Colchicine Poisoning: Rare and Often Fatal
Faris Yaseen*, Mohamed Anass Fehdi and Mohammed Mouhaoui
Emergency Department, CHU Ibn Rochd, Casablanca, Morocco
Received Date: 26/03/2025; Published Date: 30/04/2025
*Corresponding author: Faris Yaseen, Emergency Department, CHU Ibn Rochd, Casablanca, Morocco
Abstract
Introduction: Colchicine poisoning is a rare, serious and even fatal condition. It can be observed following an elimination defect, a drug interaction or massive ingestion of colchicine.
Observations: we present in our study the case of two siblings were admitted to the emergency department after colchicine ingestion in the aim of autolysis within a few months’ interval.
Conclusion: These cases in our study show that ingestion of doses of colchicine lower than the fatal dose of 0.8 mg/kg can still present with a fatal evolution. The hypothesis of symptomatic treatments with organ support at an early stage, in order to prevent a full-blown shock with multivisceral failure are still the most used techniques.
Keywords: Colchicine poisoning; Fatal; Multi-visceral defect
Introduction
Colchicine is a naturally occurring alkaloid found in the seeds and bulb of Colchicum autumnale. It has been used for its anti-inflammatory properties in prophylaxis and in the treatment of acute attacks of gout for decades. It is also prescribed in other diseases with an inflammatory component such as Familial Mediterranean Fever (FMF) or Behçet's disease [1-4].
Colchicine is a spindle poison that acts by binding to tubulin present in the intracellular compartment and inhibiting its polymerization into microtubules. This results in a decrease in the cellular mechanisms that can be involved in inflammation: a decrease in endocytosis and exocytosis, a decrease in cell motility and, at higher doses, a blockage of cell mitoses in metaphase also responsible for the toxicity of colchicine in particular for tissues with rapid turnover [1,2].
From a pharmacokinetic point of view [4], colchicine is rapidly absorbed across the gastrointestinal membrane, with peak blood concentrations being reached, depending on the individual, within 30 minutes to 3 hours after oral administration [2,4].
After a significant hepatic first-pass effect partly responsible for its low bioavailability (between 25 and 50%) [2,5], colchicine is distributed rapidly and massively in all tissues (Vd: 5—8.5 L/ kg) mainly intestinal mucosa, liver, kidneys and spleen [2]. Colchicine undergoes hepatic metabolism of the oxidative type ensured by CYP3A4 leading to the production of demethylated metabolites excreted in the bile. An enterohepatic cycle may lead to a second peak in plasma concentrations within 6 hours of administration [4]. 10% to 20% are also eliminated via the kidneys in unchanged form [6].
The elimination half-life in healthy volunteer patients has been estimated between 14 and 30 hours after oral administration [5].
Colchicine poisonings are rare but they are most often serious, even fatal[3,6–9]. They can be observed following an elimination defect (acute renal failure or hepatic failure), a drug interaction or massive ingestion of colchicine. We report here 2 cases of acute intoxication occurring secondary to a massive intake of colchicine in the context of a suicide attempt.
