Cystic Meningioma: A Rare Presentation and Case Report
Nabil Nia*, Marouane Hammoud, Mdarhri Mehdi, Oualid Mohammed Hmamouche, Fayçal Lakhdar, Mohammed Benzagmout, Khalid Chakour and Mohammed El Faiz Chaoui
Department of Neurosurgery, Hassan II University Hospital, Fez, Morocco
Received Date: 24/03/2025; Published Date: 29/04/2025
*Corresponding author: Nabil Nia, Department of Neurosurgery, Hassan II University Hospital, Fez, Morocco
Abstract
Cystic meningiomas are an uncommon subtype of intracranial meningiomas, accounting for 2– 4% of all cases. Their radiological appearance often mimics other cystic brain lesions, making preoperative diagnosis challenging. We report a case of a 67-year-old woman presenting with progressive left-sided hemiparesis. Neuroimaging revealed a right fronto-temporo-parietal cystic lesion exerting a mild mass effect. Histopathological examination confirmed the diagnosis of cystic meningioma. The patient underwent a successful surgical resection. This case highlights the diagnostic challenges, surgical considerations, and pathological findings of cystic meningiomas, emphasizing the importance of multimodal imaging and complete cyst wall excision to minimize recurrence risk.
Introduction
Meningiomas are the most common primary intracranial tumors, accounting for 15–20% of all central nervous system neoplasms. However, the presence of cystic components in meningiomas is rare, occurring in 2–4% of cases, and presents a diagnostic challenge as they can be mistaken for gliomas, metastases, or hemangioblastomas [1].
Cyst formation in meningiomas can be intratumoral, peritumoral, or mixed. The exact pathophysiology remains debated, but proposed mechanisms include tumoral degeneration, ischemic necrosis, hemorrhage, or active secretion by tumor cells. Radiologically, cystic meningiomas can display atypical imaging features, complicating preoperative diagnosis [1].
This report discusses the clinical presentation, radiological findings, and surgical outcomes of a cystic meningioma in a 67-year-old patient, contributing to the growing understanding of this uncommon tumor subtype.
Case Presentation
Patient History and Clinical Findings
A 67-year-old woman with no significant past medical history presented with progressive left- sided hemiparesis evolving over three months. The patient reported intermittent headaches over the past two years, with recent worsening. No seizures, cognitive disturbances, or cranial nerve deficits were noted.
Neurological examination revealed:
GCS : 15/15
- Left-sided hemiparesis (muscle strength 3/5)
- Preserved deep tendon reflexes (DTRs)
- No cranial nerve deficits
- No sensory impairment Neuroimaging Findings
A CT scan showed a right fronto-temporo-parietal cystic lesion (58.2 × 46.1 mm) with mild mass effect on the right lateral ventricle and a slight midline shift. No calcifications or hemorrhagic components were observed.
MRI revealed :
- A well-circumscribed extra-axial cystic lesion with a dominant cystic component and a peripheral solid nodule.
