Guillain-Barré Syndrome Presenting a Extubation Failure in the ICU
Kenza Damaan, Salma Fatihi*, Sabah Benhamza, Mohamed Lazraq, Youssef Miloudi and Abdelhak Bensaid
Intensive Care Unit, 20 August Hospital 1953, University Hospital Centre IBN Rochd, Casablanca, Morocco
Received Date: 27/02/2025; Published Date: 03/04/2025
*Corresponding author: Salma Faihi, Intensive Care Unit, 20 August Hospital 1953, University Hospital Centre IBN Rochd, Casablanca, Morocco
Abstract
Guillain-Barré Syndrome (GBS) is a rare but serious autoimmune disorder characterized by acute flaccid paralysis. Early recognition in the ICU is crucial, especially when it presents atypically, such as through extubation failure .
A 29-year-old female was admitted to the ICU for severe pneumonia. Following mechanical ventilation and planned extubation, the patient demonstrated extubation failure due to undiagnosed neuromuscular weakness, later confirmed as GBS.
This case highlights the diagnostic challenges and the importance of neurological assessment in ICU.
Keywords : Extubation failure ; Guillain-barré syndrome ; Intensive Care Unit
Background
Guillain-Barré Syndrome (GBS) is the most prevalent acute immune-mediated paralytic neuropathy [1]. It is characterized by acute-onset, progressive muscle weakness and areflexia, typically presenting as a symmetric ascending paralysis that can progress to respiratory muscle involvement, necessitating mechanical ventilation in severe cases [2,3]. The pathogenesis of GBS involves an aberrant immune response, usually triggered by a preceding infection, leading to immune-mediated damage to the peripheral nerves and nerve roots [4]. Campylobacter jejuni, cytomegalovirus, Epstein-Barr virus, Mycoplasma pneumoniae, and more recently, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), have been identified as frequently implicated infectious agents in GBS [5,6].
GBS is a heterogeneous disorder with several clinical variants, including Acute Inflammatory Demyelinating Polyneuropathy (AIDP), Acute Motor Axonal Neuropathy (AMAN), and acute motor and sensory axonal neuropathy (AMSAN) [7]. The prognosis varies depending on the subtype and severity, with some patients experiencing complete recovery and others suffering from long-term disability [8]. Management primarily involves supportive care, with Intravenous Immunoglobulin (IVIG) and plasma exchange being the mainstays of treatment, as they have been shown to shorten recovery time and improve outcomes [9].
Respiratory failure is a critical complication of GBS, occurring in approximately 20-30% of cases, often due to progressive weakness of the diaphragm and intercostal muscles [10,11]. Patients requiring mechanical ventilation pose significant challenges in the intensive care unit (ICU), particularly concerning timely extubation. Extubation failure, defined as the inability to sustain spontaneous breathing after removal of the endotracheal tube, is commonly attributed to pulmonary or cardiac causes, but neuromuscular disorders such as GBS should also be considered [12].
Although GBS-related respiratory muscle weakness is well recognized in the acute phase, subclinical neuromuscular involvement can persist, making weaning from mechanical ventilation more complex [13]. Failure to recognize ongoing diaphragmatic dysfunction may lead to premature extubation and reintubation, increasing the risk of ICU-acquired complications, prolonged hospitalization, and mortality [14,15]. Therefore, a thorough neurological assessment is essential in patients with unexplained weaning difficulties.
This case report highlights the importance of considering subclinical respiratory muscle weakness in patients who experience extubation failure. We discuss the clinical course, diagnostic challenges, and implications for ICU management in such cases.
Case Presentation
The patient is a 29-year-old female with Marfan syndrome complicated by mitral insufficiency and aortic aneurysm, managed on Bisoprolol 1.25 mg/day. Her past medical history includes psychomotor delay, ambulatory difficulties due to scoliosis and bilateral coxarthrosis (status post bilateral total hip arthroplasty in 2017), and a family history of ICU hospitalization for hypoxemic pneumonia a week prior our patient’s admission. She was admitted to the ICU for acute respiratory failure secondary to severe pneumonia.On ICU admission, respiratory examination revealed a respiratory rate of 20 breaths per minute, oxygen saturation of 62% under a high-concentration mask, with suprasternal and intercostal retractions and bilateral basithoracic rhonchi. Hemodynamically, the patient was tachycardic (130 bpm) with a blood pressure of 100/60 mmHg. Neurologically, her Glasgow Coma Scale (GCS) was 13/15, indicating mild impairment; however, the remainder of the neurological exam was limited but initially showed no deficits.
