Pyelo-Ureteric Junction Obstruction Revealed by Urinoma: A Case Report
Nachid A*, Safwate R, Hannaoui A, Tmiri A, Kbirou A, Moataz A, Dakir M, Debbagh A and Aboutaieb R
Department of Urology, CHU IBN Rochd, Casablanca, Morocco
Received Date: 19/03/2025; Published Date: 16/05/2025
*Corresponding author: Nachid A, Department of Urology, CHU IBN Rochd, Casablanca, Morocco
Abstract
Ureteropelvic Junction (UPJ) obstruction is a congenital or acquired condition that can remain asymptomatic until adulthood. We report the case of a 57-year-old man who presented with flank pain and was found to have a urinoma on imaging studies. Further evaluation revealed a UPJ obstruction as the underlying cause, associated with early renal failure evidenced by elevated serum creatinine. The patient underwent appropriate urological management with favorable postoperative outcomes. This case highlights the importance of considering UPJ obstruction in adults presenting with urinoma and impaired renal function.
Keywords: Pyelo-Ureteric Junction (PUJ); Obstruction; Pyeloplasty
Introduction
Pyelo-Ureteric Junction Obstruction (PUJ-O) syndrome corresponds to a defect of urine flow between the pyelon and the proximal portion of the lumbar ureter, whose obstruction is functional in more than half of the cases, it may be secondary to a compression of the ureter, inflammation, retroperitoneal fibrosis, kidney stones, or scar tissue from previous surgery.
PUJ-O can be revealed mostly by intermittent lumbar pain or be completely asymptomatic and discovered incidentally during an imaging test.
Whatever the cause, the effect of the obstruction is the same and can lead, in some cases, to complications (pyelonephritis, lithiasis and in rare case urinoma) that may affect the fate of the kidney [1].
Here we report the case of a 57 years old man who presented with acute pyelonephritis and onset of an early renal insufficiency on a pyelo-ureteric junction syndrome which is rare form of revelation.
Medical Observation
A 57-years-old man with no significant medical history presented to the emergency department with persistent left lumbar pain for 15 days, despite treatment, associated with burning sensation during urination, pollakiuria and feverish sensation, with no history of passing stones or sand in urine nor notion of trauma.
On physical examination, the patient had a left lumbar sensibility, fever at 38,9 and a 30cc prostate on rectal examination without nodules, painless to touch.
Blood tests revealed leukocytosis with a count of 24.09 x 10^3/µL with 91.8% neutrophils, platelets count of 174 x 10^3/µL, C-reactive protein level of 603mg/L, plasma urea and creatinine levels of 0.67g/L and 17.5 mg/L respectively (eGFR: 41mL/min/1,73m2), and potassium level of 5.1 mmol/L. The urine culture revealed a pH of 6, with 500 white blood cells/mm^3, 30 red blood cells/mm^3, and a few gram-negative bacilli seen on microscopy.
Injected abdominal-pelvic computed tomography scan showed a major left ureterohydronephrosis likely due to pyelo-ureteric junction syndrome associated with a left perirenal fluid collection continuous with the urinary tract (Figure 1).