Observations
Observation 1
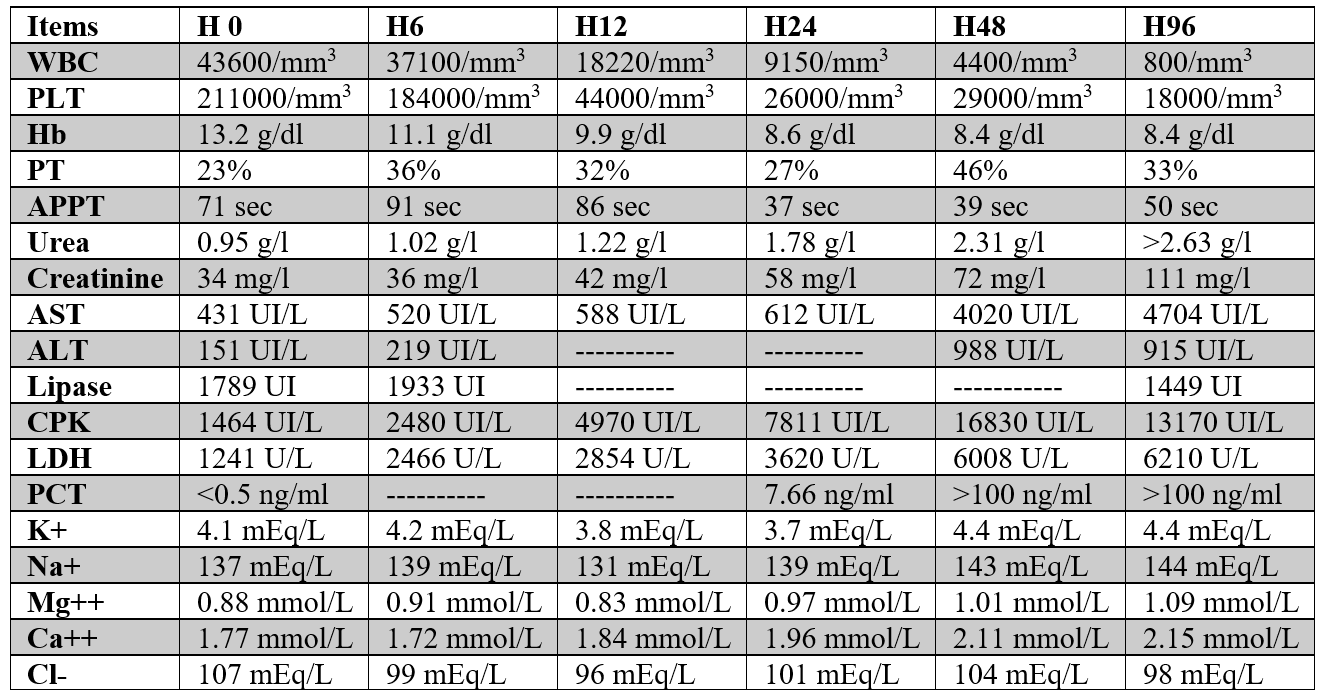
Patient S.O, 38 years old female, followed for depression for 3 months, admitted to the vital emergency room for colchicine poisoning 15h prior to arrival, with the aim of autolysis. She had ingested 40 tablets of colchicine 1 mg of a dose 0.72 mg/kg, without any notion of vomiting following ingestion. Initially, her vital signs, hemodynamically, respiratory and neurologically were stable, with a heartbeat of 96 beats per minute, blood pressure 131/66 mmHg, respiratory rate 15 breaths per minute, oxygen saturation 98% on air room. She reported gastrointestinal manifestations including abdominal pain, vomiting with liquid diarrhea. We proceeded to an evacuating treatment based on activated charcoal despite the 15h interval prior ingesting, as well as a symptomatic treatment based on rehydration. Emergency blood tests were requested, objectifying a hyperleukocytosis at 43,600, a PT at 23%, an elongated APPT at 71 sec (control at 30 sec), renal insufficiency with urea at 0.95 g / L, creatinine at 34 mg /L, hepatic cytolysis with AST at 431 and ALT at 151 IU/L, lipase a 1789 IU/L, CPK a 1464 IU/L and LDH has 1241 IU/L (table 1). An ECG was performed showing sinus tachycardia. Rehydration was set up, with frozen plasma pellet transfusion. The evolution at H+22 of her admission was marked by the appearance of a hemodynamic instability (low blood pressure 79/34 mmHg and rapid heart rate 142 bpm) having responded to the filling at the beginning then to vasopressors (Norepinephrine 40 mcg/kg/h), chest tightness, shortness of breath, and difficulty breathing, then the patient was altered on the neurological level which required an intubation with realization of a cerebral scanner returning normal.
She progressed to circulatory failure, respiratory dysfunction, liver and kidney failure and coagulopathy.
