An Extremely Rare Case of Extradural Hematoma Following Stereotactic Brain Biopsy
Kaoutar Stitou*, Baderddine Mohammadine**, Oualid Mohammed Hmamouche,Marouane Hammoud, Faycal Lakhdar, Mohammed Benzagmout, Khalid Chakour and Mohammed El Faiz Chaoui
Department of Neurosurgery, University Hospital of Fez, Morocco
Received Date: 08/03/2025; Published Date: 14/04/2025
*Corresponding author: Dr. Stitou Kaoutar*, Department of Neurosurgery,University Hospital of Fez, Morocco; Dr. Baderddine Mohammadine**, Department of Neurosurgery,University Hospital of Fez, Morocco
Abstract
Stereotactic brain biopsy is a minimally invasive procedure widely used for the diagnosis of deep-seated brain lesions. Although generally considered safe, it is not without risks.
We report a rare complication of extradural hematoma following a stereotactic brain biopsy in a 32-year-old female patient with a high-grade glial tumor. This case highlights the diagnostic and therapeutic challenges encountered during the management of a deep-seated brain lesion and the importance of early recognition and management of complications.
Keywords: Extradural hematoma; Stereotactic brain biopsy; High-grade glial tumor
Introduction
Stereotactic brain biopsy is a minimally invasive procedure used for the diagnosis of intracranial lesions. Although considered relatively safe, it is not without risks, including hemorrhage, infection, and neurological deficits [1]. Here, we present a case complicated by an extradural hematoma following stereotactic biopsy, emphasizing the importance of prompt diagnosis and surgical intervention.
Case Presentation
A 32-year-old female patient with no prior medical history presented one year ago with complaints of headaches and decreased visual acuity. Upon clinical examination, the patient was conscious, hemodynamically and respiratory stable, with no sensory or motor deficits. Ophthalmological examination revealed visual acuity of 9/10 bilaterally and papilledema stage II bilaterally. Laboratory tests, including coagulation profile and platelet count, were within normal ranges, ruling out any coagulation disorders.
The brain CT scan revealed the brain CT scan with a non-contrast parenchymal window revealed a slightly spontaneously hyperdense heterogeneous lesion in the pineal region, which enhances after contrast injection, responsible for triventricular hydrocephalus (Figure 1).
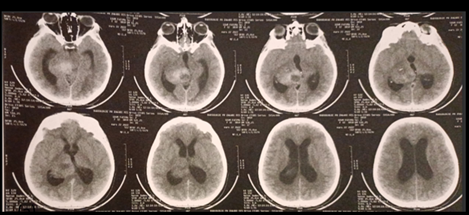
Figure 1: The brain CT scan with a non-contrast parenchymal window revealed a slightly spontaneously hyperdense heterogeneous lesion responsible for triventricular hydrocephalus.
The brain MRI (Figure 2) Identified a well-defined, roughly rounded lesion in the right thalamus measuring 43 mm x 30 mm x 37 mm, with hyperintensity on T1 and hyperintensity on T2 sequences. The lesion compressed the third ventricle and had intimate contact with the pineal gland, causing midbrain compression and hydrocephalus. Spectroscopy findings included increased choline, decreased N-acetylaspartate (NAA), and a choline/creatinine ratio of 2.3, suggestive of a high-grade tumor.
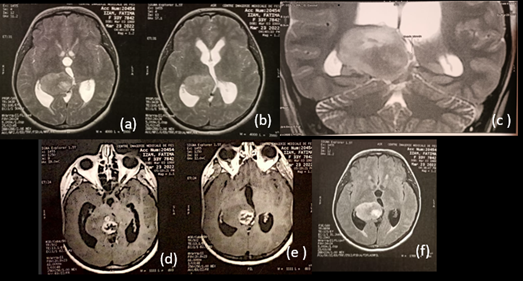
Figure 2: Brain MRI revealed a roughly rounded lesion in the right thalamus measuring 43 mm x 30 mm x 37 mm, (a)(b) hyperintense on T2 axial slice and (c) coronal slice, (d)(e) enhancing with contrast, and (f) heterogeneous hyperintense on FLAIR sequence. The lesion compressed the third ventricle and was in intimate contact with the pineal gland, causing midbrain compression and hydrocephalus."
The patient underwent ventriculocisternostomy to relieve hydrocephalus, followed by an initial stereotactic biopsy, which was inconclusive. A repeat stereotactic biopsy was performed six months later.