Initial arterial blood gas analysis demonstrated a PaO₂/FiO₂ ratio of 42 mmHg, acidemia (pH 7.26), hypercapnia (PaCO₂ 61.9 mmHg), HCO₃⁻ 28 mmol/L, and lactate 1.25 mmol/L. Laboratory investigations revealed Hemoglobin of 14 g/dL, a white blood cell count of 7,320 e/mm³ with low lymphocyte count (830 e/mm³), markedly elevated C-reactive protein (CRP = 461.7 nmol/L), and procalcitonin (PCT = 15ng/mL) (Table 1). COVID serologies, sputum cultures, and multiplex PCR were negative. Chest imaging confirmed severe pneumonia (Figure 1).
Table 1: Initial laboratory investigations.
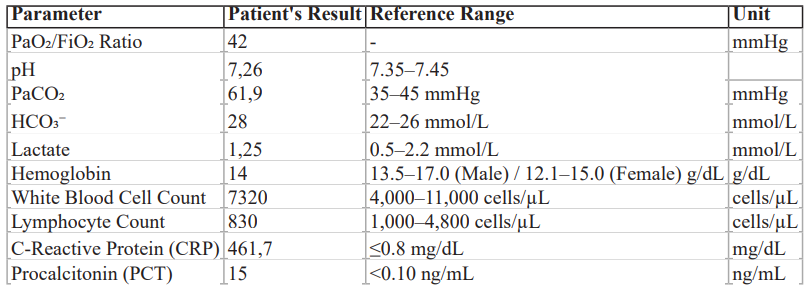
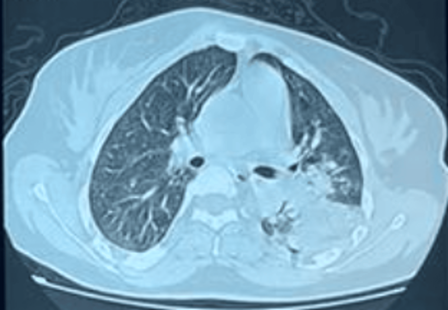
Figure 1: CT Scan demonstrating severe pneumonia.
The patient was immediately intubated due to hypoxic respiratory failure and Antibiotic therapy was initiated. She managed on mechanical ventilation with appropriate sedation and supportive care. No initial signs of neuromuscular weakness were noted.
After 7 days of mechanical ventilation, she met standard extubation criteria (adequate oxygenation with PaO₂/FiO₂ > 200 (Table 2), hemodynamic stability, and resolution of pulmonary pathology as confirmed by chest imaging (Figure 2) and improved inflammatory markers). A spontaneous breathing trial (SBT) was successfully conducted for 45 minutes, and the patient was extubated on day 7.
Table 2: Ventilatory Parameters progression.
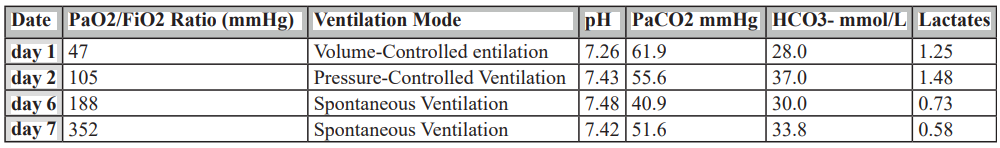
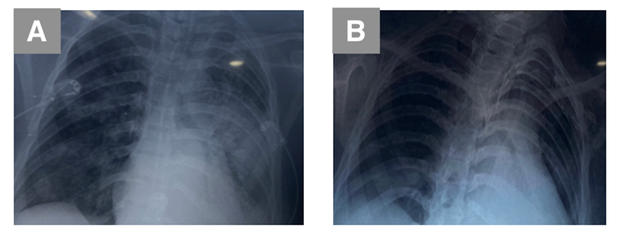
Figure 2: Illustrating respiratory improvement on imaging demonstrated by Chest X-Rays.
A: Chest X-Ray on day 1; B: Chest X-Ray on day 4
Within few minutes post-extubation, the patient developed respiratory distress, weak cough and poor secretion clearance.Non-invasive ventilation was initiated but proved ineffective. Due to progressive respiratory failure, reintubation was required within 2 hours.
On clinical examination, the patient showed no particular signs suggestive of respiratory or cardiac pathology. However the patient was tachycardic, with a heart rate of 100 bpm. The neurological examination revealed generalized flaccid weakness, more pronounced in the lower limbs and proximal muscles, accompanied by areflexia and bulbar involvement (absent cough reflex and dysphagia). Sensory involvement was minimal, with preserved pain sensation. Cerebrospinal fluid (CSF) analysis did not reveal albuminocytologic dissociation. Nerve Conduction Studies (NCS) / Electromyography (EMG) findings were consistent with demyelinating polyneuropathy, demonstrated by prolonged distal latencies and reduced conduction velocities.The study also revealed a sensorimotor axonal neuropathy with motor predominance, suggestive of GBS. Sural nerve sparing was noted, with better sural nerve amplitudes compared to the reduced sensory amplitudes in other explored nerve trunks-a typical finding in GBS.Imaging revealed right pulmonary embolism involving the ventral segmental branch of the right upper lobe artery and the paracardiac and medio-basal segmental branches of the right lower lobe artery, indicating an additional complication contributing to the patient's respiratory compromise and possibly exacerbating hypoxemia.