Because of her acute renal failure, hemodialysis was taken in consideration, but she had unstable circulation with low blood pressure (75-95/35-55 mmHg) even with high doses of norepinephrine (reached 200 mcg/kg/h).
Treatment by frozen plasma, antibiotics and proton pump inhibitors were administrated as well.
Patient’s vital functions deteriorated further and died 96hours approximately after admission.
Observation 2
Patient S.F., 30 years old male, with a history of drugs addiction (Hashish and MDMA commonly known as ecstasy), admitted to the vital emergency room for colchicine poisoning 14h prior arrival, with the aim of autolysis. He ingested 40 colchicine 1 mg tablets of a dose 0.67 mg/kg, without any notion of spontaneous or provoked vomiting following ingestion. Initially he was hemodynamically, respiratory and neurologically stable. He reported vomiting with abdominal and pelvic pain. We proceeded to an evacuating treatment based on activated charcoal, as well as a symptomatic treatment based on rehydration.
A biological assessment was requested, objectifying a hyperleukocytosis at 45,330/mm3, a platelet count at 215,000/mm3, a PT at 23%, an elongated APPT at 61 sec (control at 30 sec), renal failure with urea at 0.75 g/L, creatinine at 44 mg/L, hypochloremia at 83 mmol/L, hepatic cytolysis with AST at 539 IU/L and ALAT at 142 IU/L, lipase a 1039 IU/L, CPK a 644 IU/L and LDH has 892 IU/L. an ECG was performed showing repolarization disorders. Rehydration was set up, with frozen plasma transfusion. The evolution was marked by the appearance of hemodynamic instability justifying vascular filling, catecholamines at increasing doses guided by hemodynamic monitoring, respiratory and neurological distress at H+12 which required an intubation with realization of a cerebral scanner returning normal and thoracic in favor of alveolar hemorrhage. The patient had died in a picture of multi-visceral failure at H46 of his admission.
Table 1: Laboratory blood tests over time for patient S. O.
Discussion
Colchicine poisoning is rare but most often serious, even fatal [3,7]. Patient care must be carried out as early as possible in order to limit the absorption of colchicine. Indeed, once absorbed, only symptomatic treatment can be implemented, as no antidote is currently available [1,8]. The use of activated charcoal is usually reserved for an acute overdose of this drug (up to two hours after drug ingestion) since it adsorbs colchicine, preventing gastrointestinal absorption and interrupting its enterohepatic circulation. Despite this, large amounts of colchicine have been found to remain in the stomach even 24 hours after ingestion so, though these patients already have a late presentation of more than 12 hours, they were given activated charcoal upon admission [10].
The appearance of digestive disorders in a context of taking colchicine should therefore not be neglected. Early measurement of colchicine blood concentrations has no prognostic value for intoxication, but it is essential to confirm intoxication [11,12]. In cases of severe poisoning, regular measurement of colchicine concentrations will make it possible to monitor the evolution of the poisoning.
Colchicine intoxication develops in three phases. After ingestion, the latency phase before the appearance of the first symptoms is 6 to 12 hours [4,7,13]. In the first phase, the patient presents with gastrointestinal disturbances, vomiting and diarrhea. This first phase may reflect mild poisoning. The second phase theoretically appears between the 2nd and 7th day and is characterized by the persistence of digestive disorders and a drop in coagulation factors. Bone marrow aplasia and multi-visceral failure (particularly respiratory, cardiac, and neurological) appear suddenly from the 3rd day. In the case reported, the second phase begins on day 3 with the appearance of tricytopenia signifying bone marrow aplasia and coagulopathy due to hepatic failure, death most frequently occurs in the context of multi-visceral failure [14].
In our study, the first phase is presented by gastrointestinal symptoms in the 2 cases, and the passage of the 2nd and 3rd phase in the 36h prior admission to the ER which follows [10,12-14], a hemodynamic instability refractory to filling at the beginning then to vasoactive drugs and a respiratory and neurological distress, then death following a multi-visceral failure.
