Skull Deformation Revealing a Pediatric Cerebral Hydatid Cyst
Nabil Nia*, Mdarhri Mehdi, Oualid Mohammed Hmamouche, Marouane Hammoud, Faycal Lakhdar, Mohammed Benzagmout, Khalid Chakour and Mohammed El Faiz Chaoui
Department of Neurosurgery, Hassan II University Hospital. Fez Morocco
Received Date: 03/03/2025; Published Date: 10/04/2025
*Corresponding author: Nabil Nia, Department of Neurosurgery, Hassan II University Hospital. Fez Morocco
Abstract
Background: Cerebral hydatidosis is a rare parasitic infection caused by Echinococcus granulosus, primarily affecting children in endemic regions. While intracranial hydatid cysts typically present with symptoms of increased intracranial pressure or neurological deficits, skull deformation as the main presenting feature is exceptionally rare.
Case Presentation: We report the case of a 5-year-old child presenting with a three-month history of progressive right temporal swelling associated with headaches. Clinical examination revealed a firm, non-inflammatory right temporal mass. Imaging studies, including CT and MRI, demonstrated a large unilocular cystic lesion causing significant chronic mass effect on the temporal bone, leading to its deformation. Given the intraoperative discovery of severe skull thinning, a modified craniotomy approach utilizing a traditional drill and Gigli saw was employed to ensure safe cyst removal while preserving bone integrity.
Discussion: Skull deformity due to the chronic expansion of an intraparenchymal hydatid cyst is an unusual manifestation of cerebral hydatidosis, with very few cases documented in pediatric patients. This case underscores the importance of considering hydatid disease in the differential diagnosis of unexplained cranial deformities, particularly in endemic regions.
Conclusion: This report highlights an atypical presentation of cerebral hydatid cyst with skull deformation as the primary complaint. Early imaging and tailored surgical strategies are crucial for optimal management and prevention of complications.
Keywords: Cerebral hydatid cyst; Skull deformation; Pediatric neurosurgery; Craniotomy; Hydatid disease; MRI; Surgery
Introduction
Cerebral hydatidosis, caused by Echinococcus granulosus, is a rare parasitic infection predominantly affecting children in endemic regions [1]. Typically, it presents as a cystic intracranial lesion with symptoms such as headaches, vomiting, hemiparesis, seizures, behavioral changes, or, in some cases, skull deformity [2].
Our case is distinctive because the primary reason for consultation was skull deformation, a manifestation that is infrequently reported in the literature. This clinically evident deformity was identified intraoperatively, necessitating a modified craniotomy approach utilizing the soft usage of a traditional drill and Gigli saw to ensure the safe removal of the cyst. Such a presentation underscores the importance of considering cerebral hydatidosis in children presenting with skull deformities, even in the absence of other neurological symptoms.
Case Report
We report the case of a 5 years old, admitted to our department with the presentation of a three-month history of right temporal swelling associated with a progressive headache. He had a history of contact with dogs.
The first examination showed Fully conscious (GCS 15/15), no focal deficits. Cranial Examination: A right temporal firm, oval swelling (3cm × 4cm) was palpable without signs of inflammation. Motor Function: Normal muscle tone and reflexes.
Injected CT scan showed a unilocular cystic lesion, not enhanced after injection of contrast product. The CT also showed a deformation of the temporal bone due to chronical mass effect on the right side that corresponds to the clinical evident swelling on the temporal region (Figure 1).
MRI examination showed unilocular cystic lesion, hyperintense on T2-weighted and FLAIR images. No enhancement with gadolinium, confirming its non-solid nature with Compression of the middle cerebral artery (MCA) without significant stenosis. Effacement of the lateral ventricle with associated mild hydrocephalus. Engagement under the falx cerebri and early uncal herniation (Figure 2).
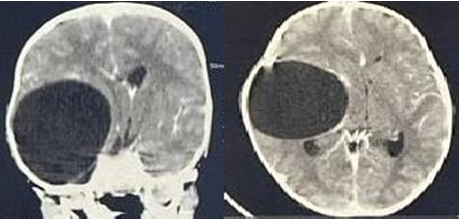
Figure 1: Preoperation CT scan revealed a large cystic right parietal and temporal lobe with Skull Deformation.