- The solid portion showed homogeneous gadolinium enhancement, while the cystic part exhibited no contrast uptake.
- FLAIR sequences displayed mild perilesional edema.
- The lesion caused compression of the adjacent cortex, leading to sulcal effacement and a midline shift of ~6 mm.
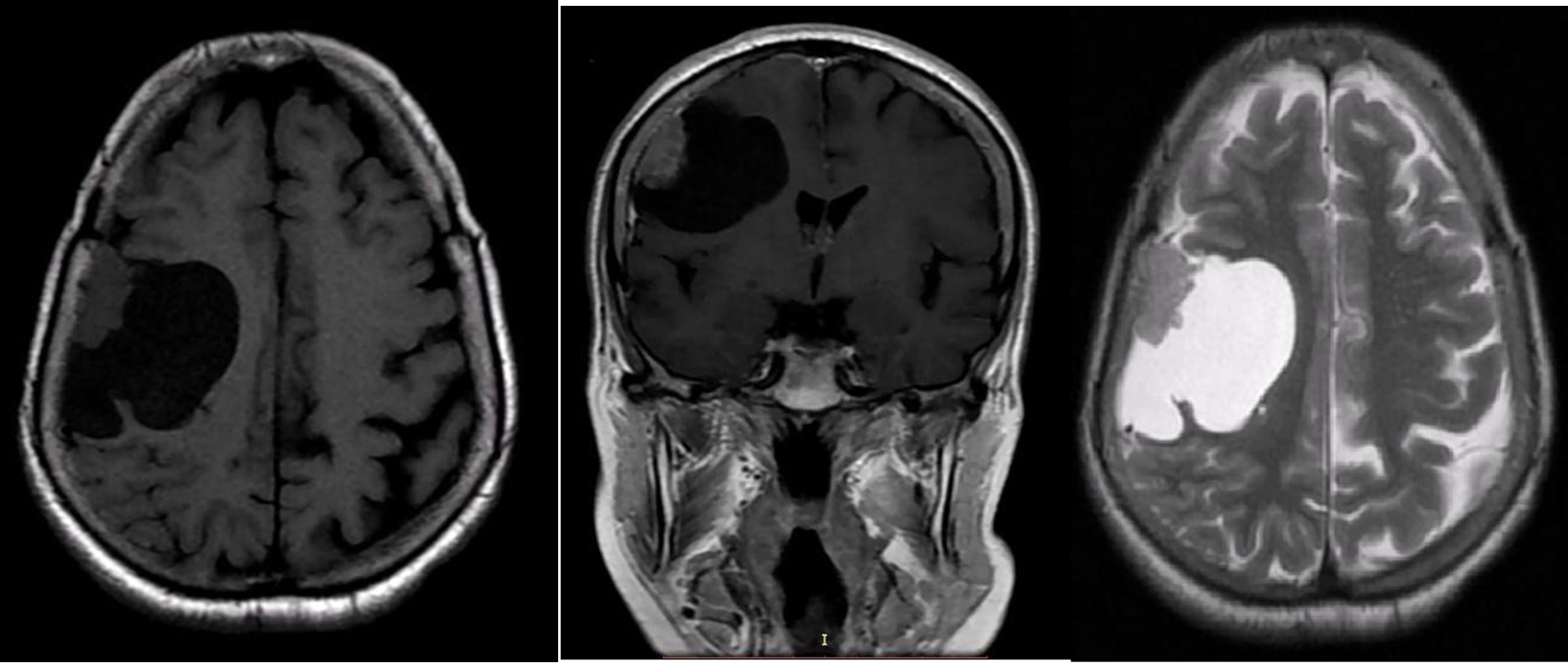
Figure 1: MRI showing A well-circumscribed extra-axial cystic lesion with a dominant cystic component and a peripheral solid nodule.
Based on these imaging features, a cystic meningioma was the leading differential diagnosis.
Surgical Management
The patient underwent a right fronto-temporo-parietal craniotomy for tumor resection. Intraoperatively :
- The lesion was extra-axial, with a fibrous capsule and clear cystic
- The solid portion was firmly adherent to the dura mater, supporting a meningioma
- The cystic wall was carefully dissected and completely excised, as neoplastic cells were suspected to line the cystic wall.

Figure 2: Peri-Operative Image of the solid portion of the tumor adhering to the dura mater.
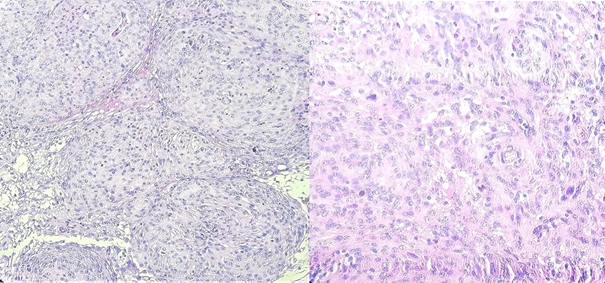
Figure 3: The monomorph meningothelial tumoral proliferation is hallowed with microcystis of various size (HE × 100).
The histological examination of the surgical specimen confirmed the diagnosis of transitional cystic meningioma.
Postoperatively, the patient showed progressive improvement in motor function, with muscle strength increasing to 4/5 at 3-month follow-up.
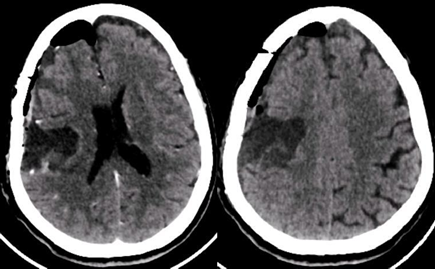
Figure 4: Post-operative brain scan.
Discussion
Pathophysiology of Cystic Meningiomas
Cyst formation in meningiomas is rare [2] and may arise from:
- Ischemic necrosis and tumor degeneration
- Secretory activity of tumor cells
- Arachnoid entrapment leading to peritumoral cyst formation
Histocystic meningiomas can be WHO grade I (benign) or higher-grade variants. In some cases, atypical or malignant meningiomas exhibit cystic changes, necessitating thorough histopathological evaluation.
Cystic meningiomas mimic other cystic brain lesions, complicating preoperative diagnosis. Gliomas, metastases, hemangioblastomas, and neuroglial cysts should be considered as differentials [3]. The following MRI features help distinguish them:
- Meningiomas: Extra-axial location, dural attachment, homogeneous enhancement of solid portions.
- Gliomas: Intra-axial, irregular enhancement, infiltrative
- Metastases: Strong peripheral enhancement, surrounding vasogenic
- Hemangioblastomas: Strong enhancement, flow voids, cerebellar predilection
According to the radiological, operative, and histological data, the case we report corresponds to type 2 of Nauta's classification [6]. This author divided cystic meningiomas into four categories based on the location of the cystic cavity: type 1 is a meningioma where the intratumoral cyst is central, type 2 is where the cyst is intratumoral but peripheral, type 3 is where the cyst is peritumoral in the adjacent brain parenchyma, and type 4 is where the cyst is located peritumoral between the tumor and the adjacent parenchyma.