Conclusion
Cases of massive ingestion of colchicine are rare, and mostly in the context of autolysis. These cases in our study show that ingestion of doses of colchicine lower than the fatal dose of 0.8 mg/kg can still present with a fatal evolution. The typical signs of gastrointestinal distress with the need of rapid organ support and close follow-up before the installation of the multivisceral dysfunction. The authors support the hypothesis of symptomatic treatments with organ support at an early stage, in order to prevent a full-blown shock with multivisceral failure, but further studies on the effects and treatment of massive overdose of this drug still are required.
Competing interests: The authors declare no competing interests.
Author’s contribution: Patient management: Faris YASEEN and Mohamed Anass Fehdi; Data collection: Faris Yaseen; Manuscript drafting: Faris Yaseen; Manuscript revision: Mohamed Anass Fehdi, Mohammed Mouhaoui. All authors read and approved the final version of this manuscript.
References
- Niel E, Scherrmann J-M. Colchicine today. Joint Bone Spine, 2006; 73: 672–678.
- Kapp RW. Clarke’s Analysis of Drugs and Poisons, 3rd edition Edited by Anthony C. Moffat, M. David Osselton, and Brian Widdop Publisher: Pharmaceutical Press: London, 2004; 1: 480; 2004; 2: 1176. Int J Toxicol, 2006; 25: 81–82.
- Deveaux M, Hubert N, Demarly C. Colchicine poisoning: case report of two suicides. Forensic Science International, 2004; 143: 219–222.
- Rochdi M, Sabouraud A, Girre C, Venet R, Scherrmann JM. Pharmacokinetics and absolute bioavailability of colchicine after i.v. and oral administration in healthy human volunteers and elderly subjects. Eur J Clin Pharmacol, 1994; 46: 351–354.
- McCabe DJ, Wilson BZ, Radke JB, Bottei EM. A Fatal Colchicine Ingestion With Antemortem Blood Concentration. Am J Forensic Med Pathol, 2022; 43: 253–255.
- Milne ST, Meek PD. Fatal colchicine overdose: Report of a case and review of the literature. The American Journal of Emergency Medicine, 1998; 16: 603–608.
- Bodeau S, Bennis Y, Abe E, Quinton M-C, Andréjak M, Bricca G, et al. Colchicine: une intoxication rare mais souvent mortelle – À propos de 3 cas d’intoxication aiguë. Toxicologie Analytique et Clinique, 2016; 28: 32–37.
- Schaffer DH, Overbeek DL, Erickson TB, Boyer EW, Goldfine C, Muhsin SA, et al. Severe colchicine poisoning treated successfully with kidney replacement therapy and plasmapheresis: a case report. Toxicology Communications, 2022; 6: 46–50.
- Miller MA, Hung Y-M, Haller C, Galbo M, Levsky ME. Colchicine-related death presenting as an unknown case of multiple organ failure. J Emerg Med, 2005; 28: 445–448.
- Zawahir S, Gawarammana I, Dargan PI, Abdulghni M, Dawson AH. Activated charcoal significantly reduces the amount of colchicine released from Gloriosa superba in simulated gastric and intestinal media. Clin Toxicol (Phila), 2017; 55: 914–918.
- Finkelstein Y, Aks SE, Hutson JR, Juurlink DN, Nguyen P, Dubnov-Raz G, et al. Colchicine poisoning: the dark side of an ancient drug. Clin Toxicol (Phila), 2010; 48: 407–414.
- Fu M, Zhao J, Li Z, Zhao H, Lu A. Clinical outcomes after colchicine overdose. Medicine (Baltimore), 2019; 98: e16580.
- Leung YY, Yao Hui LL, Kraus VB. Colchicine--Update on mechanisms of action and therapeutic uses. Semin Arthritis Rheum, 2015; 45: 341–350.
- Wu J, Liu Z. Progress in the management of acute colchicine poisoning in adults. Intern Emerg Med, 2022; 17: 2069–2081.