Following the second biopsy, the patient experienced severe headaches. A control CT scan revealed a 17-mm extradural hematoma in the right parietal region (Figure 3).
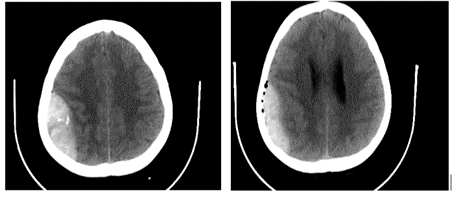
Figure 3: A control CT scan revealed a 17-mm extradural hematoma in the right parietal region.
Surgical evacuation of the hematoma via right parietal craniectomy was performed, resulting in good postoperative recovery (Figure 4).
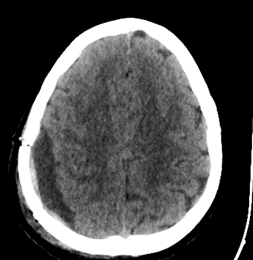
Figure 4: Post-operative scan showing evacuation of the left parietal extra-Dural hematoma.
Histopathological analysis confirmed a high-grade glial tumor. the patient received radiotherapy and chemotherapy. A one-year follow-up CT-scan demonstrated significant regression of the lesion (Figure 5).
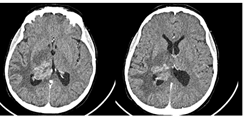
Figure 5: Axial brain scan with contrast injection, performed one year after stereotactic biopsy, demonstrating lesion regression.
Discussion
Stereotactic biopsy is a cornerstone in the diagnosis of intracranial lesions, particularly deep-seated tumors. Hemorrhagic complications occur in 0.7-4.3% of cases, with symptomatic hematomas being even rarer [2]. Factors predisposing to hemorrhage include vascularized tumors, coagulopathy, and procedural trauma [3].
In this case, preoperative blood tests, including coagulation studies, were normal, eliminating coagulopathy as a contributing factor. The absence of coagulation abnormalities suggests a mechanical cause related to the biopsy procedure itself, such as vessel injury or dura mater damage during needle insertion [4]. Repeat biopsies, as in this case, may further increase the risk due to prior tissue disruption and scarring [5].
Extradural hematomas are particularly rare following stereotactic biopsy, as most hemorrhages tend to be intraparenchymal. The development of an extradural hematoma may be linked to dural perforation or leakage of blood into the epidural space through a small cortical breach [6]. Another possible mechanism is injury to a branch of the middle meningeal artery, which could contribute to hematoma formation in the extradural space.
Management of extradural hematomas requires rapid diagnosis through imaging and prompt surgical evacuation when clinically indicated. Timely intervention, as demonstrated in this case, is critical to prevent neurological deterioration and improve outcomes [7].
This case highlights several key considerations for reducing the risk of hemorrhagic complications: Meticulous planning with imaging to avoid highly vascularized regions. Use of intraoperative image guidance to optimize needle placement. Close postoperative monitoring, particularly in symptomatic patients, with early imaging to detect hemorrhage. Availability of neurosurgical teams for urgent intervention in case of complications.
Despite the occurrence of a postoperative complication, this patient experienced good neurological recovery and long-term improvement following oncological treatment. This outcome underscores the importance of a multidisciplinary approach in managing intracranial tumors.
Conclusion
This case highlights the potential complications associated with stereotactic brain biopsy and underscores the need for meticulous perioperative care and prompt management of complications. Multimodal treatment approaches combining surgery, radiotherapy, and chemotherapy can achieve favorable outcomes.
References
- Smith JS, et al. "Complications of Stereotactic Brain Biopsy: A Review of 500 Cases." Neurosurgery, 2005.
- Zrinzo L. "Hemorrhagic Complications in Stereotactic Brain Biopsies." Acta Neurochirurgica, 2008.
- Hall WA, et al. "Factors Influencing Hemorrhage Risk in Stereotactic Biopsy." Journal of Neurosurgery, 1999.
- Sawaya R, et al. "Intracerebral Hemorrhage Following Biopsy of Intracranial Tumors." Neurosurgery, 1992.
- Levy ML, et al. "Repeat Biopsies and Their Associated Risks in Intracranial Lesions." Journal of Neuro-Oncology, 2000.
- Rahmathulla G, et al. "Epidural Hematomas Following Brain Surgery: Mechanisms and Management." Neurosurgery Quarterly, 2013.
- Woodworth GF, et al. "Safety and Efficacy of Stereotactic Brain Biopsies: A Systematic Review." Neurosurgical Review, 2007.