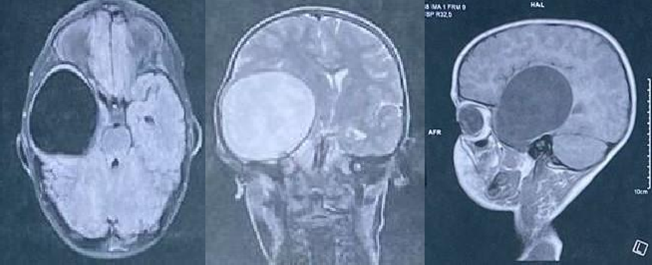
Figure 2: A unilocular cystic lesion, hyperintense on T2-weighted and FLAIR images. No enhancement with gadolinium, confirming its non-solid nature.
Surgical management
A right temporal craniotomy was planned to excise the hydatid cyst. However, intraoperative discovery of severe skull thinning and deformation required an extremely delicate bone flap removal to avoid fragmentation. The surgical approach followed these steps:
Scalp Incision and Exposure:
- A right temporo-parieto-frontal incision was performed to provide adequate exposure while minimizing cosmetic impact.
- Careful dissection of the scalp and periosteum was undertaken to avoid damaging the underlying thinned
Craniotomy with Bone Preservation Strategy:
- A traditional drill was used instead of a high-speed burr drill, ensuring controlled and soft penetration of the already weakened bone.
- The Gigli saw technique was chosen for osteotomy to avoid excessive mechanical stress that could lead to unintended fractures.
- Bone removal was performed in a stepwise manner, maintaining structural stability until the cyst was adequately
Hydatid Cyst Excision (Dowling-Orlando Technique Adaptation):
- Once the dura was opened, the cyst was identified within the temporal
- En bloc excision was carefully attempted, using minimal manipulation to prevent
- Saline irrigation and hydro-dissection techniques facilitated atraumatic separation of the cyst from surrounding brain tissue (Figure 3, 4).
- Gentle aspiration of surrounding cerebrospinal fluid helped decompress the area, reducing pressure on the cyst capsule.
Hemostasis and Closure:
- Hemostasis was meticulously achieved, ensuring no residual cyst fragments or
- The bone flap was repositioned and reinforced, taking into account the pre-existing skull
- The scalp was closed in layers, and a sterile dressing was
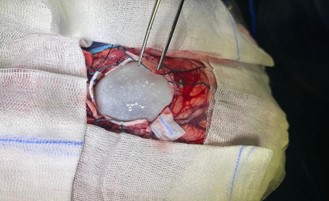
Figure 3: Intra-operative microsurgical dissection to remove a large hydatid cyst.

Figure 4: Large hydatid cyst post-evacuation.
Postoperative considerations
- The patient was monitored for signs of intracranial hypertension or
- Albendazole therapy was initiated postoperatively to reduce the risk of
- A follow-up CT scan confirmed complete excision without complications (Figure 5)
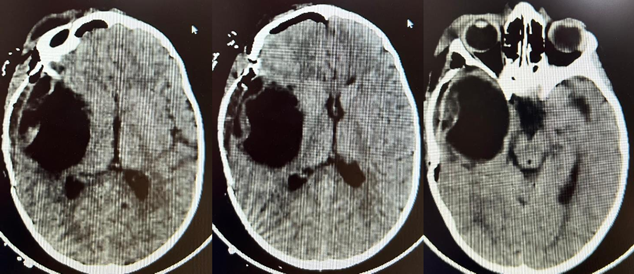
Figure 5: Post-operative brain scan.
Discussion
Intracranial localisation of hydatid cyst is an uncommon neurosurgical condition, affecting more frequently children and young adults. [3] Typically affecting the sylvian artery territory, cerebral hydatidosis generally have a supratentorial location [4]. Clinical manifestations generally result from mass effect on the surrounding brain region and high intracranial pressure causing a wide variety of symptoms depending on the exact location (Seizure, focal deficit, headache, vision loss …) [5].
