Spermocytic Tumor
Safwate R*, Nachid A, Safieddine MM, Kbirou A, Moataz A, Dakir M, Debbagh A and Aboutaieb R
Department of Urology CHU Ibn Rochd Casablanca, Morocco
Received Date: 01/03/2025; Published Date: 23/04/2025
*Corresponding author: Safwate Reda, Department of Urology CHU Ibn Rochd Casablanca, Morocco
Abstract
Spermatocytic seminoma is an uncommon tumor, accounting for less than 1% of all malignant testicular tumors. This type of germ cell tumor is recognized as a distinct entity, characterized by unique features in terms of histogenesis, clinical presentation, histology, and prognosis. We report a case of a male patient of 72 years old who came to our medical structure for a swelling of the left testicle, A scrotal mass was identified during examinations and subsequently surgically excised. Histological and immunochemical analyses indicated the presence of a spermatocytic tumor.
Keywords: Spermocytic Testis; Seminoma; Tumor
Introduction
Spermatocytic Seminoma (SS) is a rare tumour, accounting for less than 1% of malignant testicular tumours [1]. This tumour has both a clinical and anatomopathological appearance that differs from the classic seminoma, characterized essentially by a slow evolution, an early stage at the time of diagnosis, and the absence of metastasis.
The diagnosis relies on histopathology and the overall prognosis is typically favorable unless a sarcomatous component is present. The primary mode of treatment is surgery [2,3]. We report a recent occurrence of spermatocytic seminoma and conduct a comprehensive examination of its diagnostic, anatomopathological, therapeutic, and evolutionary aspects.
Case Report
J.A, aged 72, married with 4 children, butcher, chronic smoker, no pathological history, no cryptorchidism, no infertility, no family history of testicular cancer.
Symptoms began 1 year before with the progressive appearance of a painless swelling of the left testicle, with no other associated signs, and the patient's general condition remained unchanged. Clinical examination revealed an enlarged, painless left testicle, with a regular surface and homogeneous structure. Biological tests were normal, with negative tumour markers: Lactate Dehydrogenase (LDH), Human Chorionic Gonadotropin (HCG) and Alpha-Fetoprotein (AFP).
Scrotal Doppler ultrasound revealed an enlarged (360cc) heterogeneous left testis with multiple hypoechoic patches, hypervascularised on Doppler.
Inguinal orchiectomy was indicated in this patient.
Macroscopic examination showed the presence of a multilocular solid cystic mass measuring 10.5x11x6 cm occupying the entire testicle. The solid areas were the site of necrotic remodeling estimated at 60%, hemorrhagic and myxoid (Figure 1).
Histological examination showed a tumour proliferation of diffuse and multinodular architecture, surrounded by fibrous bands, with a high cell density (Figure 2). Cytologically, there are three cell populations: small cells with rounded and dense nuclei; intermediate cells with a granular chromatin nucleus that is rarely filamentous and with reduced cytoplasm; large cells with the same chromatin texture as the intermediate cells (Figure 3).
However, the immunohistochemical study showed negative labelling for the anti-PLAP antibody as well as for the anti-CD 30, anti-CK, anti-CD 10, anti-CD 20 and anti-CD 117. Diffuse nuclear labelling of anti-SALL4 antibody by tumor cells is observed.
The diagnosis of spermatocytic seminoma was thus established.
Post-operative biological markers (LDH/HCG/AFP) were always negative and the postoperative thoracic-abdominal-pelvic CT scans showed no evidence of distant lymph node or visceral metastases. Adjuvant chemotherapy or radiotherapy was deemed unnecessary, and vigilant monitoring was advised. As of 18 months post-surgery, the patient remains free from tumor recurrence.

Figure 1: Multilocular solid and cystic tumour (non-individualisable testis).
