Rare Cases of Supra- and Infra-Tentorial Extradural Hematomas: A Review of Two Clinical Cases
Zahir Ilias*, Stitou Kaoutar, Hmamouch Mohamed Oualid, Hammoud Marouane, Mohammed Benzagmout, Fayçal Lakhdar, Khalid Chakour and Chaoui El faiz Mohammed
Department of Neurosurgery University Hospital Hassan II Fez- Morocco
Received Date: 10/03/2025; Published Date: 15/04/2025
*Corresponding author: Zahir Ilias, Department of Neurosurgery University Hospital Hassan II Fez- Morocco; Stitou Kaoutar, Department of Neurosurgery, University Hospital of Fez, Morocco
Abstract
Extradural hematoma (EDH) is a rare but serious complication of brain injury. EDH located supra- and infra-tentorially is even less common, with only a few studies dedicated to this subject. The clinical signs are often nonspecific, but early identification of supra- and infra-tentorial EDH, coupled with swift treatment, is essential to prevent further complications. We report two cases of a supra- and infra-tentorial EDH.
Keywords: Extradural; Hematoma; Infra-tentorial; Supra-tentorial
Introduction
Extradural hematoma (EDH) is a rare complication of brain injury, accounting for approximately 1%–4% of traumatic brain injuries [1,2]. The occurrence of EDH in the supra- and infra-tentorial regions is extremely uncommon. Clinical symptoms are often nonspecific, and in some cases, acute EDH may present with no symptoms initially. It has been reported that occipital fractures are associated with 84% of EDH cases. With the introduction of Computed Tomography (CT) scans, diagnosing the condition has become easier, and patient prognosis has significantly improved. This paper presents two cases of an EDH located supra- and infra-tentorially.
Illustrative Case 1
A 30-year-old patient, with no notable medical history, is admitted to the emergency department for the management of a head injury following a road traffic accident. He is admitted with a Glasgow Coma Scale (GCS) of 6 and right-sided anisocoria.
The initial brain CT scan reveals a right parieto-occipital extradural hematoma with a maximum thickness of 38 mm, corresponding to a right parietal fracture line extending towards the ipsilateral temporal region.
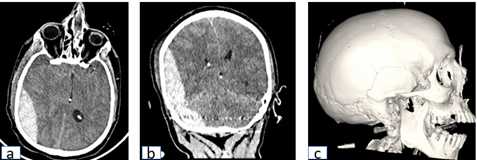
Figures a-c: Preoperative non-contrast brain CT, axial section (a) and coronal section (b), showing a right parieto-occipital extradural hematoma of 38mm, and a 3D bone window image (c) showing a right parietal fracture line.
The patient is quickly admitted to the operating room. He underwent a parieto-occipital craniectomy with complete evacuation of the extradural hematoma and suspension of the dura mater.
The patient was admitted to the neurosurgical intensive care unit for postoperative monitoring. Postoperative head CT showed resolution of the hematoma.
On the 3rd postoperative day, the patient was extubated with a normal neurological examination
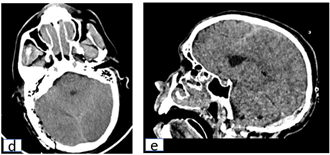
Figures d, e: Postoperative non-contrast brain CT, axial section (d) and sagittal section (e), showing complete evacuation of the hematoma.
Illustrative Case 2
8-year-old child, no medical history, admitted to pediatric emergency for management of a head injury following a 2-meter fall. On examination, the child is conscious with a GCS of 15, experiencing headaches, stable hemodynamically and respiratory-wise, with no sensory-motor deficits or cerebellar syndrome.
The initial brain CT scan reveals a right extradural hematoma in the posterior cranial fossa with supratentorial extension measuring 28mm, associated with a ipsilateral occipital fracture.
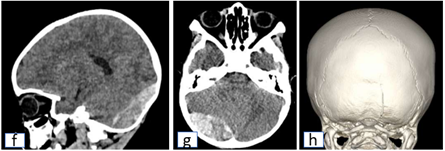
Figures f-h: Preoperative non-contrast brain CT, sagittal section (f) and axial section (g), showing a right extradural hematoma in the posterior cranial fossa of 28mm with supratentorial extension and a 3D bone window image (h) showing a right occipital fracture.
The child was quickly taken to the operating room, where a flap centered on the hematoma was performed, and the hematoma was evacuated with dural suspension.
Post-operatively, the patient was extubated with a resolution of the headaches and a normal neurological examination.
The follow-up CT scan shows a complete resolution of the hematoma.
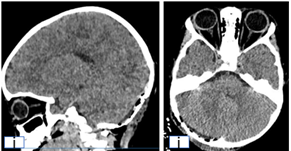
Figures i,j: Postoperative non-contrast brain CT, sagittal section (i) and axial section (j), showing complete evacuation of the hematoma.
Discussion
A simultaneous acute supra- and infra-tentorial EDH is a rare case which appears both in front of lateral sinus and behind it. The cases are generally associated with lateral sinus injury [4,5]. EDH of the posterior fossa is mainly seen in young-aged patients, which representing 55% of the reported series of Jang et al [6]. The higher incidence in children may be attributed to the rich vascularization of their dura and diploe, as well as the fact that cranial trauma in children often affects or involves the occipital region.
