Scopulariopsis Brain Infection in a 5 Years Old Child with Pre-B Acute Lymphoblastic Leukemia
Sajjad Ali*, Aun Raza, Salma Abbas and Summiya Nizamuddin
Shaukat Khanum Memorial Cancer Hospital and Research Center, Pakistan
Received Date: 09/04/2025; Published Date: 15/05/2025
*Corresponding author: Sajjad Ali, Shaukat Khanum Memorial Cancer Hospital and Research Center, Pakistan
Abstract
Background: Scopulariopsis species are environmental fungi that rarely cause human infections. However, in immunocompromised patients, they can lead to invasive, life-threatening diseases with challenging management. Scopulariopsis brevicaulis has been implicated in deep fungal infections, but detailed information on its pathogenesis remains limited. Pulmonary and disseminated infections are the most common clinical manifestations, often requiring prolonged antifungal therapy.
Case Presentation: We report a rare case of Scopulariopsis brain infection in a paediatric patient with pre-B acute lymphoblastic leukemia (ALL). The patient developed persistent fever and neurological symptoms, prompting imaging studies that revealed enhancing brain lesions. Despite negative bacterial and mycobacterial cultures, fungal culture and microscopy of brain tissue confirmed Scopulariopsis species. The patient was treated with voriconazole, demonstrating a favourable clinical and radiological response.
Conclusion: This case report emphasizes the importance of vigilance and prompt diagnosis in managing opportunistic infections in immunocompromised patients. Fungal infection (Scopulariopsis) should be considered in the differential diagnosis of CNS infections in patients with underlying malignancies and immunosuppression. Species identification and minimum inhibitory concentration (MIC) data were not available. Early recognition and treatment with appropriate antifungal agents, such as voriconazole, can significantly improve outcomes in these patients.
Introduction
Scopulariopsis is a common fungus in the environment and it is commonly found on vegetables, animal corpses and other organic waste. It obtains nutrients from dead organic matter. It causes opportunistic infection in humans [1-3]. Scopulariopsis belongs to Microascaceae family. Scopulariopsis brevicaulis is the commonest species reported. Other species include Scopulariopsis acremonium, Scopulariopsis brumptii, Scopulariopsis candida, Microascus trigonosporus, Microascus cinereus [4]. Microscopically, the isolated fungus has hyaline and septate hyphae, finger-like conidiophores on which annelids produced chains of conidia [5]. Surface slide is powdery light brown colonies with a light tan on the periphery and the reverse slide is usually tan with darker brownish center (Figure 4) [6,7].
Although rare, Scopulariopsis brevicaulis can causes invasive fungal infection in humans. Opportunistic fungal have become a significant cause of morbidity and mortality in patients with severe underlying diseases such as malignancy and post bone marrow transplant and impaired host defense capabilities [8]. The most common manifestation is pulmonary and disseminated infection. Infections at other sites such as ear, nose, nails, lung and brain have been reported in immunocompromised patients and those with ongoing substance abuse [6,9]. The exact pathogenesis remains unknown. Treatment remains challenging. Diverse approaches have been described in the literature with varying outcomes [6,7].
Here, we report a rare case of Scopulariopsis brain infection in a paediatric patient with pre-B-acute lymphoblastic leukemia (ALL). To our knowledge, this represents the first documented case of Scopulariopsis affecting the central nervous system in a child. This report highlights the diagnostic challenges, treatment considerations, and the need for further research into optimal management strategies for such rare fungal infections.
Case Report
5 years old female with Pre-B-ALL had been diagnosed in January, 2023. He had been treated with induction chemotherapy with vincristine, peg asparaginase, dexamethasone and intrathecal methotrexate from 2nd February, 2023 to 1st March, 2023 followed by the consolidation chemotherapy with vincristine, intrathecal methotrexate and 6-merceptopurines dated from 11th march, 2023 to 28th March, 2023. She had received interim maintenance chemotherapy with vincristine, dexamethasone, 6-merceptopurines and intrathecal methotrexate from 24th May, 2023 to 21th June 2024. She had delayed intensification chemotherapy with vincristine, doxorubicin, peg asparaginase and 6-merceptopurines, cyclophosphamide, cytarabine and intrathecal methotrexate from 30th July to 14th September, 2023. She was started on maintenance chemotherapy since 26th september, 2023 with 6-merceptopurine, dexamethasone and methotrexate with plans to complete 18 months.
She was admitted for delayed intensification chemotherapy in end of July 2023. She had developed daily fever and blood culture was sent that grew Carbapenem resistant Escherichia coli (E coli) and Candida albicans which was treated with meropenem, colistimethate sodium for E coli bacteremia and initially caspofungin then switched to fluconazole for candidemia.