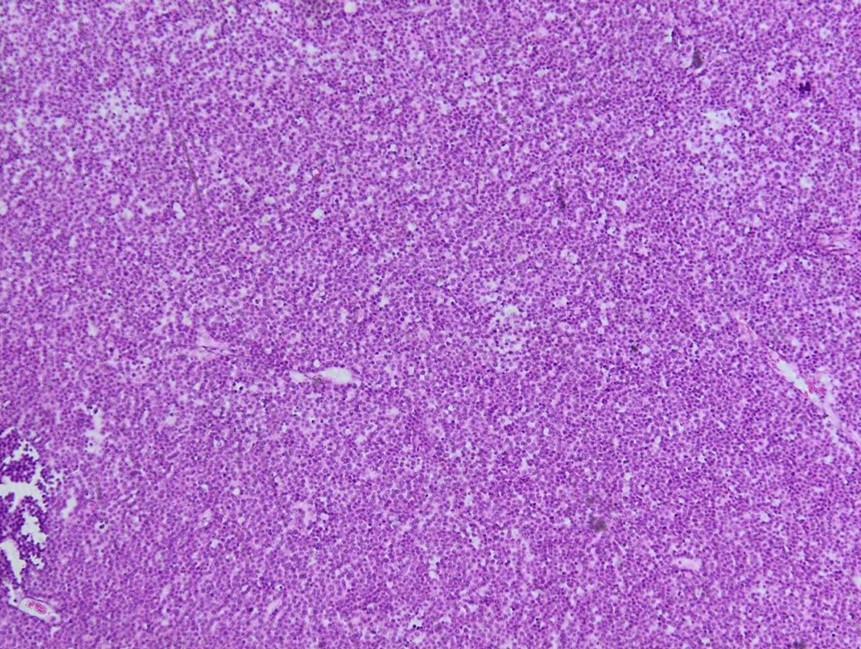
Figure 2: Blankets of cells with diffuse architecture.
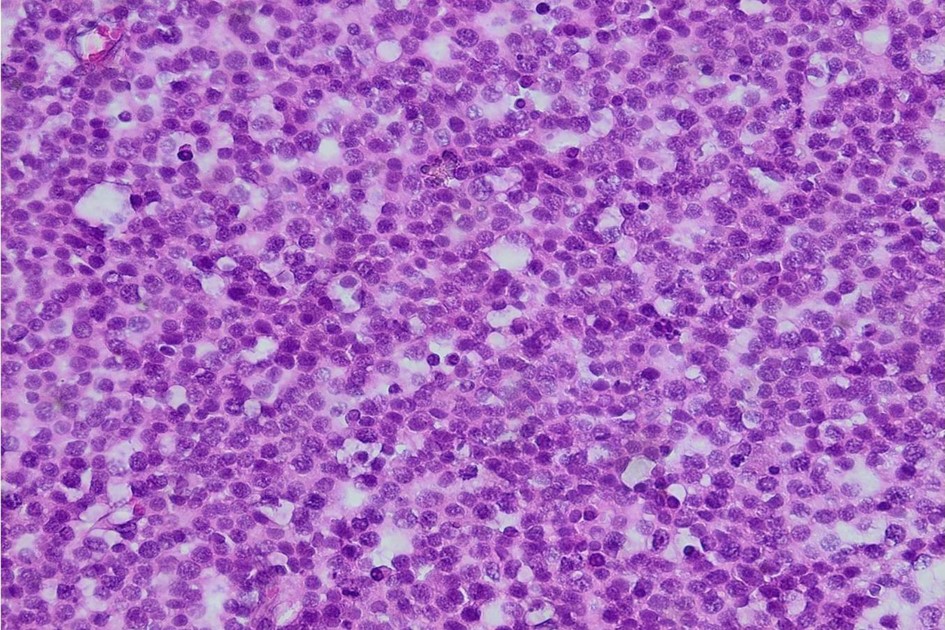
Figure 3: Image showing three cell populations: small cells with dense nuclei, intermediate cells with granular nuclei, large cells. (High magnification).