The cause of trauma can vary, ranging from high-energy impacts to less severe events. Unlike EDH in the anterior and middle cranial fossae, supra- and infra-tentorial EDH do not present with distinct clinical symptoms. Clinical manifestations of supra-tentorial EDH may include headache, nausea, vomiting, memory loss, hemiparesis, and loss of consciousness, while infra-tentorial EDH may present with neck pain, cranial nerve palsy, and cerebellar dysfunction [1]. The absence of clinical signs does not rule out the diagnosis.
Hooper classified traumatic posterior fossa EDH into three stages: acute, subacute, and chronic, based on the onset of symptoms. Acute EDH occurs within the first 24 hours after trauma, subacute EDH develops between the 2nd and 7th days, and chronic EDH appears more than 7 days after the trauma [1]. Acute EDH is typically associated with severe trauma, with the primary symptom being impaired consciousness or coma. In subacute EDH, common signs include intracranial hypertension and compression of the cerebellum or brainstem, which is often seen in children, as in our case. The chronic form is rare and typically presents similarly to an infra-tentorial expansive process, usually managed with follow-up rather than surgery. The posterior fossa EDH is usually associated with occipital fracture [1,3,6,7]. The fracture cannot be visible on radiological exam and CT scan but can be seen during operation.
Surgery remains the gold standard for treating supra- and infra-tentorial EDH, involving hematoma evacuation via craniotomy. Perioperative evaluation provides an opportunity to identify the source of the bleeding. According to the study of Upadhyay, et al [4] the origin of bleeding could be arterial from the posterior meningeal artery or venous from the lateral sinus or the torcula.
Many authors [1,6,8] recommended combined supra-tentorial and sub-occipital craniotomy and leave a bone bridge over the transverse sinus for dural suspension. Nasi, et al [8] reported that the source of bleeding of supra- and infra-tentorial EDH is venous bone fracture with diploe bleeding (50%), transverse/sigmoid sinus injury (22%), oozing meningeal venous vessel (8%), detachment of transverse sinus without wall injury (6%), and unknown in the other cases. Some authors suggested providing conservative treatment for small non-compressive hematomas but strict clinical and radiological follow-up is mandatory [6].
The supra- and infra-tentorial EDH prognosis has improved since the advancement of the CT scan. The bad prognosis factors of supra- and infra-tentorial EDH including initial or secondary consciousness disorders associated parenchymal lesions. The reported mortality rates were various. Aji et al [1] in their literature review reported that in general, the overall mortality of supra- and infra-tentorial EDH is 17%, the operative mortality rate is 14%, and the morbidity rate is 6% and a better prognosis can be achieved in patients under 10 years of age. After literature review, Nasi et al [8] reported that overall mortality of supra- and infra-tentorial EDH is 4%; 92% of the supra- and infra-tentorial EDH patients obtained favorable outcomes (Glasgow outcome score (GOS) 4–5) after surgery, while 8% of them obtained an unfavorable outcome (GOS 1–3) [8].
EDH is a true neurosurgical emergency, and cases located in the supra- and infra-tentorial regions are rare. Due to the lack of specific clinical signs for supra- and infra-tentorial EDH, greater attention should be given to diagnosing pediatric trauma patients with occipital impact. Early diagnosis through CT scan and timely hematoma removal are key factors in ensuring a favorable prognosis.
References
- Aji YK, Apriawan T, Bajamal AH. Traumatic supra- and infra-tentorial extradural hematoma: case series and literature review. Asian J Neurosurg, 2018; 13: 453–457. doi: 10.4103/ajns.AJNS_282_16.
- Nagi S, Ben Reguiga M, Kaddour C. Extradural hematoma of posterior fossa: report of four pediatric cases. J Pediatrie Pueric, 2007; 20: 29–32.
- Roda JM, Giménez D, Pérez-Higueras A. Posteror fossa epidural hematomas: a review and synthesis. Surg Neurol, 1983; 19: 419–424. doi: 10.1016/0090-3019(83)90138-6.
- Upadhyay P, Srivastav A. Supra- and infratentorial acute extradural haematoma. India J Neurotrauma, 2007; 4: 59–61.
- Askeri G, Akademisi T, Cerrahisi S. Supra- and infratentorial acute epidural haematoma: a case report. Surgery, 2009; 2: 161–163.
- Jang JW, Lee JK, Seo BR. Traumatic epidural haematoma of the posterior cranial fossa. Br J Neurosurg, 2011; 25: 55–61. doi: 10.3109/02688697.2010.520759.
- Xiaoyu W, Guoping L. Surgical treatment of supra- and infratentorial epidural hematoma. Turk Neurosurg, 2013; 23: 299–303. doi: 10.5137/1019-5149.JTN.5043-11.
- Nasi D, Laccarino C, Romano A. Surgical management of traumatic supra and infratentorial extradural hematomas: our experience and systematic literature review. Neurosurg Rev, 2019: 1–9. doi: 10.1007/s10143-019-01083-7.

