Orbital Exenteration: What Place in the Therapeutic Arsenal of Malignant Tumors of the Orbit?
Ayoub Bakhil*, Hugues Buckat, Nawfal El Hafidi, Moussa Boubacar, Hicham Sabani, Lahcen Khalfi, Jalal Hamama and Karim El Khatib
Department of Maxillofacial Surgery, Mohammed V Military Hospital Rabat, Mohammed V university, Morocco
Received Date: 07/03/2025; Published Date: 21/04/2025
*Corresponding author: Ayoub Bakhil, Department of Maxillofacial Surgery, Mohammed V Military Hospital Rabat, Mohammed V university, Rabat, Morocco
Abstract
Introduction: Orbital exenteration is a disfiguring surgical procedure involving removal of the entire orbital contents, including the periosteum. It is indicated primarily in tumor pathology, Through a series of cases and a review of the literature, we will discuss the place of exenteration and the reconstruction procedures.
Material and Method: Retrospective study carried out on patients operated on in our training for orbital exenteration with a review of the literature Results 12 files were collated of patients operated on for a malignant tumour of the orbit, with an average age of 65 and a sex ratio of 1.5, the histological type was basal cell carcinoma, with enlarged exenteration in 8 patients, with reconstruction in most cases by a Temporal muscle and by epithesis in two patients
Conclusion: The indication for orbital exenteration has recently been called into question by studies that have shown the absence of benefit in terms of overall survival, but it remains the only surgery that allows local carcinological control.
Keywords: Exenteration; Reconstruction; Palpebral tumour
Introduction
Orbital exenteration is a anatomically and psychologically demanding surgical procedure, involving removal of the entire orbital contents by subperiosteal dissection. The first exenteration surgery is said to have been performed by Bartisch in 1583.
It is mainly indicated for malignant pathology of the orbit, its contents or neighbouring tissues invading the orbit. Palpebral carcinomas with signs of clinical or radiological invasion are the main indication for exenteration in our practice, dominated by basal cell carcinomas, squamous cell carcinomas and sebaceous carcinomas, followed by malignant tumours of the eyeball. At present, exenteration is rarely indicated for benign conditions, except for infections.
The lack of benefit in terms of overall survival, and the development of new medical treatments in recent years, tend to call into question this disfiguring procedure. Through a series and a review of the literature, we will discuss the current place of exenteration in the therapeutic arsenal of malignant tumors of the orbit.
Patients and Methods
We collated patient medical records operated on in our department between 2017 and 2024 and collected the different patient and tumour data (histological type, location, treatment and follow-up).
We included in this study patients who had undergone surgery for orbital exenteration of a malignant tumour. Patients who were lost to follow-up or whose records could not be analysed were excluded. We also carried out a bibliographical search on the following databases: Pubmed, Googlescholar, clinicalkey using the keywords: orbital exeteration, palpebral tumor, orbital reconstruction.
Results
We collected 12 patients who underwent orbital exenteration, all for malignant tumors. The mean age was 65 years with a male to female ratio of 1.5. All patients reported excessive sun exposure.
11 patients had palpebral cutaneous carcinoma and only one patient had conjunctival melanoma. The carcinomas were dominated by basal cell carcinoma (7 patients), followed by squamous cell carcinoma (4 patients), the most common site being the lower eyelid.
Therapeutic decisions were made during multidisciplinary consultations based on the presence of clinical and radiologic signs of invasion for cutaneous palpebral carcinoma (Figure 1). All patients underwent surgery under general anesthesia, with total exenteration in 4 patients and extended exenteration to adjacent soft tissues and bone walls in 8 patients (Figure 2).

Figure 1: Squamous cell carcinoma of the lower eyelid.

Figure 2: Orbital exenteration extended to the side wall.
Only one patient benefited from homolateral parotid lymph node curage for advanced squamous cell carcinoma associated with parotid adenopathies, while the anatomopathological results of the surgical specimens showed insufficient margins in 3 patients operated on for squamous cell carcinoma, who benefited from neoadjuvant radiotherapy within 6 weeks.
All our patients were reconstructed in a single-stage operation after extemporaneous control of the margins. 8 patients were reconstructed using a temporalis muscle flap (Figure 3), completed by a Mustarde flap for reconstruction of the skin plane (Figure 4), and 4 cases were reconstructed using a fascia temporalis flap for those two patients who received an epithesis implant.

Figure 3: Temporalis muscle flap reconstruction.

Figure 4: Skin reconstruction using a MUSTARDE flap.
Follow-up was instituted on a regular basis, with a minimum of 6 months and a maximum of 86 months. During this follow-up, we noted 4 cases of local recurrence (Figure 5), which were managed with radiochemotherapy. 6 patients survived to one year, and 4 to 5 years.