Discussion
Spermatocytic Seminoma was first described by Pierre Masson in 1946. It accounts for 4-7% of all seminomas [2,6] and 1-2% of testicular germ cell tumors [4]. For several reasons, it is considered a separate entity. It is thought to arise from spermatogenesis cells: spermatogonia and spermatocytes found in the seminiferous tubules [2,3,4]. It is therefore a more differentiated tumor than other germ cell tumors [3].
It is an exclusively testicular tumour, which has never been observed in the ovary or on an ectopic testicle. It is not associated with any of the risk factors for germ cell tumours (cryptorchidism, hypofertility, gonadal dysgenesis). The age of onset varies in the literature from 19 to 92 years, with a peak in frequency between the fifth and sixth decades (54 years). Our patient was 72 years old.
The SS is thought to be secondary to age-dependent activation of mutations in the FGFR3 and HRAS genes and amplification of the short arm of chromosome 9 corresponding to the DMRT1 gene [5].
Serum markers are consistently negative and are therefore of no value in the initial diagnosis or in monitoring.
Uncharacteristic symptoms are limited to a painless swelling. The tumour is usually unilateral.
Macroscopically, SS presents as a multinodular, well-limited, soft, gelatinous or myxoid tumour, sometimes cystic or more rarely necrotic-hemorrhagic [5]. As in the case of our patient.
Histological aspects as well as immunohistochemical study allows to make the difference, OCT4, PLAP, αFP, βHCG and CD30 are negative. CD117 (kit), SALL4 and oct2 are positive. [4]
Given the advanced age of patients, the differential diagnosis is essentially lymphoma and metastasis, especially in cases of bilateral involvement. Histological studies and immunohistochemistry (lymphoid markers, cytokeratins, neuroendocrine markers, Melan-A, etc.) help to correct the diagnosis. Differential diagnosis can also be made with classic seminoma.
As well as making a positive diagnosis, the pathologist's other role is to look for a sarcomatous contingent, in particular a rhabdomyosarcoma, which has a completely different prognosis [1-4]. This association is always accompanied by a rapidly unfavorable metastatic course (essentially in the retroperitoneum, lung and liver) [1, 3,4,]. Otherwise, it is a benign tumor with a favorable prognosis. However, only one case of pure SS has developed metastases [5].
Inguinal orchiectomy is a sufficient and appropriate treatment for this condition. The prognosis is better in the absence of a sarcomatoid component, with a 10-year survival rate for stages I exceeding 10 years [5].
Conclusion
Spermtocitic Seminoma is a rare germinal cell tumour that should be considered in elderly patients with large testicular tumours and negative serum markers. The polymorphic cellular appearance on histology and c-Kit expression on immunohistochemistry are characteristic. A sarcomatous component should be sought, as it completely transforms the prognosis.
Conflicts of interest: The authors have no conflicts of interest.
The examination of the patient was conducted in accordance with the Declaration of Helsinki Principles. Written informed consent was obtained from the patient for publication of this article.
References
- Decaussin M, Borda A, Bouvier R, et al (2004) Le séminome spermatocytaire: étude anatomo-clinique et immunohistochimique de 7 cas. Ann Pathol, 2004; 24: 161–166.
- EL Fellah H, Tijami F, Jalil A. Séminome spermatocytaire (à propos de deux cas). J Maroc Urol, 2008; 11: 25–28.
- Chelly I, Mekni A, Gargouri MM, et al (2006) Séminome spermatocytique avec contingent rhabdomyosarcomateux. Progr Urol, 2006; 16: 218–220.
- Camparo P, Houlgatte A. Classification des tumeurs testiculaires. EMC (Elsevier Masson SAS, Paris), Urologie. 2008; 18-650-A-11.
- Haroon S, Tariq MU, Fatima S, Kayani N. Spermatocytic seminoma: a 21 years’ retrospective study in a tertiary care hospital in Pakistan. Int J Clin Exp Pathol, 2013; 6(11): 2350- 2356.