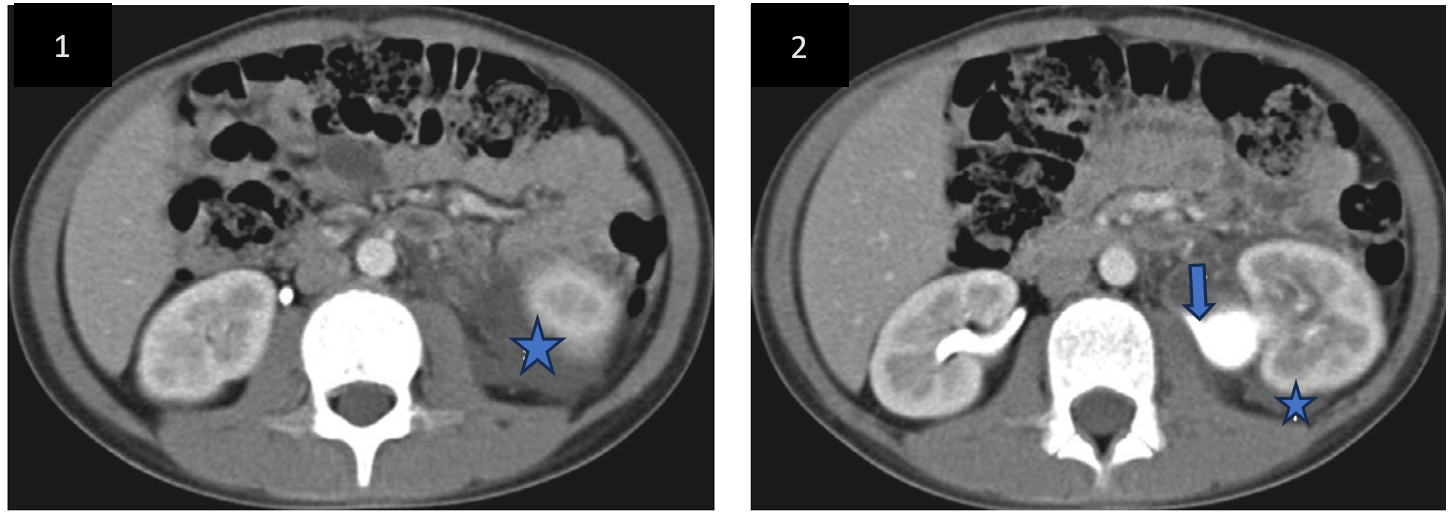
Figure 1: CT urogram showing ureteropelvic junction obstruction (inverted arrow) and perirenal fluid collection (asterisk).
The patient underwent a double J stent (MDS jj) and a urethral catheterization with cloudy urine. Antibiotic therapy with third-generation cephalosporin and amikacin was given (based on eGFR). The clinical course was marked by persistent fever and lumbar pain, leading to a second uro-CT scan after an external drainage by nephrostomy. The imaging revealed a complicated pyelonephritis with pre- and retroperitoneal infectious collections involving the proximal ends of the double J stent and nephrostomy tube in place.
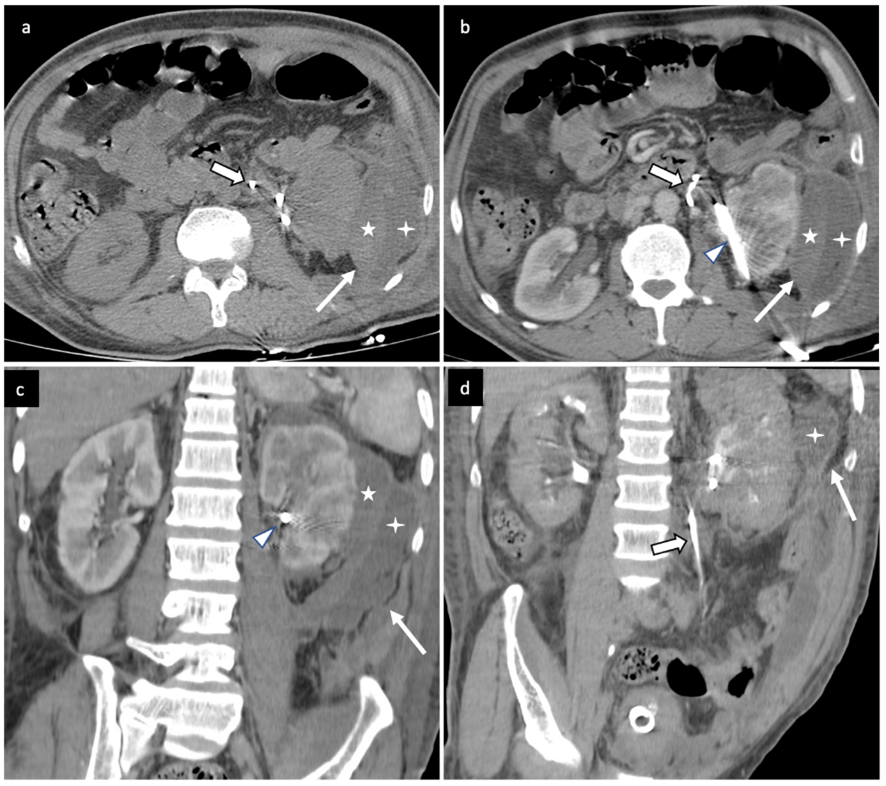
Figure 2: Computerized Tomography (CT) urogram with axial section in spontaneous contrast (a), axial and coronal oblique sections at nephrographic time (b and c) and coronal oblique section at excretory time (d); heterodense left perirenal collection (arrow) with a spontaneously dense portion (star) and an area of liquid density (asterisk) in connection with a hemato-urinoma. Nephrostomy tube (arrowhead) and JJ tube (solid arrow).
