Intratumoral Hemorrhage in Posterior Fossa Tumors after Ventriculoperitoneal Shuneting: Case Report
Nabil Nia*, Mdarhri Mehdi, Oualid Mohammed Hmamouche, Marouane Hammoud, Faycal Lakhdar, Mohammed Benzagmout, Khalid Chakour and Mohammed El Faiz Chaoui
Department of Neurosurgery, Hassan II University Hospital, Fez, Morocco
Received Date: 17/03/2025; Published Date: 18/04/2025
*Corresponding author: Nabil Nia, Department of Neurosurgery, Hassan II University Hospital, Fez, Morocco
Abstract
Spontaneous hemorrhage into an intracranial neoplasm is relatively rare, usually occurring in metastatic lesions, glioblastomas, or pituitary adenomas. Hemorrhage into posterior fossa tumors is extremely rare [1-4]. We report a case of fatal hemorrhage in a posterior fossa lesion located in the 4th ventricle, suggestive of an ependymoma, following the insertion of internal ventricular drainage in a 14-year-old child.
Keywords: Ependymoma; Fourth ventricle; Hemorrhage; Shunt
Introduction
Massive intratumoral hemorrhages following Cerebrospinal Fluid (CSF) diversion for a posterior fossa tumor with hydrocephalus are rare. We report our experience with one patient and have reviewed the literature.
Case Presentation
This is a 14-year-old child with no significant medical history, admitted for progressively worsening gait disturbances over the past 4 months, aggravated two weeks ago by a syndrome of intracranial hypertension characterized by headaches and vomiting. On examination, the child was conscious (GCS 15), with equal and reactive pupils; there were no sensory or motor deficits, but a cerebellar statico-kinetic syndrome was observed.