Later on, she had developed abdominal distention and keeping in view her febrile neutropenia, she underwent Computed Tomography (CT) of chest, abdomen and pelvic which revealed cecal perforation and pulmonary nodules. She had undergone exploratory laparotomy and resection of bowels with ileostomy and Hartmann procedure for cecal perforation on 2nd August, 2023 and treated for presumed fungal pneumonia with voriconazole from 23rd July, 2023 to 11th dec, 2023). Post surgery she had developed fever, pain and discharge at the surgical site. Abdominal wound infection was suspected and culture wound swab sent on 7th August, 2023 grew Enterococcus gallinarum (sensitive to chloramphenicol. linezolid) treated with oral linezolid. She underwent stoma reversal on 12th December, 2023
In April 2024, she was admitted for right abdominopelvic collection and pigtail drain was inserted on 9th April, 2024 by intervention radiology team. Pus culture grew E. coli which was treated with piperacillin/tazobactam. Repeat CT abdomen reported fistulous communication between bowel and collection and so she underwent exploratory laparotomy with retroperitoneal exploration, adhesionolysis, ileal wedge resection and anastomosis, revision of previous anastomotic site with ileocolic anastomosis on 1st May, 2024.
She presented on 15th August 2024 with persistent and continuous fever and headache for 4 days. Patient had no other neurological symptoms such as fits, vision loss and weakness in the limbs. She reported no other symptoms. Clinically, the patient was febrile on arrival, irritable and lethargic but there were no signs of meningism. Abdomen was soft, non-tender with a well healed laparotomy wound. Baselines labs revealed neutropenia from 15th to 18th August, 2024. Initially blood culture and lumbar puncture was not performed. She was initially started on piperacillin/tazobactam from 15th to 18th August 2024 for febrile neutropenia.
Magnetic resonance imaging (MRI) brain (Figure 1) done on 19th August 2024 revealed enhancing nodules centered over surface of left parietal and right occipital area highly concerning for disease involvement vs brain abscesses. She was started on Ceftriaxone, Vancomycin and metronidazole on 19th August 2024.
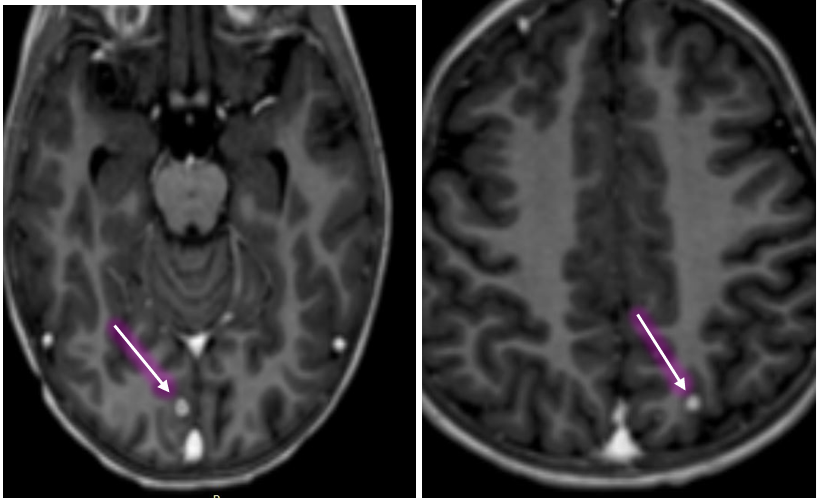
Figure 1: Brain MRI: Post contrast T1- weighted images demonstrates two enhancing nodules each on right occipital cortex and left posterior parietal region.
Cerebrospinal Fluid (CSF) analysis was performed later on 4th September, 2024 which revealed 01 white blood cells (WBC), protein 22.8mg/dl and glucose 48 mg/dl. Her CSF India ink test and meningitic panel including polymerase chain reactions (PCR) for Escherichia coli K1 haemophilus influenzae, listeria monocytogene, neisseria meningitidis, streptococcus agalactiae, streptococcus pneumoniae, cytomegalovirus, enterovirus, herpes simplex virus 1, herpes simplex virus 2, Human herpesvirus 6, Human parechovirus, varicella zoster virus, Cryptococcus neoformans/gattii were negative. She had negative bacterial, fungal and mycobacterial cultures on CSF. Her CSF cytology was negative for malignant cells.
Repeat brain imaging with MRI scan (Figure 2) was done on 20th September, 2024 which showed interval development of new right occipital lobe lesion as well interval increase in size of previous right occipital lobe lesion consistent with disease progression.