Based on clinical presentation, EMG/NCS findings, and CSF analysis, a diagnosis of GBS was confirmed. Immunotherapy was initiated with intravenous immunoglobulin (IVIG) at 0.4 g/kg/day for 5 days, as well as supportive care including close respiratory monitoring and physiotherapy. Sedation was minimized to accurately assess neuromuscular strength [9]. Moreover, despite prophylactic anticoagulation, CT Pulmonary Angiography confirmed a pulmonary embolism. Immediate Anticoagulation using Low-Molecular-Weight Heparin (LMWH) was initiated [8].
The patient showed a progressive recovery of bulbar functions, with a gradual return of both the cough reflex and swallowing ability (deglutition), indicating improvement in cranial nerve function and neuromuscular strength.Weaning from mechanical ventilation was initiated on day 15, with the patient successfully transitioned to oxygen therapy. Oxygen support was progressively reduced over the following days as respiratory function improved. By day 25, the patient was successfully weaned to room air. Neurological function continued to improve, with gains in muscle strength and functional abilities, consistent with a favorable response to the treatment for GBS and effective management as physical rehabilitation was initiated. The patient was discharged from the ICU on day 28. At follow-up, after 3 weeks, the patient demonstrated near-complete motor recovery.
Discussion
Importance of considering neuromuscular causes like GBS in unexplained extubation failure.
Extubation failure is a significant complication in critically ill patients, often leading to prolonged mechanical ventilation, increased ICU stay, and higher morbidity [12]. While respiratory and cardiac causes are the most common, neuromuscular disorders like GBS can present atypically and contribute to extubation failure [1]. This case highlights the critical role of neuromuscular assessment in patients with unexplained respiratory failure, particularly when standard extubation criteria are met but the patient fails to maintain adequate ventilation post-extubation.
Guillain-Barré Syndrome and Respiratory Failure
GBS is an acute immune-mediated polyneuropathy characterized by rapidly progressive weakness, areflexia, and, in severe cases, respiratory failure due to diaphragmatic and intercostal muscle involvement. Up to 30% of GBS patients require mechanical ventilation due to: respiratory muscle weakness, bulbar dysfunction (leading to impaired airway protection, dysphagia, and absent cough reflex) [9] and autonomic instability affecting respiratory drive [14].In this case, the patient's extubation failure was probably primarily due to respiratory muscle weakness and bulbar involvement (evidenced by the absent cough reflex and dysphagia), hallmark features of severe GBS [11].Electrophysiological studies confirmed the diagnosis, revealing sensorimotor axonal neuropathy with motor predominance, a finding consistent with acute motor axonal neuropathy (AMAN) . Notably, the absence of albuminocytologic dissociation in the initial CSF analysis does not exclude GBS, as this can be absent in the early stages of the disease [3].Timely intervention with immunotherapy improves prognosis [4].
Extubation Criteria and Neuromuscular Disorders
Traditional extubation criteria, such as adequate oxygenation, stable hemodynamics, and successful spontaneous breathing trials (SBT), may not reliably predict extubation success in patients with underlying neuromuscular weakness [12]. In GBS, even if ventilatory parameters appear sufficient during SBT, the respiratory muscles may not sustain prolonged spontaneous breathing, leading to post-extubation respiratory failure [15]. Furthermore, bulbar dysfunction increases the risk of aspiration, ineffective coughing, and secretion retention, compounding the risk of extubation failure. This case underscores the importance of: careful neuromuscular assessment before extubation and bedside evaluations of cough strength and swallowing to assess bulbar function.
Pulmonary Embolism as a Contributing Factor
The discovery of a pulmonary embolism (PE) further complicated the patient’s respiratory status. PE can exacerbate hypoxemia and increase the work of breathing, both of which can contribute to extubation failure [8]. In immobilized patients, especially those with neuromuscular weakness like GBS, the risk of venous thromboembolism (VTE) is significantly heightened [13]. The dual presence of GBS-related muscle weakness and PE-related hypoxemia created a complex pathophysiological scenario, leading to extubation failure. Early identification and management of PE with anticoagulation were essential in this patient’s recovery.
