnating in the digestive tract.
It is a rare cause of intestinal obstruction. Surgical treatment is an enterotomy which may increase morbidity. We report a case treated surgically by manual expression without enterotomy. The aim of this article was to discuss the indications for treatment.
Observation
A 19-year-old patient with no specific medical or surgical history was admitted to the Intake Department of Casablanca University Hospital with abdominal pain that had been progressing for three days, of progressive intensity, with infrequent stools and gas and no vomiting. There was no evidence of fever. On admission, the patient's blood pressure was 120/70 mmHg, pulse 92 beats per minute, and temperature 36°C8. On physical examination, the mucous membranes were well stained. The abdomen was slightly distended with generalized tenderness predominating in the right iliac fossa. On rectal examination, the blister contained faces.
The rest of the physical examination was normal. A complete blood count (CBC) showed white blood cells at 8,560 cells per mm3, haematocrit at 17.5 cells per mm3, and platelets at 303,000 cells. A frontal unprepared abdomen X-ray (APX) revealed hydroaeric levels (HAL) in the small intestine. Abdominal and pelvic CT showed significant distension of the small intestines with hydroaerosal levels in favour of an occlusive syndrome with a transitional zone at the level of the last ileal loop (Figure 1).
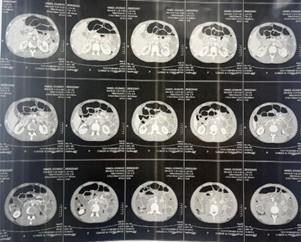
Figure 1: Occlusive syndrome with a transitional zone.
In view of this occlusive syndrome, we admitted the patient to hospital, administered parenteral fluid and electrolytes, performed a urinary catheterisation, inserted a nasogastric tube and administered parenteral paracetamol for analgesia.
Surgical exploration by median laparotomy above and below the umbilicus revealed a moderate peritoneal effusion of ascites fluid (removed and evacuated). There was a 3 cm distension of the small intestine upstream of a transition zone 4 m from the ADJ and 1.10 m from the JIC (Figure 2). The site of a mechanical obstruction (hard food) (Figure 3).
Catarrhal appendix in mesocoeliac position (Figure 4).

Figure 2: Small intestine upstream of a transition zone.

Figure 3: Mechanical obstruction (hard food).
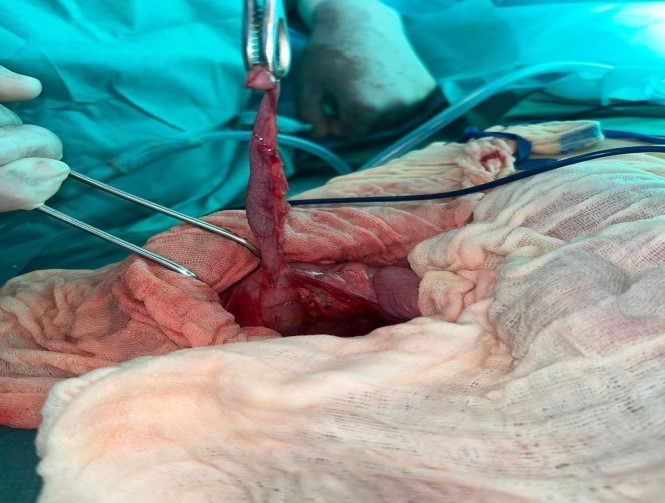
Figure 4: Catarrhal appendix in mesocoeliac position.
The rest of the examination was unremarkable.
We performed manual expression without opening the small bowel. The intra-intestinal bezoar was held between the pulp of the five fingers of the right hand on the proximal side of the bezoar and we applied gradual and repeated manual pressure.
The distal portion of the loop was held by the left hand to monitor the progression of the bezoar through the valve of Bauhin valve.
The same manoeuvre was performed on the colon until the bezoar was extracted through the anus.
It was a phytobezoar, friable, mobilisable, weighing about 20g and made up of fig peel; we had also carried out a retrograde appendectomy.