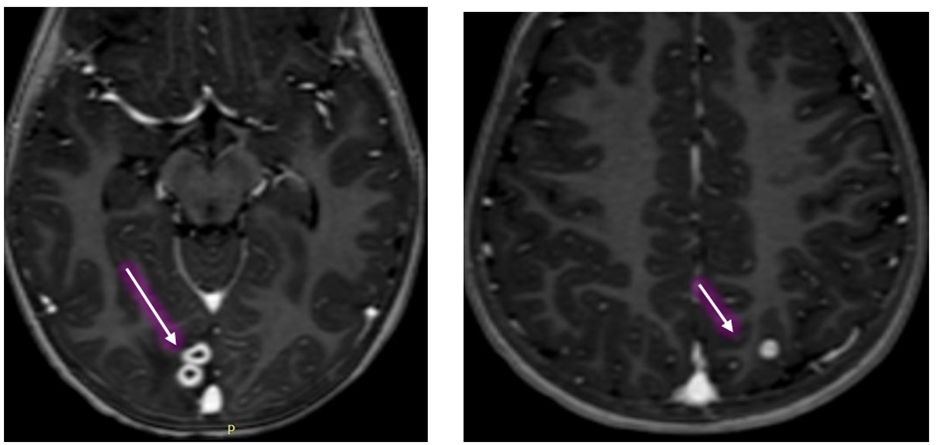
Figure 2: Brain MRI: Post contrast T1- weighted images showed new enhancing cortical based lesion adjacent to previously demonstrated right occipital lobe lesion and left posterior parietal lobe nodule slightly increased in size.
The patient was planned for brain biopsy and neuroavigation guided right occipital craniotomy and resection of the lesion was done 8th October, 2024.
Histopathology (Figure 3) showed glial tissue with reactive gliosis, foci of abscess formation and surrounding vague granulomatous response.
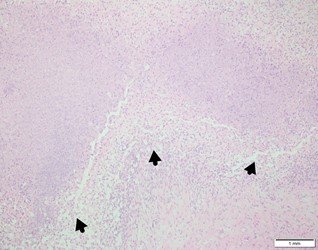
Figure 3: Histopathology: Microscopy revealed glial tissue with abscess formation and epithelioid histiocytes. No definite caseous necrosis seen.
