A Large Retrorectal Epidermoid Cyst: A Rare Cause of Chronic Abdominal Pain and Constipation
Amrharhe El Mehdi1,*, Mechhor Salma1, El Bacha Hicham1, Cherkaoui Malki Manal1, Benzzoubeir Nadia1, Sabbah Farid2 and Errabih Ikram1
1Medicine B Gastroenterology and Proctology Department, Ibn Sina University Hospital, Rabat, Morocco
2Department of General Surgery C, Ibn Sina University Hospital, Rabat, Morocco
Received Date: 11/02/2025; Published Date: 26/03/2025
*Corresponding author: Amrharhe El Mehdi, MD, Medicine B Gastroenterology Department, Ibn Sina University Hospital, Rabat, Morocco
Abstract
Retrorectal cysts are rare congenital anomalies arising from embryological remnants, with retrorectal epidermoid cysts being a subset that can cause chronic abdominal pain and bowel dysfunction. We report the case of a 27-year-old woman presenting with chronic left-sided abdominal pain and constipation. Imaging revealed a large biloculated retrorectal cyst (94 mm), necessitating surgical excision. A combined laparoscopic and Kraske approach was performed, achieving complete resection. Histological analysis confirmed an epidermoid cyst with no malignancy. The patient had an uneventful recovery, with complete symptom resolution and no recurrence at six months. This case underscores the importance of considering retrorectal cysts in chronic abdominal pain. MRI plays a crucial role in diagnosis and surgical planning. Complete excision remains the gold standard for preventing complications, with a multidisciplinary approach optimizing outcomes.
Keywords: Constipation; Chronic abdominal pain; Retrorectal cyst; Epidermoid cyst; Surgical excision; Kraske approach
Introduction
Retrorectal cysts are rare congenital anomalies derived from embryological remnants, with an estimated incidence of approximately 1 per 40,000 hospital admissions [1]. These lesions are more frequently observed in women and typically manifest between the third and fifth decades of life [2]. Although often asymptomatic, they may present with chronic abdominal pain, bowel dysfunction, or urinary symptoms depending on their size and location [3]. Imaging plays a crucial role in diagnosing these lesions, and surgical excision is the treatment of choice to prevent complications such as infection, rupture, or, rarely, malignant transformation [4]. We report a case of a large retrorectal epidermoid cyst diagnosed in a 27-year-old woman, managed through surgical excision.
Case Report
Ms. K. E, a 27-year-old educator with no significant medical, surgical, or family history, presented with chronic abdominal pain persisting for one year. The pain was predominantly localized to the left hypochondrium and left flank, intermittent, without mechanical characteristics, and not associated with significant digestive disturbances. The patient also reported chronic evacuation constipation, having approximately two bowel movements per week. No systemic symptoms such as fever or weight loss were noted.
Initial clinical examination revealed mild tenderness in the left lower abdomen, without any palpable mass or signs of peritoneal irritation. Routine laboratory tests, including complete blood count, liver and kidney function tests, and inflammatory markers, were within normal limits.
An abdominal ultrasound revealed a hypoechoic, heterogeneous mass measuring 68.7 x 94.32 mm in the retrorectal region (Figure 1). Pelvic MRI confirmed a biloculated, thin-walled lesion measuring 60 x 52 x 60 mm. The lesion infiltrated the anococcygeal ligament and was in close contact with the rectal wall and coccyx without evidence of malignancy (Figure 2-5).
The intervention was performed in two stages. Under general anesthesia, laparoscopic exploration revealed no signs of carcinomatosis or hepatic metastasis. Dissection of the mesorectum allowed access to the posterior plane up to the levator ani muscles. Due to the lesion’s low and posterior location, conversion to a Kraske approach was required. Through a left paramedian incision, retrorectal space access was achieved after anococcygeal ligament division. The mass was removed en bloc, preserving adjacent structures. Histological analysis revealed a cystic formation lined by mature squamous epithelium with a visible granular layer and a lumen filled with concentric keratin lamellae. Surgical resection achieved clear margins, with no signs of malignancy. The final diagnosis was a retrorectal epidermoid cyst.