The progression was marked by apyrexia on day 1 post-nephrostomy, regression of the lumbar pain, and a decrease in C-reactive protein to 54 mg/L compared to 603 mg/L, creatinine at 9 mg/L compared to 47.5 mg/L, and white blood cells at 9,870 compared to 24,090.
Discussion
Urinoma is defined as an encapsulated collection of urine in the perirenal or periureteral space, due to a sudden increase in pressure in these spaces, the rupture occurs at the fornix or proximal ureter respectively [2] and can be of traumatic, lithiasic or iatrogenic origin and exceptionally due to a malformative uropathies [3].
Most common malformative uropathy in urinoma is posterior urethra valve in 70% of cases, whose functional prognosis is better than PUJ-O [4,5].
The constellation of good renal contrast excretion with extravasation of contrast into the medial perirenal space with an intact calyceal system and non-visualization of the unilateral ureter is virtually diagnostic of complete or partial UPJ disruption [6].
Our patient had no urological or surgical history, this peri-renal collection may be due to an increase in pressure in the renal sinus, hence its rupture with no history of trauma, although this explanation remains unclear due to the impossibility of performing an injected CT scan on admission because of the acute renal failure, which was confirmed after the percutaneous nephrostomy.
More than 90% of urinomas secondary to obstructive malformative uropathy respond to percutaneous shunting which removes the obstruction [2].
A pyeloplasty can be performed if the radiological control allows to link the appearance of the dilatation or its absence with the appearance or not of symptoms to avoid any recurrence [2].
In our case, the evolution was favorable clinically and biologically after the external drainage, he will be scheduled for a pyeloplasty to avoid any recurrence.
Conclusion
PUJ-O Syndrome is most often revealed by lumbar or abdominal pain, rarely by complications and exceptionally by urinoma following spontaneous rupture.
There are few cases in the literature describing the revelation of this syndrome by a spontaneous urinoma in adults and children.
Diagnosis confirmation is based on CT urogram that shows extravasation of contrast in the perirenal space with a non-dilated ureter.
Emergency treatment is based on external drainage combined with antibiotic, followed by pyeloplasty to correct the malformation and prevent recurrence.
Fundings: none
Conflict of interest: none
References
- McKnoulty M, Green A, Scott S, Roberts MJ, Kothari A. Spontaneous renal fornix rupture in pregnancy and the post partum period: a systematic review of outcomes and management. BMC Urol, 2020; 20(1): 116.
- Tseng PC, Liu TY, Pan SJ, Sung DS. Spontaneous Perirenal Urinoma Associated with Ureteropelvic Junction Obstruction in a Child: A Case Report. Pediatr Neonatol, 2009; 50(3): 121‑124.
- Tsai JD, Huang FY, Lin CC, Tsai TC, Lee HC, Sheu JC, et al. Intermittent Hydronephrosis Secondary to Ureteropelvic Junction Obstruction: Clinical and Imaging Features. Pediatrics, 2006; 117(1): 139‑146.
- Throff JW, Brzezinska R, Beetz R, Stein R, Rohatsch P. Acute perirenal extravasation of urine in an infant with non-refluxing megaureter. Pediatr Nephrol, 2004; 19(3): 357‑360.
- Stathopoulos L, Merrot T, Chaumoître K, Bretelle F, Michel F, Alessandrini P. Prenatal Urinoma Related to Ureteropelvic Junction Obstruction: Poor Prognosis of the Affected Kidney. Urology, 2010; 76(1): 190‑194.
- Kawashima A, Sandler CM, Corriere JN Jr, et al. Ureteropelvic junction injuries secondary to blunt abdominal trauma. Radiology, 1997; 205: 487–492.