Brain tissue was negative for bacterial culture and her mycobacterial gene Xpert was negative and Mycobacterial culture was not sent on brain tissue. Initial Koh and microscopy were negative fungi in this case. Lactophenol Cotton Blue (LPCB) mount (Figure 4a) of the colony showed hyaline, septate hyphae with conidiophores bearing annellides. Fungal cultures (Figure 4b) later revealed light brown colonies with a tan periphery and dark brown reverse coloration.
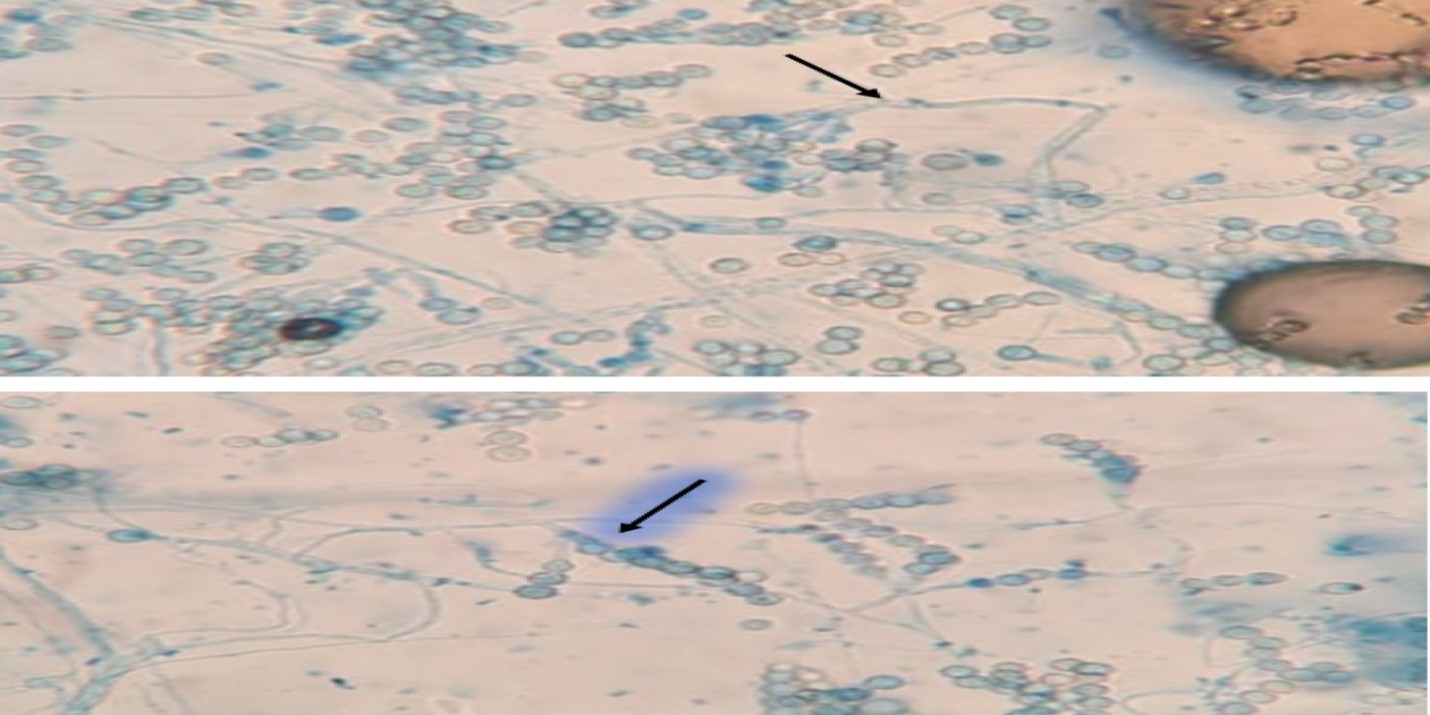
Figure 4a: Microscopy and Culture: LPCB mount of the colony showed hyaline, septate hyphae with conidiophores bearing annellides.
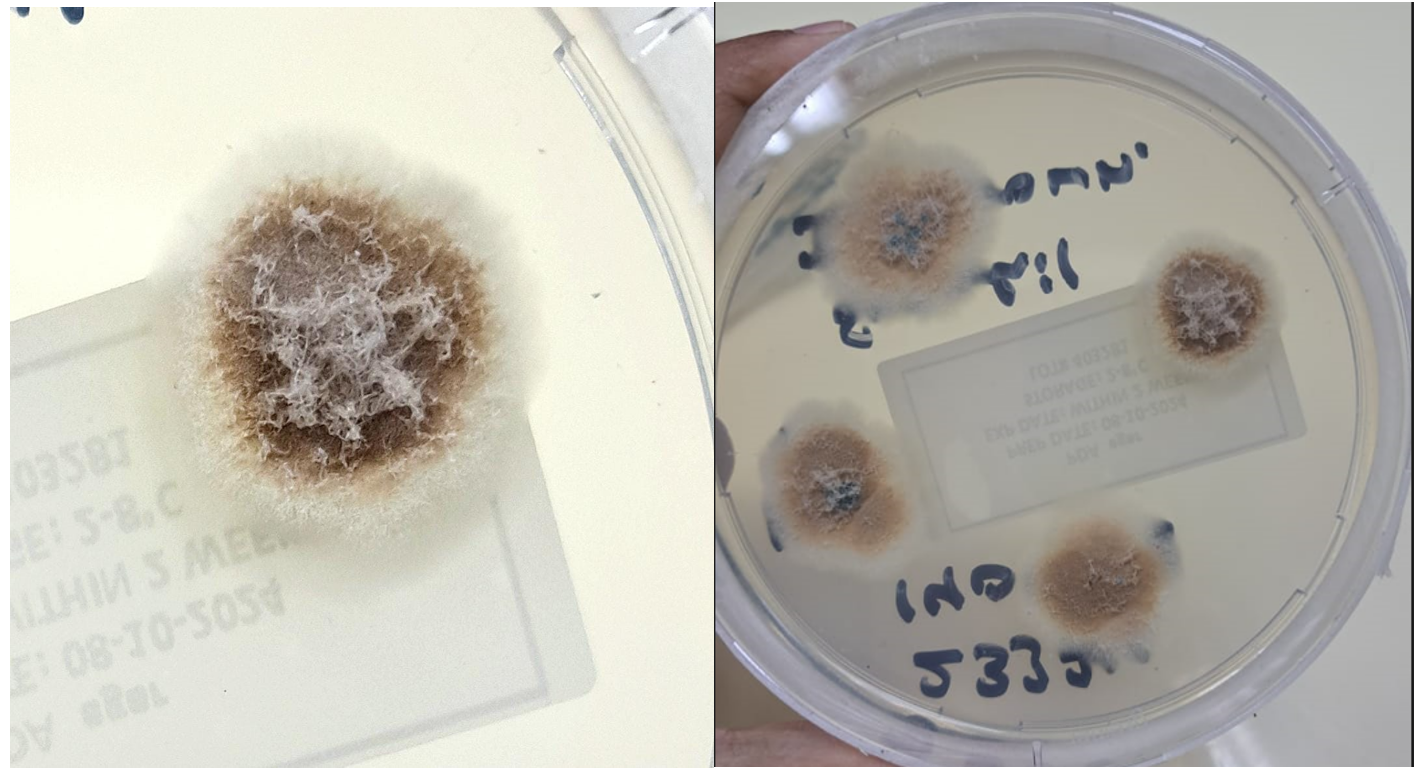
Figure 4b: Fungal cultures showed light brown colonies with a tan periphery and dark brown reverse coloration.
