Spontaneous Cervical Epidural Hematoma of Idiopathic Etiology: A Case Report
Nabil Nia*, Oualid Mohammed Hmamouche, Marouane Hammoud, Fayçal Lakhdar, Mohammed Benzagmout, Khalid Chakour and Mohammed El Faiz Chaoui
Department of Neurosurgery, Hassan II University Hospital, Morocco
Received Date: 08/04/2025; Published Date: 19/05/2025
*Corresponding author: Nia Nabil, Department of Neurosurgery, Hassan II University Hospital, Fez, Morocco
Abstract
The Spontaneous Spinal Epidural Hematoma (SSEH) is a rare case characterized by the occurrence of blood effusion in the epidural space without any trauma. It is a serious pathology for which rapid positive diagnosis is essential to preserve the functional and potentially the vital prognosis.
Keywords: The Spontaneous; Epidural Hematoma; MRI
Introduction
The Spontaneous spinal epidural hematoma (SSEH) is defined as an epidural hematoma that has no known etiological reason [1]. Although arteriovenous malformations, tumors, trauma, or postoperative complications are attributed to cause this disease, the most common site of SSEH is the cervicothoracic region [2]. Patients with SSEH typically present acute severe back pain and signs of either fast progression to the spinal cord, or of the compression of cauda equina [4]. The MRI is considered the modality of choice for diagnosis [3]. The most effective treatment consists of a rapid decompressive laminectomy and the evacuation of the hematoma [5]. The prognosis of SSEH is closely related to the level and size of the hematoma, the degree of preoperative neurological deficit, and the time between symptoms onset and surgery [6].
Case Presentation
We report the case of a 10-year-old child admitted to the emergency room for cervical pain, aggravated by the heaviness of the 4 limbs of sudden onset for 02 days, mainly in the crural region. There was no recent medical history of trauma, infection, surgery, or use of anticoagulants. The initial lab tests, such as routine blood tests, liver function tests, blood creatinine, electrolytes, activated partial thromboplastin time, and international normalized ratio, were within normal limits.
Neurologic exam: This examination showed that standing and walking were impossible, with tetraparesis rated 0/5 in the two lower limbs, a deficit in elbow extension of the two upper limbs rated 2/5, hypoesthesia, and a sub- nipple sensory level, and the osteotendinous reflex was abolished with an indifferent Babinski.
Imagery: Spinal MRI showed a posterior epidural hematoma spread from C4 to D1, strongly compressing the spinal cord. The hemostasis tests were normal (Figure 1).
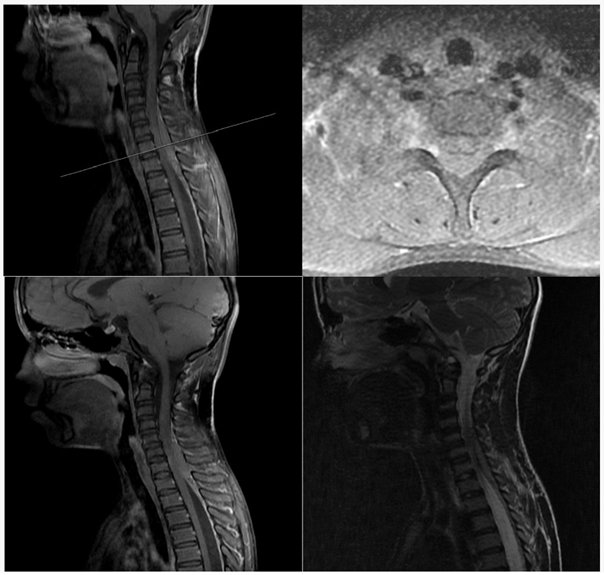
Figure 1: MRI of spinal cord showing the extradural hematoma compressing and dis-placing the spinal cord.
Surgery procedure: The patient underwent a posterior C5-C7 laminotomy, with evacuation of the epidural hematoma; The intraoperative exploration, after evacuation of the hematoma, did not reveal any malformative or tumoral abnormalities; the pathological study confirmed no evidence of vascular malformation or neoplasm.
Discussion
SSEH is a rare neurosurgical pathology with an estimated incidence of 0.1 per 100,000 individuals [7]; it is considered a surgical emergency [8]. The etiology is unknown, but it is generally accepted that most of these hematomas arise from a rupture of the epidural venous plexus [9]. A second theory links the bleeding from the free epidural anastomotic arteries to the radicular arteries of the cervical spine [10,11]. As the case of our patient, the majority of SSEH’s are located in the C6/7 region, a very mobile segment of the spine, and it is believed that certain movements at this level could stretch the free arteries beyond their limits of tolerance, causing them to break up. The most common presentation is acute pain and radicular symptoms similar to those of a herniated disc. Depending on the severity and speed of the bleeding, neurological symptoms can progress quickly. Also, there is no significant correlation with age, race, or gender, and there is disagreement in the literature as to the most common location on the spine. The MRI is the diagnostic modality of choice. During the first 24 hours, the hematoma generally appears isointense at the cord level on T1WI and hyperintense and heterogeneous on T2WI. Then, the hematoma usually becomes hyperintense on T1WI and T2WI over the next 48 hours. Chronic hematomas appear hypointense on both T1WI and T2WI [12-14].