The post-operative course was straightforward and the patient was discharged on the fourth post-operative day.
Pathological examination of the appendix revealed acute suppurative pan-appendicitis with oxyurosis, no signs of malignancy, hematic and inflammatory ascites fluid with no cells suspected of malignancy. The patient was prescribed albendazole-based medical treatment for pinworm infection. At six months, there was no recurrence and his physical examination was normal.
Discussion
The prevalence of bezoar occlusions is estimated at 2-3%, and phytobezoars are the most common, accounting for 80% of all occlusions [1]. Occlusions in the oesophagus are rare and those in the colon exceptional. The treatment of phytobezoars, although poorly codified, is essentially surgical. The aim is to extract the bezoar but also to avoid complications and recurrences [1]. In our patient, we extracted the bezoar after manual expression by laparotomy. Given its advantages over laparotomy, laparoscopy is the best means of exploration [2]. However, it can be difficult to express the bezoar in this way, as there is a loss of manual contact. In our patient, we performed extraction by manual expression because the phytobezoar was friable, not adherent to the walls of the small intestine and close to the cecum. This manoeuvre is easy in these circumstances. The most commonly performed therapeutic procedure is an enterotomy [1].
But for many patients, the phytobezoar is easily fragmented and evacuated by manual expression without enterotomy. Enterotomy may be indicated only if the bezoar cannot be fragmented and adheres to the intestinal walls. Resection is rarely performed and may be reserved for cases of intestinal necrosis or complication. This manual extraction manoeuvre can lead to erosion of the intestinal mucosa, ulceration, haemorrhage or perforation, complications which we did not observe in our patient. The closer the bezoar is to the ileo-caecal valve, the easier it is for the surgeon to fragment it and evacuate it manually to the cecum. This technique avoids the need for an enterotomy, which carries an increased risk of postoperative morbidity. Some authors have attempted medical treatment with chemical dissolution of the phytobezoar using acetylcysteine, papain or cellulose. However, the results are controversial and there is a risk of bezoar migration [1].
In some cases, the chemical composition of the mass makes medical treatment illusory [3].
Some authors suggest the use of copious drinks combined with transit accelerators, and others, fragmentation either by laser and mini-explosion, or by extracorporeal lithotripsy, especially in adult patients in poor general condition who are unfit for surgery [4].
Endoscopic techniques are mainly used in cases of gastric or duodenal bezoar.
However, attempted extraction by endoscopy may result in failure or severe complications such as pneumomediastinum due to oesophageal fissure because of the size of the bezoar [4].
Endoscopic extraction may be proposed if surgery is contraindicated after an attempt at chemical dissolution. The definitive solution is surgery. Extraction by enterotomy is the most commonly practised, but manual expression has some advantages. In a third of cases, patients present with a recurrence because the favouring factors are still present and patients still maintain their eating habits [3].
Conclusion
Obstructive phytobezoar of the small intestine is a rare condition. Surgical treatment by manual expression is preferable and consists of extraction without enterotomy if the bezoar is friable and does not adhere to the intestinal walls.
References
- Ersoy YE, Ayan F, Ersan Y. Gastro-intestinal bezoars: thirty-five years experience. Acta Chir Belg, 2009; 109: 198-203.
- Kwok Kay Yau, Wing tai Siu, Bonita Ka Bo Law, Hester Yui Shan Cheung, Joe Ping Yiu ha,
Michael ka Wah Li. Laparoscopic approch compared with conventional open approach for bezoar-induced small bowel obstruction. Arch Surg, 2005; 140: 972-975. - Kassé AA, Cherbonnel G, Fall B, Toure P, Diop A. Les phytobézoard : à propos de trois observations.
Dakar Med, 1984; 20: 460-476. - Chellat H, Amrani L, Hrona A, Amrani N. Trichobézoard gastrique: a propos d’un cas. Acta Endosc, 2011; 41: 8-10.