A Computed Tomography (CT) scan revealed a cerebellar lesion located in the 4th ventricle, which showed enhancement after contrast medium injection, suggesting an ependymoma, as well as marked dilation of the 3rd ventricle (Figure 1). On the same day, the child underwent a ventriculoperitoneal (VP) shunt procedure.
The surgical procedure went smoothly; in the immediate postoperative period, the patient developed bilateral mydriasis with absent brainstem reflexes, prompting an immediate brain CT scan, which revealed an intratumoral hemorrhage causing upward transtentorial herniation and a reduction in ventricular dilation. The patient was then transferred to the intensive care unit. He remained in a coma for 2 days and then died of cardiorespiratory arrest.
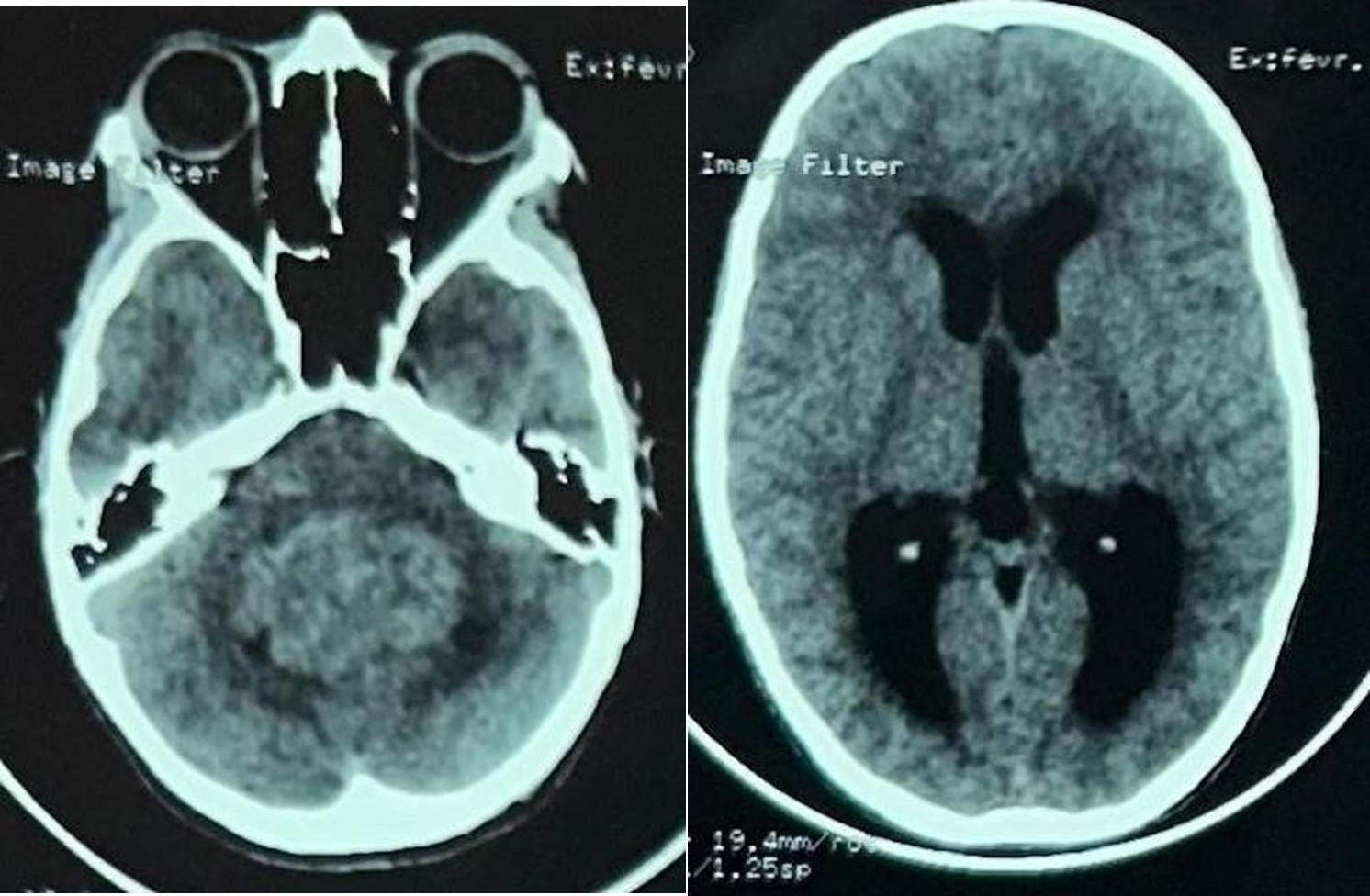
Figure 1: CT scan showing a tumor process of the 4th ventricle with extension to the vermis and cerebellar parenchyma bilaterally, suggestive of an ependymoma; complicating active triventricular hydrocephalus upstream.
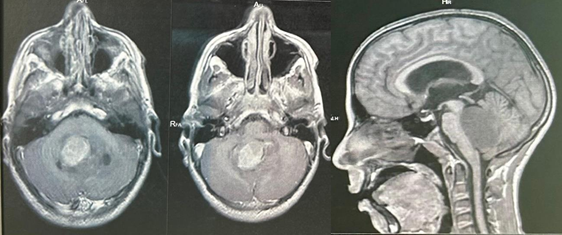
Figure 2: CT scan showing a tumor process of the 4th ventricle with extension to the vermis and cerebellar parenchyma bilaterally, suggestive of an ependymoma; complicating active triventricular hydrocephalus upstream.
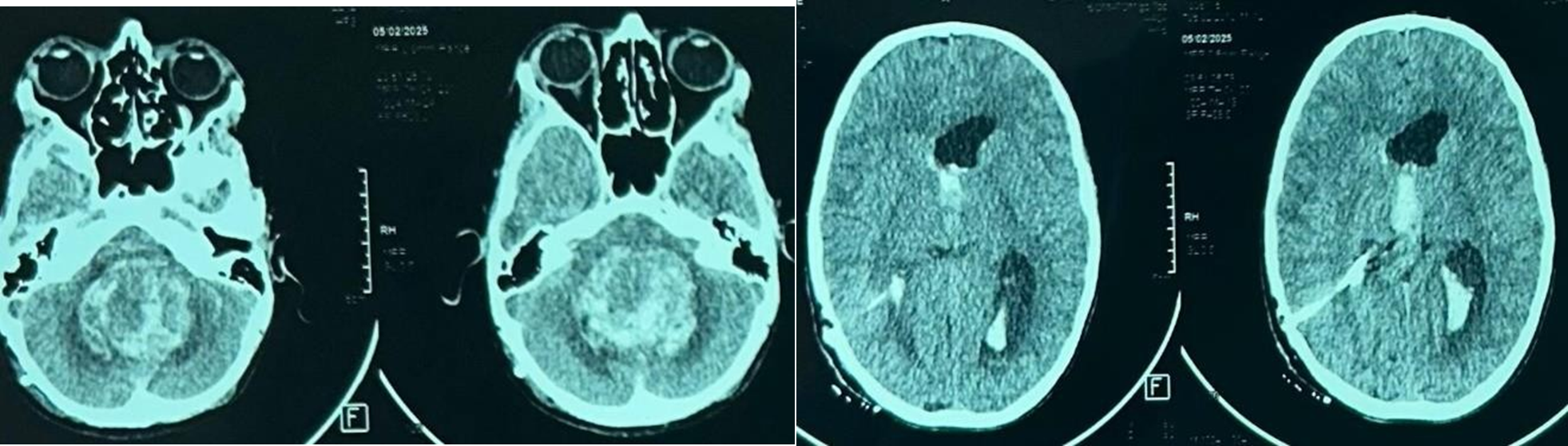
Figure 3: CT scan showing Hemorrhage within the tumor after shunt insertion.