Intratumoral cysts are rare, and they are produced by secretory or degenerative phenomena, ischemic necrosis, hemorrhage, or demyelination due to a perfusion defect of the white matter [7]. The peritumoral cyst is typically large and unilocular with xanthochromic fluid content, and it results from the glial response to the presence of the meningioma with fluid production by glial cells [8]. The CT interpretation of cystic meningiomas can be difficult, unlike the solid form where the scanner has a sensitivity of 100% and a specificity of 90%.
The diagnosis of cystic forms is made preoperatively by computed tomography in less than 40% of cases, thus explaining the possibility of confusion between cystic meningioma and other intracranial tumors, notably gliomas and metastases [9.12]. Magnetic resonance imaging is highly sensitive in diagnosing this type of tumor as it allows for easy identification of the dural attachment, the interface between the tumor, the cyst, and the normal brain parenchyma [7.8.10.13.14.15]. Therapeutically, the recommendation to respect the cyst wall is important and crucial in order to minimize the recurrence of this benign lesion [11.7].
Complete cyst wall excision is essential to prevent recurrence, as neoplastic cells are often present within the cyst wall [4]. Studies suggest that up to 60% of cystic meningiomas contain tumor cells within the cystic lining, warranting aggressive resection whenever feasible [5].
In our case, this completely excised, including the cystic wall, minimizing recurrence risk.
Prognosis and Follow-Up
Cystic meningiomas have a slightly higher recurrence risk compared to solid meningiomas, particularly if cystic remnants are left behind. Our patient remains recurred 6-month follow-up, with progressive neurological recovery.
Conclusion
Cystic meningiomas are rare but diagnostically challenging tumors that require meticulous preoperative evaluation and complete surgical resection. This case underscores:
- The importance of multimodal imaging for distinguishing cystic meningiomas from other intracranial cystic lesions.
- The need for complete cyst wall excision to reduce recurrence
- The role of histopathological confirmation in guiding postoperative
References
- Boukobza M, et al. “Cystic meningioma: radiological, histological, and surgical particularities in 43 patients,” Acta Neurochir, 2016; 158(10): pp. 1955–1964. doi: 1007/s00701-016-2898-x.
- Singh D, Scalia G, Mathand VU, Chaurasia B. “Cystic meningiomas: A complex diagnostic challenge and clinicopathological insights from a unique case presentation”, doi: 1002/ccr3.8781.
- Ghani E, Al-Yamany M. “Intracranial cystic meningiomas: A rare type of tumours,” Br J Neurosurg, 2015; 29(3): pp. 396–400. doi: 10.3109/02688697.2014.997673.
- Gkasdaris G, et “Purely cystic meningioma: Case report and systematic review of the literature,” Clinical Neurology and Neurosurgery, 2022; 223: p. 107498. doi: 10.1016/j.clineuro.2022.107498.
- Nauta HJW, Tucker WS, Horsey WJ, Bilbao JM, Gonsalves C. Xanthochromic cystics associated with Journal of neurology, neurosurgery, and psychiatry, 1979; 42: 529–535.
- De Jesus O, Rifkinson N, Negron Cystic meningiomas: a review. Neurosurgery, 1995; 36: 489–492.
- Zee CS, Chen T, Hinton DR, Tan M, Segall HD, Apuzzo ML. Magnetic resonance imaging of cystic meningiomas and its surgical Neurosurgery, 1995; 36: 492–498.
- Fortuna A, Ferrante L, Acqui M, Guglielmi G, Mastronardi Cystic meningiomas. Acta neurochirurgica, 1988; 90: 23–30.
- Chen TY, Lai PH, Ho JT, Wang JS, Chen WL, Pan HB, et al. Magnetic resonance imaging and diffusion-weighted images of cystic meningioma: correlating with histopathology. Clinical imaging, 2004; 28: 10–19.
- Inoue T, Kuromatsu C, Sawada K, Matsushima Recurent cystic meningioma. Surgical neurology, 1986; 26: 399–404.
- Ueno Y, Tanaka A, Nakayama Y, Nomoto Intracerebral cyst associated with meningioma. Clinical neurology and neurosurgery, 1999; 101: 271–274.
- Qasho R, Epimenio RO. Cystic meningioma: neuroradiological (MRI, CT) and macroscopic intraoperative A case reports. Neurosurgical review, 1998; 21155–21157.
- Umansky F, Pappo I, Pizov G, Shalit Cystic changes in intracranial meningiomas: a review. Acta neurochirurgica, 1998; 95: 13–18.
- Wasenko JJ, Hochhauser L, Stopa EG, Winfield JA. Cystic meningiomas MR characteristics and surgical AJNR. American journal of neuroradiology, 1994; 15: 1959–1965.