Differentiating GBS from ICU-acquired weakness
While both GBS and ICU-Acquired Weakness (ICUAW) present with neuromuscular impairment in critically ill patients, several key distinctions aid in their differentiation. GBS typically manifests with an acute onset and a characteristic ascending pattern of weakness, often accompanied by pronounced bulbar dysfunction and areflexia. In contrast, ICUAW generally develops insidiously during a prolonged ICU stay, presenting as a diffuse, symmetric weakness that lacks the distinctive progression and bulbar features of GBS. Electrophysiological studies are crucial in distinguishing the two: GBS usually exhibits demyelinating features or axonal involvement in certain variants, such as prolonged distal latencies and conduction block, whereas ICUAW shows a generalized reduction in muscle action potentials without specific demyelinating changes [7]. In this case, the rapid onset of severe neuromuscular deficits and supportive electrophysiological findings strongly favored a diagnosis of GBS over ICUAW [7]. This distinction was crucial in guiding the timely initiation of targeted immunotherapy [5].
Conclusion
This case underscores the critical role of Guillain-Barré Syndrome (GBS) as a potential cause of extubation failure in the ICU. While extubation failure is often attributed to respiratory or cardiac issues, this case highlights how undiagnosed neuromuscular weakness, specifically GBS, can impair respiratory muscles and bulbar function, leading to post-extubation respiratory distress.
Despite meeting standard extubation criteria, the patient’s inability to sustain spontaneous breathing was due to GBS-related muscle weakness and bulbar dysfunction. Early recognition of GBS through nerve conduction studies and electromyography, followed by timely treatment with intravenous immunoglobulin (IVIG), was crucial in facilitating recovery.
This case emphasizes the importance of considering neuromuscular disorders like GBS in unexplained extubation failure and highlights the need for thorough neurological assessments in critically ill patients to ensure appropriate diagnosis and management.
References
- Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016 ; 388: 717-727. 1016/S0140-6736(16)00339-1.
- van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain-Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol, 2014 ; 10: 469-482. 1038/nrneurol.2014.121.
- Asbury AK, Cornblath DR. Assessment of current diagnostic criteria for Guillain-Barré syndrome. Ann Neurol, 1990; 27: 21-24. 1002/ana.410270707.
- Hughes RA, Swan AV, van Doorn PA. Intravenous immunoglobulin for Guillain‐Barré syndrome. Cochrane Database Syst Rev, 2014; 2063. 1002/14651858.CD002063.pub6.
- van Koningsveld R, Steyerberg EW, Hughes RA, Swan AV, van Doorn PA, Jacobs BC. A clinical prognostic scoring system for Guillain-Barré syndrome. Lancet Neurol, 2007; 6: 589-594. 1016/S1474-4422(07)70130-8.
- Abu-Rumeileh S, Abdelhak A, Foschi M, Tumani H, Otto M. Guillain-Barré syndrome spectrum associated with COVID- 19: an up-to-date systematic review of 73 cases. J Neurol, 2021; 268: 1133-1170. 1007/s00415-020-10124-x.
- Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med, 2020; 46: 637-653. 1007/s00134-020-05944-4.
- Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet, 2012; 379: 1835-1846. 1016/S0140-6736(11)61904-1.
- Sharshar T, Chevret S, Bourdain F, Raphaël JC. Early predictors of mechanical ventilation in Guillain-Barré syndrome. Crit Care Med, 2000; 28: 881-885. 1097/00003246-200004000-00003.
- van Doorn PA, Ruts L, Jacobs BC. Clinical features, pathogenesis, and treatment of Guillain-Barré syndrome. Lancet Neurol, 2008; 7: 939-950. 1016/S1474-4422(08)70215-1.
- Lawn ND, Fletcher DD, Henderson RD, Wolter TD, Wijdicks EF. Anticipating mechanical ventilation in Guillain-Barré syndrome. Arch Neurol, 2001; 58: 893-898. 1001/archneur.58.6.893.
- American Thoracic Society, American College of Chest Physicians: ATS/ACCP Statement on weaning from mechanical ventilation. Am J Respir Crit Care Med, 2001; 163: 512-517. 1164/ajrccm.163.3.ats1-01.
- Benslimane A, Caumes E, Rozenberg F, et al. Guillain-Barré syndrome associated with pulmonary embolism: an underdiagnosed complication?. J Neurol, 2005; 252: 1421-1423. 1007/s00415-005-0857-2.
- Rabinstein AA, Wijdicks EF. Warning signs of imminent respiratory failure in neurological disorders. Lancet Neurol, 2004; 3: 755-762. 1016/S1474-4422(04)00919-1.
- Durand MC, Porcher R, Orlikowski D, et al. Clinical and electrophysiological predictors of respiratory failure in Guillain-Barré syndrome: a prospective study. Lancet Neurol, 2006; 5: 1021-1028. 1016/S1474-4422(06)70603-2.