Discussion
On reviewing the literature about intratumoral hemorrhage in children [4,5], we observed an unexpectedly high inci dence of an ictal presentation. Hemorrhage is reported to occur in highly vascularized tumors, such as metastases. med- ulloblastomas. and neuroblastomas. Although ependymoma is a highly vascularized tumor. only a few cases of hemorrhage in ependymoma have been reported. Our patient had a tumor that does not often bleed. The sudden and dramatic clinical deterioration after ventricular decompression suggests that VP shunt insertion was the cause of intratumoral bleeding. In spite of avoiding cerebrospinal fluid leak during the operation and inserting a medium pressure valvular shunt, operation upset the delicate balance of pressures between the supra- and infratentorial compartments. Only three other cases of hem- orrhage after VP shunting and two cases of hemorrhage after the insertion of an external drainage system have been reported [12,13].
This case stirs up again the controversy about the use of precraniotomy shunts before tumor operation and the choice between internal and external shunts. Almost all published data indicate that precraniotomy shunts benefit children who are ill from hydrocephalus due to posterior fossa tumor by improving their general condition before operation and by reducing operative mortality and morbidity. This agreement lessens the significance of the controversy and argumentation for and against precraniotomy shunts. The major arguments against precraniotomy internal shunts are: (a) the risk of upward herniation after shunt insertion [6,7], (b) the possibility of transshunt metastasis [8]. (c) the belief that cortico- steroids restore patency to an obstructed cerebrospinal fluid pathway [9] and (d) the fact that most children do not need a permanent shunt after tumor removal.
Advances in technology have made external drainage com- parable to internal shunting in risk and benefit for children who need hydrocephalus treatment before craniotomy, so that in the U.S. the use ofa precraniotomy shunt seems to be anachronistic.
The risk of infection. generally accepted to be between 4% and I 0% [14], is an important argument for those, and we are among them, who use permanent shunts, although it has been reported that the risk of infection with current external drain- age systems is equivalent to that with internal shunts [10].
the occurrence of hemorrhage in ependymoma after VP shunting, although infrequent [4,11], is a complication that must be borne in mind when deciding between an internal and an external shunt.
Conclusion
Major intratumoral hemorrhage following CSF diversion for posterior fossa tumors is an important cause of immediate deterioration and contributes to morbidity and mortality, even for benign tumors.
References
- Coulon R, Till lntracranial ependymomas in children-a review of 43 cases. Childs Brain, 1977; 3: 154-168.
- Lamers BJM. Clinical and diagnostic appearance of tumors of posterior fossa in childhood: Results of a retrospective coopera- tive Adv Neurosurg, 1983; 175-179.
- Pierluca P. Les ependymomes de la fosse cerebral posterieure. Neurochirurgie, 1977; 23(suppl I): 111-147.
- Wakai S, Yamakawa K, Manaka S, Takakura Spontaneous intracranial hemorrhage caused by brain tumor: Its incidence and clinical significance. Neurosurgery, 1982; 10: 437-444.
- Laurent J, Bruce DA, Schut Hemorrhagic brain tumors in pediatric patients. Childs Brain, 1981; 8: 263-270.
- Epstein F, Murali R. Pediatric posterior fossa tumors: Hazards of the "preoperative" Neurosurgery, 1978; 3: 348-350.
- Raimondi A, Tomita Hydrocephalus and infratentorial tu- mors-incidence, clinical picture and treatment. J Neurosurg, 1981; 55: 174-182.
- Hoffman H, Hendrick B, Humphreys R. Metastasis via V-P shunt in patients with J Neurosurg, 1976; 44: 562.
- Epstein F, Murali R. Pediatric posterior fossa tumors: Hazards of the "preoperative" Neurosurgery, 1978; 3: 348-350.
- Richard K, Heller R, Frowein Internal shunt or perioperative pressure-controlled ventricular fluid drainage in children and juveniles with infratentorial tumors. Adv Neurosurg, 1983; 249-255.
- Waga S, Shimizu T, Shimosaka S, Tochio Intratumoral hemorrhage after a ventriculoperitoneal shunting procedure. Neurosurgery, 1981; 9: 249-252.
- Vaquero J, Cabezudo JM, De Sola G, Nombela L. Intratumoral hemorrhage in posterior fossa tumors after ventricular drainage: Report of two cases. J Neurosurg, 1981; 54: 406-408.
- Waga S, Shimizu T, Shimosaka S, Tochio Intratumoral hemorrhage after a ventriculoperitoneal shunting procedure. Neurosurgery, 1981; 9: 249-252.
- Alvarez-Garijo Mengual MY. Infection rate with and without prophylactic antibiotic therapy after shunt insertion for hydro- cephalus. Monogr Neurol Sci, 1982; 8: 66-68.