The radiological differential diagnoses include the epidural abscess and the spinal epidural lymphoma [15].
An urgent surgical intervention by posterior laminectomy and evacuation of the epidural hematoma is justified within 12 to 48 hours following the appearance of symptoms [16-18]. Our patient benefited from a cervical laminotomy with evacuation of the epidural hematoma.
The outcomes are generally poor without a surgical intervention [19]. The prognosis is primarily based on pre-operative neurological status, where patients with residual neurological function at admission have a better prognosis [15,8]. The non-surgical management is reserved only for asymptomatic patients, where strict bed rest and serial imaging studies are recommended [17].
Conclusion
The spontaneous spinal hematoma is a pathology with a poor prognosis, responsible for sometimes permanent neurological deficit. The bleeding is most often of venous origin in patients taking anticoagulants or suffering from a coagulopathy. In addition, its management can present some difficulties. The first stage concerns the correction of possible coagulation disorders before surgical evacuation of the hematoma. At last, the functional prognosis essentially depends on the initial neurological deficit, level and extent of the hematoma and on the time elapsed before the intervention.
References
- Beatty RM, Winston KR. Hématome péridural cervical spontané : une considération de l'étiologie, Journal of Neurosurgery, 1984; 61(1): pages 143-148.
- Groen RJM, Goffin J. Traitement non opératoire des hématomes épiduraux rachidiens spontanés: une revue de la littérature et une comparaison avec des cas opératoires. Acta Neurochirurgical, 2004; 146(2): pages 103-110.
- Zeng L, Liu Z, Shen 13 Cas d’hématomes épiduraux rachidiens spontanés aigus Menton. J. Neurol., 2002; 35(2): pages 71-73.
- Groin RJM, Ponssen L’hématome épidural rachidien spontané Une étude de l’étiologie, 1990; 1869: pages 121-138
- LiaoC-C, Hsieh P-C, Lin T-K, Lin C-L, Lo Y-L, Lee S-C. Traitement chirurgical de l'hématome épidural rachidien spontané : une expérience de 5 ans: article clinique », Journal of Neurosurgery: Spine, 2009; 11(4): pages 480-486.
- Liu Z, Jiao Q, Xu J, Wang X, Li S, You C. Hématome épidural rachidien spontané: analyse de 23 cas, Surgical Neurology, 2008; 69(3): pages 253-260.
- BS Baek, JW Hur, KY Kwon et Hématome épidural rachidien spontané J Korean Neurosurg Soc, 2008; 44(1): pp. 40–42.
- Gopalkrishnan CV. Hématome péridural cervical spontané: à propos d’un cas et revue de la littérature Surg. Neurol. Int., 2019; 10(2): p. 113–117.
- Liao C-C, Lee S-T, Hsu W-C, Chen L-R, Lui T-N, Lee S-C. Expérience dans la prise en charge chirurgicale de l'hématome épidural rachidien spontané. Journal of Neurosurgery, 2004; 100(1): 38- 45.
- Gopalkrishnan CV. Hématome péridural cervical spontané : à propos d’un cas et revue de la littérature Surg. Neurol. Int., 2019; 10(2): p. 113 – 117.
- Alves JL, Santiago JG, Costa G, et Une classification standardisée des hématomes sous-duraux- I Suis. J. Méd. médico-légal. Pathol, 2016; 37(3): pages 174-178.
- Abascal F, Pinto JI, Figols FJ, et Rapport de cas Hématome épidural rachidien chronique non traumatique de la colonne lombaire : diagnostic IRM, 2000; 1605: pages 1602-1605.
- Avrahami E, Tadmor R, Ram Z, et Démonstration par IRM d'un hématome épidural aigu spontané du rachis thoracique Neuroradiologie, 1989; 31(1): pp. 89–92.
- Al-Mutair A, Bednar DA. Hématome épidural rachidien Confiture. Orthop. Surg., 2010; 18(8): pages 494-502.
- Gala FB, Aswani Y, Center LI, et Imagerie des lésions de l'espace épidural postérieur de la colonne vertébrale : un essai illustré, 2016; 26: pages 299-315.
- Bhat KJ, Kapoor S, Watali YZ, et a Hématome épidural spontané du rachis associé au clopidogrel: étude de cas et revue de la littérature Asiatique J Neurochirurgie, 2015; 10(1): p. 54.
- Rajz G, Cohen JE, Harnof S, et Hématome épidural rachidien spontané : importance de l'état neurologique préopératoire et d'une intervention rapide J. Clin. Neurosci. : journal officiel de la Société Neurochirurgicale d’Australasie, 2015; 22(1): pp. 123-128.
- Zhong W, Chen H, You C, et al. Hématome épidural rachidien spontané J. Neurosci., 2011; 18(11): pages 1490-1494.
- Iwatsuki K, Deguchi M, Hirata H, et Hématome épidural cervical récurrent résolu spontanément chez une primigeste de 37 semaines Global Spine J., 2015; 5(5).