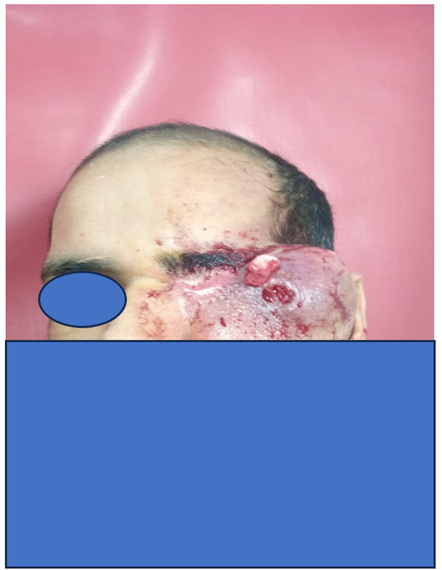
Figure 5: Locally advanced recurrence of squamous cell carcinoma.
Discussion
Orbital exenteration is a radical surgical procedure involving the removal of the eye and associated structures within the orbit. It is typically reserved for severe cases of malignancies or infections that are unresponsive to other treatments. This procedure, while life-saving, results in significant disfigurement and functional impairment.
The indications for orbital exenteration are increasingly debatable, but it remains the treatment of choice in the management of malignant tumors of the orbit or neighboring tumors with intraorbital extensions, and more rarely, severe infections of the face [1,2].
Basal cell carcinomas of the eyelids are the leading cause of orbital exenterations, followed by squamous cell carcinomas, retinoblastomas and orbital melanomas. [3], orbital exenteration can be categorized into several types, including lid and conjunctiva sparing anterior exenteration, lid sparing anterior exenteration, total exenteration, and extended exenteration, the choice of exenteration type is tailored to the patient's specific condition and the extent of the disease [4].
Reconstruction of the exenteration cavity is variable, with multiple techniques available, the choice of which depends on the surgical team, the extent of the exenteration and the exposure of noble elements, notably the dura mater, which requires immediate coverage. In addition to the patient's general condition, the most commonly used muscle flap is the temporalis muscle flap, which fills the residual cavity, allowing neo-adjuvant radiotherapy to be performed in a timely manner if indicated. [5] directed healing is still possible with plugging from the residual bone this technique allows easier prosthetic rehabilitation and easier oncological monitoring but delays adjuvant radiotherapy and prolongs the convalescence period [6].
The small number of cases in the published series of exenteration procedures, together with the great heterogeneity of malignant tumours in terms of histology, location and operators: oculoplasticians, ENT and maxillofacial surgeons, makes it difficult to compare the efficacy of exenteration with that of conservative treatment..
A metanalysis published in 2016 showed a survival rate after orbital exenteration for a malignant tumor showeda time to median (50%) survival for all patients was 78.4 months. The 1-year survival rate was 93.4% and the 5-year survival rate was 54.1%. Although not statistically significant, notable differences were found in the interval to death with respect to the identification of perineural invasion, lymphovascular invasion, and histopathologic features. The review of published studies suggested a difference in the histologic features and location of the disorder treated, the extent of orbital exenteration undertaken, and the method of reconstruction between the ophthalmology and nonophthalmology surgical disciplines [7] orbital exenteration remains the surgical technique that provides optimal control of the cancerous disease, thus avoiding local recurrence. [8,9], systemic survival after orbital exenteration compared with conservative treatment studies show no difference [10] but no randomized controlled study has been conducted in this area, given the rare nature of orbital exenteration.
The emergence of targeted therapies for cutaneous carcinomas [11] and melanomas is set to revolutionize the management of these tumors and may make it possible to adopt more conservative approaches ( eye-sparing ) and avoid exenteration, which is disfiguring surgery [12,13].
Currently, most surgical teams recommend prosthetic reconstruction for morphological reasons and for better monitoring of recurrence [14], except that in cases of enlarged exenteration with exposure of the meninges or deep structures of the face, a filling with a muscle flap seems well suited, since it completes the treatment with radiotherapy if indicated within 6 weeks [11]. In our series, most cases were reconstructed using a muscle flap, for two reasons: firstly, the extent of the excision, and secondly, the patient's socio-economic status, which does not allow for expensive prosthetic rehabilitation.
From our point of view, orbital exenteration still retains its place in the therapeutic protocol, provided that the therapeutic decision is taken on the basis of clinical, radiological and histological arguments in a specialized centre and during a multidisciplinary consultation meeting, and with the patient's consent. Orbital exenteration has shown its efficacy in ensuring optimal local tumour control, facilitating follow-up and morphological rehabilitation, and improving patients' quality of life.