The patient was started on voriconazole on 24th October 2024 with plans to complete 12 months of antifungal therapy.
Repeat imaging of brain with MRI scan (Figure 5) in November, 2024 reported postsurgical changes in the right occipital lobe with complete resection of previously seen peripherally enhancing lesions. The left parietal lesion shows interval decrease in size, suggesting response to treatment.
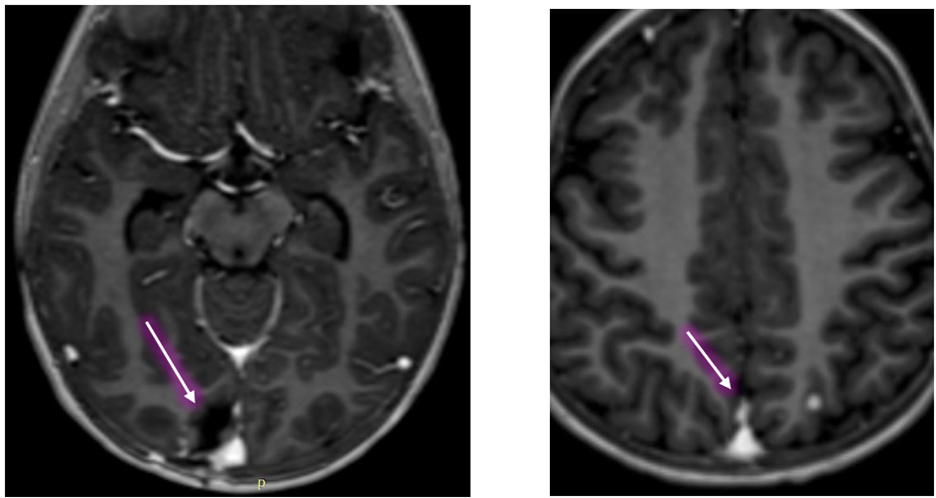
Figure 5: Brain MRI: Post contrst T1- weighted images showed postsurgical changes in right occipital lobe and decrease in size of enhancing focus noted in the left parietal cortex.
Previously demonstrated right occipital nodule has interval increase in size currently measuring 9mm against prior 5mm. Left posterior parietal lobe nodule currently measures 6.2mm against prior measurement of 5mm.
Follow up MRI brain in Feb, 2025 (Figure 6) revealed stable postsurgical changes in the right occipital lobe and a stable, tiny enhancing focus the left parietal lobe. As of March 7th 2025, the patient remains on voriconazole and is undergoing further chemotherapy.