The patient’s postoperative course was uneventful, with complete resolution of her abdominal pain and constipation. At a six-month follow-up, she remained asymptomatic, and no recurrence was detected on imaging.
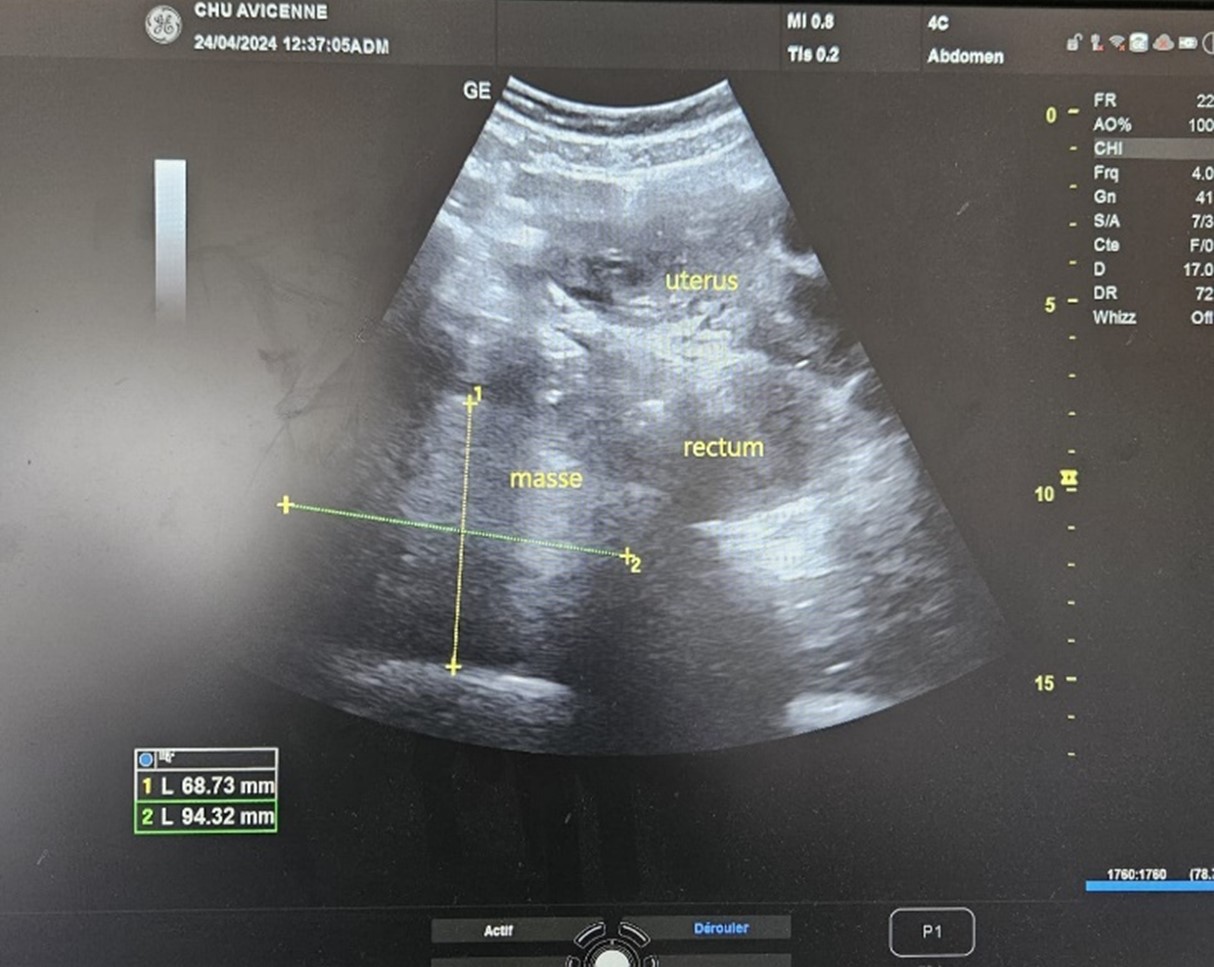
Figure 1: Ultrasound image showing a voluminous, well-defined, hypoechoic, and heterogeneous retrorectal mass.