Conclusion
Orbital exenteration is a major surgery in terms of morphology, function and also psychology, which is currently still indicated in advanced malignant orbital tumours where it is impossible to preserve the eyeball. The techniques for reconstructing the cavity are variable and must be adapted to the loss of substance, the terrain and the surgeon's experience. The indication for orbital exenteration has recently been called into question by studies that have shown the absence of benefit in terms of overall survival, but it remains the only surgery that allows local carcinological control.
References
- Rahman I, Cook AE, Leatherbarrow B. “Orbital exenteration: a 13 year Manchester experience,” J. Ophthalmol., 2005; 89(10): pp. 1335–1340. doi: 10.1136/BJO.2004.062471.
- Simon GJB, Schwarcz RM, Douglas R, Fiaschetti D, McCann JD, Goldberg RA. “Orbital exenteration: one size does not fit all,” J. Ophthalmol., 2005; 139(1): pp. 11–17. doi: 10.1016/J.AJO.2004.07.041.
- Nandi S, Chhebbi M, Mandal A. “A Systematic Review Article on Orbital Exenteration: Indication, Complications and Reconstruction Methods.,” Indian J. Otolaryngol. head neck Surg. Publ. Assoc. Otolaryngol. India, 2022; 74(Suppl 2): pp. 1183–1191. doi: 10.1007/s12070-020-02270-5.
- Baum SH, Oeverhaus M, Saxe F, Mohr C. “Modified types of orbital exenteration, survival, and reconstruction,” Graefe’s Arch. Clin. Exp. Ophthalmol., 2020; 258(10): pp. 2305–2312. doi: 10.1007/s00417-020-04812-7.
- Atabay K, Atabay C, Yavuzer R, Demirkan F, Latifoğlu O. “One-stage reconstruction of eye socket and eyelids in orbital exenteration ,” Plast. Reconstr. Surg., 1998; 101(6): pp. 1462–1463. doi: 10.1097/00006534-199805000-00005.
- Jategaonkar AA, Vernon D, Byrne PJ. “Regional Reconstruction of Orbital Exenteration Defects.,” Plast. Surg., 2019; 33(2): pp. 120–124. doi: 10.1055/s-0039-1685475.
- Hoffman GR, Jefferson ND, Reid CBA, Eisenberg RL. “Orbital Exenteration to Manage Infiltrative Sinonasal, Orbital Adnexal, and Cutaneous Malignancies Provides Acceptable Survival Outcomes: An Institutional Review, Literature Review, and Meta-Analysis,” Oral Maxillofac. Surg., 2016; 74(3): pp. 631–643. doi: 10.1016/j.joms.2015.09.019.
- Wong JCL, Thampy R, Cook A. “Life expectancy following orbital exenteration,” J. Ophthalmol., 2015; 99(1): pp. 1–4. doi: 10.1136/BJOPHTHALMOL-2013-304436.
- Matsuo T, Ohara N, Namba Y, Koshima I, Ida K, Kanazawa S. “Ophthalmic artery embolization as pretreatment of orbital exenteration for conjunctival squamous cell carcinoma,” Intervent. Radiol., 2009; 32(3): pp. 554–557. doi: 10.1007/S00270-008-9413-6/METRICS.
- Reyes C, Mason E, Solares CA, Bush C, Carrau R. “To preserve or not to preserve the orbit in paranasal sinus neoplasms: a meta-analysis.,” Neurol. Surg. B. Skull Base, 2015; 76(2): pp. 122–128. doi: 10.1055/s-0034-1390403.
- Lavasidis G, Tzamalis A, Tsinopoulos I, Ziakas N. “Exploring vismodegib: A non-surgical breakthrough in the management of advanced periocular basal cell carcinoma,” Cancer Treat. Res. Commun., 2024; 39: p. 100796. doi: 10.1016/j.ctarc.2024.100796.
- Martel A, et al. “Orbital exenteration: an updated review with perspectives,” Ophthalmol., 2021; 66(5): pp. 856–876. doi: 10.1016/J.SURVOPHTHAL.2021.01.008.
- Sagili S, Malhotra R. “Orbital exenteration: indications, techniques and complications,” Expert Rev. Ophthalmol., 2016; 11(3): pp. 201–213. doi: 10.1080/17469899.2016.1186544.
- Martel A, Hamedani M, Lagier J, Bertolotto C, Gastaud L, Poissonnet G. “Does orbital exenteration still has a place in 2019?,” J. Fr. Ophtalmol., 2020; 43(2): pp. 152–174. doi: 10.1016/j.jfo.2019.04.021.