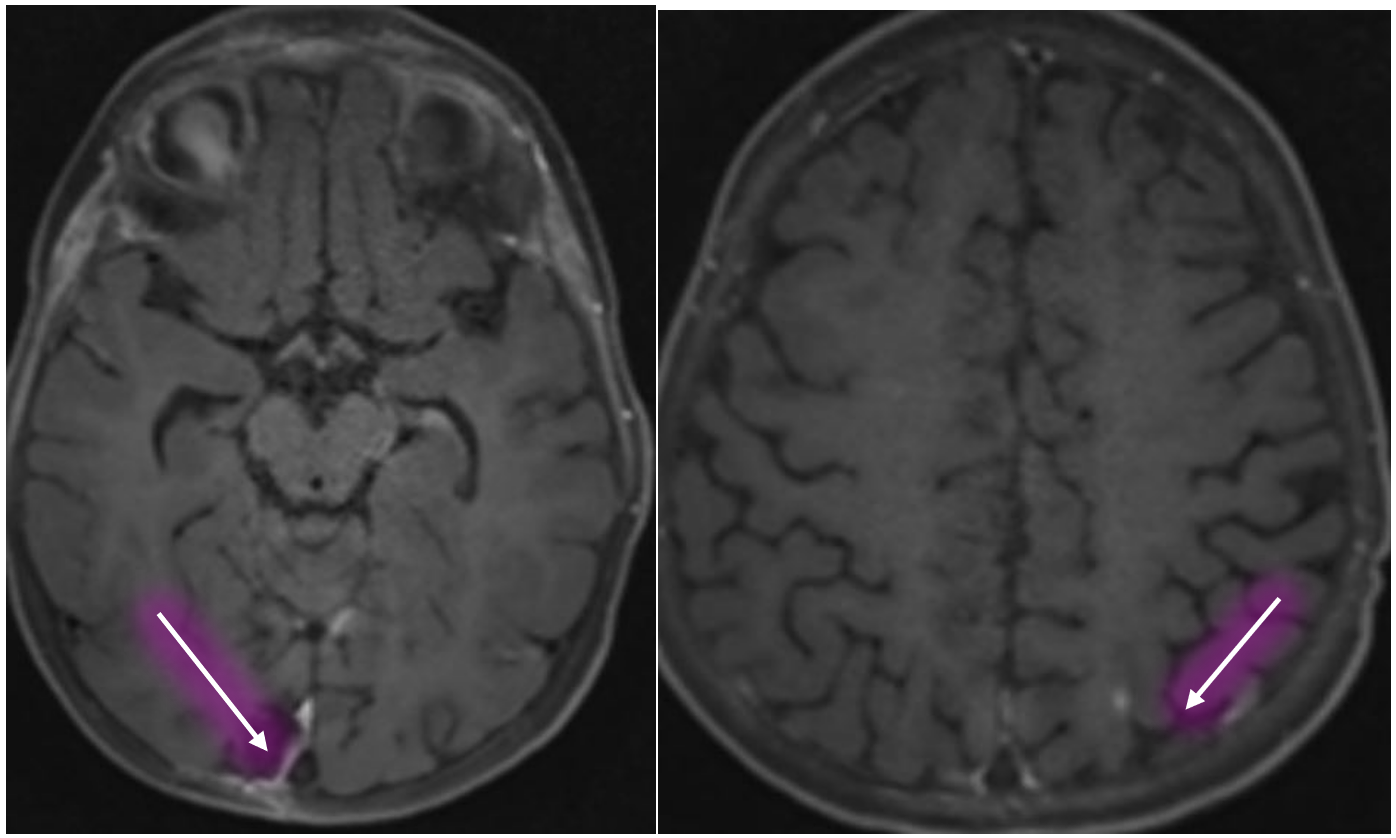
Figure 6: Brain MRI: Post contrast T1- weighted images showed stable postsurgical changes in right occipital lobe and stable enhancing focus noted in the left parietal cortex.
Discussion
This case report highlights a rare and severe fungal infection, secondary to Scopulariopsis species, affecting the brain of a 5-year-old female patient with Pre-B ALL. The patient's complex medical history, including multiple chemotherapy regimens and previous infections, increased her susceptibility to opportunistic infections. The diagnosis of Scopulariopsis species was challenging due to the non-specific symptoms and lack of typical radiological findings. However, the use of microscopy and fungal culture enabled the identification of the causative agent. Microscopic morphology demonstrated characteristic chain-forming conidia, consistent with Scopulariopsis species since antifungal susceptibility testing for moulds is not available in Pakistan, drug testing could not be performed.
The patient's response to voriconazole treatment was favorable, with significant improvement in clinical and radiological findings. This case underscores the importance of considering fungal infections in immunocompromised patients and highlights the need for early diagnosis and targeted antifungal therapy.
A literature review revealed a few case reports of Scopulariopsis species infections in adult patients, highlighting the rarity and severity of these fungal infections. Select cases of brain Scopulariopsis infections have been summarized in Table 1. [10-12]. Regarding the Scopulariopsis species, the case reports include one patient infected with Microascus cinereus, one by S. brevicaulis, and in the third case, the Scopulariopsis species was not identified. Two patients were immunocompromised while the third patient was immunocompetent. The patients were treated with antifungals and surgery (2 out of 3 patients). One patient was treated only with antifungal drugs. Two patients died due to the fungal infection; other one died from graft versus host disease of the gastrointestinal tract [10-12].