MRI is the key for diagnosis, typically showing a a cystic lesion with CSF similar signal intensity with no associated oedema [6]. Imaging can mimic other cystic lesion as arachnoid cyst, cystic tumours or even cystic glioma, thus the importance of a well done anamnesis, clinical examination and complementary imaging to identify other lesions, gathering risk factors clinic-radiological elements in favour of our diagnosis [7].
Besides osseous hydatidosis [8], which itself is exceedingly rare at the cranial level (3% of all bone hydatidosis) [9]; Cranial vault deformities as a consequence of intraparenchymal hydatid cyst mass effect is exceptional and very few authors have reported this deformity in paediatric population [10].
Conclusion
This case highlights an exceptional presentation of cerebral hydatid disease, where skull deformation was the primary reason for consultation, rather than the more commonly observed symptoms of intracranial hypertension or neurological deficits. The chronic mass effect exerted by the intraparenchymal cyst led to progressive thinning and remodeling of the temporal bone, a rare occurrence in pediatric patients. The intraoperative discovery of severe skull thinning required a modified craniotomy approach using a traditional drill and Gigli saw, ensuring safe cyst removal while preserving bone integrity. Given the rarity of such presentations, clinicians should consider hydatid disease in the differential diagnosis of unexplained cranial deformities within the pediatric population, particularly in endemic regions. Early imaging, precise surgical planning, and adjunctive antiparasitic therapy remain crucial in optimizing patient outcomes and preventing recurrence.
Compliance with ethical standards:
Disclosure of conflict of interest: The authors no conflict of interest.
Statement of informed consent: Informed consent was obtained from all individual participants included in the study.
References
- Eckert J, Deplazes P. “Biological, epidemiological, and clinical aspects of echinococcosis, a zoonosis of increasing concern,” Clin Microbiol Rev, 2004; 17(1): 107–135. doi: 10.1128/CMR.17.1.107-135.2004.
- Hmada S, et , “Pediatric brain hydatid cyst about two cases: Case report,” Ann Med Surg (Lond), 2022; 78: p. 103806. doi: 10.1016/j.amsu.2022.103806.
- Turgut M Ed. Hydatidosis of the Central Nervous System: Diagnosis and Treatment. Berlin, Heidelberg: Springer Berlin Heidelberg, 2014. doi: 10.1007/978-3-642-54359-3.
- Alshoabi SA, et “Hydatid Disease: A Radiological Pictorial Review of a Great Neoplasms Mimicker,” Diagnostics, 2023; 13(6): Art. no. 6. doi: 10.3390/diagnostics13061127.
- Turgut M. “Intracranial hydatidosis in Turkey: its clinical presentation, diagnostic studies, surgical management, and outcome. A review of 276 cases,” Neurosurg Rev, 2001; 24(4): pp. 200–208. doi: 1007/s101430100168.
- Yaghoobi MH, Sabahi MM, Zibaei M. “Imaging features of the lungs hydatid cyst disseminated into the brain and spleen,” Radiology Case Reports, 2019; 14(8): pp. 903–905. doi: 10.1016/j.radcr.2019.05.005.
- Abbasi B, et al. “Computed tomography and magnetic resonance imaging of hydatid disease: A pictorial review of uncommon imaging presentations,” Heliyon, 2021; 7(5): e07086. doi: 10.1016/j.heliyon.2021.e07086.
- Limaiem F, et al. “Hydatid cyst of the cranial vault,” J Infect Dev Ctries, 2009; 3(10): pp. 807–810. doi: 3855/jidc.48.
- Behari S, Banerji D, Phadke RV, Shukla S, Krishnani N, Chhabra DK. “Multiple infected extradural parasellar hydatid cysts,” Surg Neurol, 1997; 48(1): pp. 53–57. doi: 10.1016/s0090-3019(97)85702-3.
- Khaldi S Mohamed, Kallel J, Khouja N. “Brain hydatidosis: report on 117 cases,” Child’s Nervous System, 2000; 16(10–11): 765–769. doi: 10.1007/s003810000348.