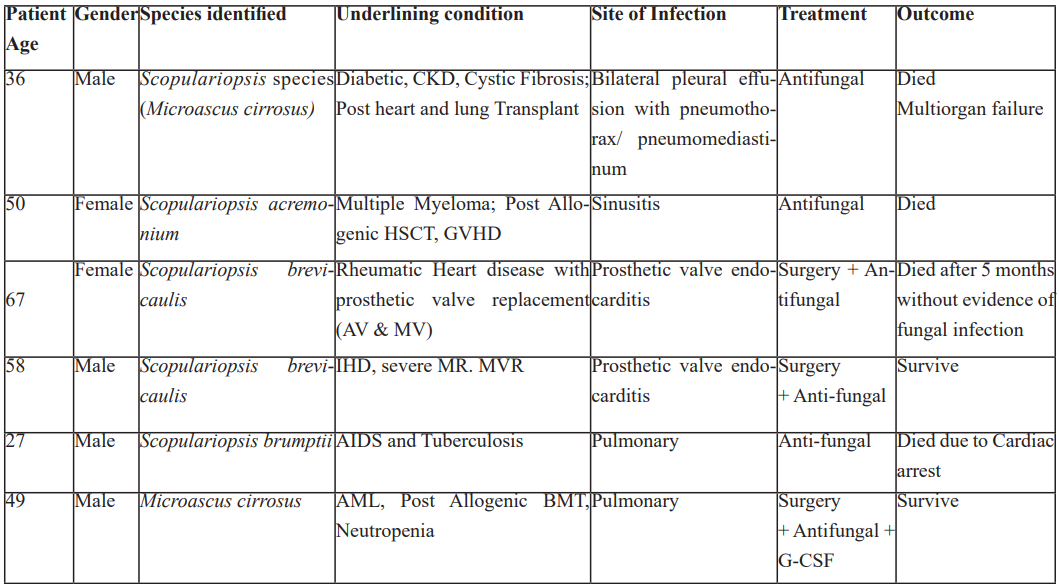
Scopulariopsis infections are typically treated with antifungal medications such as Amphotericin B, Voriconazole, Posaconazole, and Terbinafine. However, treatment can be challenging and the choice of antifungal medication may depend on the specific circumstances of the infection and the individual patient's needs. In some cases, combination therapy with multiple antifungal medications may be necessary [13-15]. Few other cases of Scopulariopsis infections have been summarized in Table 2. [16-21].
Table 1: Reported cases of Scopulariopsis Brain Infection [11-13].
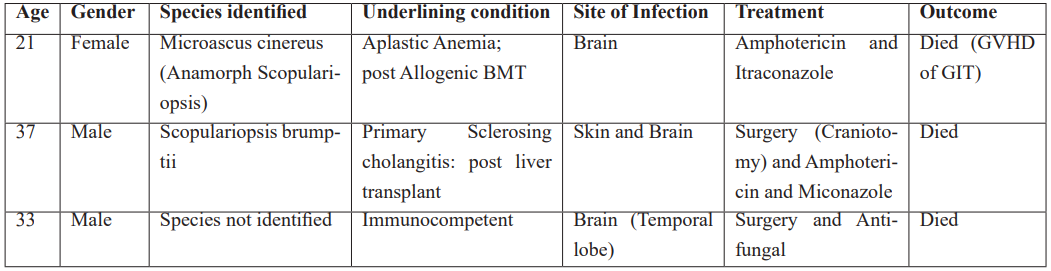
Table 2: Select Cases of Scopulariopsis other than brain [16-21].
Conclusion
This case report emphasizes the importance of vigilance and prompt diagnosis in managing opportunistic infections in immunocompromised patients. Fungal infection (Scopulariopsis) should be considered in the differential diagnosis of CNS infections in patients with underlying malignancies and immunosuppression. Species identification and MIC (Minimum Inhibitory Concentration) detection were not performed.
Early recognition and treatment with appropriate antifungal agents, such as voriconazole, can significantly improve outcomes in this patient. Further research is needed to understand the pathogenesis of Scopulariopsis species in CNS infections. Species identification and MIC detection should be performed in future cases to guide targeted antifungal therapy.
References
- Schmalreck AF, Lackner M, Becker K, Fegeler W, et al. Phylogenetic relationships matter: antifungal susceptibility among clinically relevant yeasts. Antimicrobial agents and chemotherapy, 2014; 58(3): 1575-1585.
- Gao B, Guo L, Zhao L, Duan Y, et al. Case Report of a Successfully Treated Scopulariopsis Infection in a Bilateral Lung Transplant Recipient. Exp Clin Transpla 275 nt, 2023; 21(3): 275-278.
- Sandoval-Denis M, Sutton DA, Fothergill AW, Cano-Lira J, et al. Scopulariopsis, a poorly known opportunistic fungus: spectrum of species in clinical samples and in vitro responses to antifungal drugs. Journal of Clinical Microbiology, 2013; 51(12): 3937-3943.
- Schoeppler KE, Zamora MR, Northcutt NM, Barber GR, et al. Invasive Microascus trigonosporus species complex pulmonary infection in a lung transplant recipient. Case Reports in Transplantation, 2015; 2015(1): 745638.
- Endo S, Hironaka M, Murayama F, Yamaguchi T, et al. Scopulariopsis fungus ball. The Annals of thoracic surgery, 2002; 74(3): 926-927.
- Cuenca-Estrella M, Gomez-Lopez A, Mellado E, Buitrago MJ, et al. Scopulariopsis brevicaulis, a fungal pathogen resistant to broad-spectrum antifungal agents. Antimicrobial agents and chemotherapy, 2003; 47(7): 2339-2341.
- Tunç AS, Baş B, Kutsal O. Invasive Fatal Scopulariopsis brevicaulis Infection in Canaries. Journal of Comparative Pathology, 2022; 196: 11-15.
- Gluck O, Segal N, Yariv F, Polacheck I, et al. Pediatric invasive sinonasal Scopulariopsis brevicaulis—a case report and literature review. International Journal of pediatric otorhinolaryngology, 2011; 75(7): 891-893.
- Steinbach WJ, Schell WA, Miller JL, Perfect JR, et al. Fatal Scopulariopsis brevicaulis infection in a paediatric stem-cell transplant patient treated with voriconazole and caspofungin and a review of Scopulariopsis infections in immunocompromised patients, J. Infect, 2004; 48(1): 112–116.
- Baddley JW, Moser SA, Sutton DA, Pappas PG. Microascus cinereus (anamorph Scopulariopsis) brain abscess in a bone marrow transplant recipient. Journal of Clinical Microbiology, 2000; 38(1): 395-397.
- Patel R, Gustaferro CA, Krom RA, Wiesner RH, et al. Phaeohyphomycosis due to Scopulariopsis brumptii in a liver transplant recipient. Clinical infectious diseases, 1994: 198-200.
- Hart AP, Sutton DA, McFeeley PJ, Kornfeld M. Cerebral phaeohyphomycosis caused by a dematiaceous scopulariopsis species. Clinical neuropathology, 2001; 20(5): 224-228.
- Pate MJ, Hemmige V, Woc‐Colburn L, Restrepo A. Successful eradication of invasive Scopulariopsis brumptii in a liver transplant recipient. Transplant Infectious Disease, 2016; 18(2): 275-279.
- Helander L, Stark M. Fatal Scopulariopsis brumptii in a pediatric immunocompromised host. Fetal and Pediatric Pathology, 2017; 36(1): 82-86.
- Paredes K, Capilla J, Mayayo E, Guarro J. Virulence and resistance to antifungal therapies of Scopulariopsis species. Antimicrobial agents and chemotherapy, 2016; 60(4): 2063-2068.
- Beltrame A, Sarmati L, Cudillo L, Cerretti R, et al A fatal case of invasive fungal sinusitis by Scopulariopsis acremonium in a bone marrow transplant recipient. International Journal of Infectious Diseases, 2009; 13(6): e488-92.
- Miossec C, Morio F, Lepoivre T, Le Pape P, et al. Fatal invasive infection with fungemia due to Microascus cirrosus after heart and lung transplantation in a patient with cystic fibrosis. Journal of clinical microbiology, 2011; 49(7): 2743-2747.
- Isidro AM, Amorosa V, Stopyra GA, Rutenberg HL et al. Fungal prosthetic mitral valve endocarditis caused by Scopulariopsis species: case report and review of the literature. The Journal of Thoracic and Cardiovascular Surgery, 2006; 131(5): 1181-1183.
- Jain D, Oberoi JK, Shahi SK, Shivnani G, et al. Scopulariopsis brevicaulis infection of prosthetic valve resembling aspergilloma on histopathology. Cardiovascular Pathology, 2011; 20(6): 381-383.
- Shankar EM, Vignesh R, Barton RC, Balakrishnan P, et al. Hydrothorax in association with Scopulariopsis brumptii in an AIDS patient in Chennai, India. Transactions of the Royal Society of Tropical Medicine and Hygiene, 2007; 101(12): 1270-1272.
- Ustun C, Huls G, Stewart M, Marr KA. Resistant Microascus cirrosu s pneumonia can be treated with a combination of surgery, multiple anti-fungal agents and a growth factor. Mycopathologia, 2006; 162: 299-302.