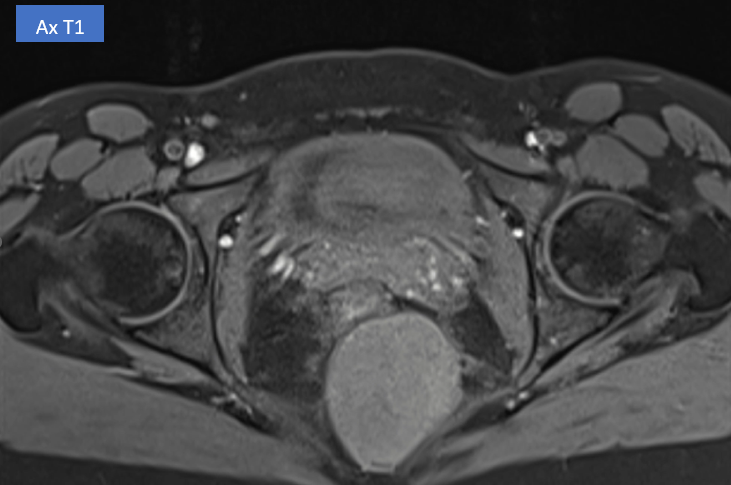
Figure 2: Axial T1-weighted MRI image showing a well-defined retrorectal mass with heterogeneous signal intensity, in close contact with the rectal wall and coccyx3.
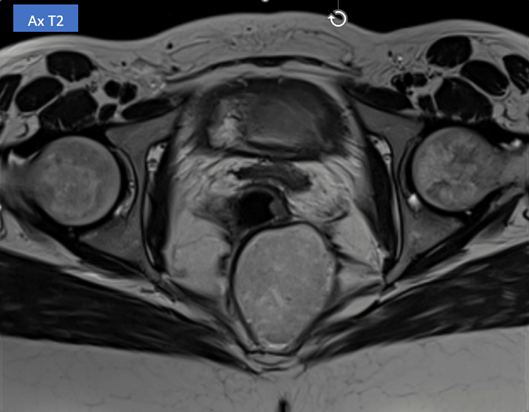
Figure 3: Axial T2-weighted MRI image showing a well-defined, biloculated retrorectal mass with heterogeneous high signal intensity, in close contact with the rectal wall and coccyx.

Figure 4: Sagittal T2-weighted MRI image showing a well-defined, retrorectal mass with heterogeneous high signal intensity, extending towards the coccyx and in close contact with the rectal wall.
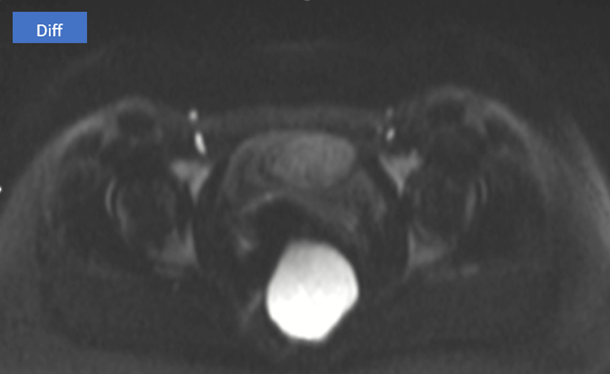
Figure 5: Axial diffusion-weighted MRI (DWI) image showing a hyperintense retrorectal mass, suggesting restricted diffusion, in close contact with the rectal wall and coccyx.
Discussion
Retrorectal epidermoid cysts are rare congenital anomalies derived from ectodermal remnants. They account for approximately 55-65% of retrorectal cystic lesions [4]. While generally benign, these lesions can lead to complications, including infection (seen in up to 30% of cases) or, more rarely, malignant transformation (<2%) [5]. The large dimensions observed in this case (up to 94 mm) are unusual and may increase surgical complexity and the risk of compression of adjacent structures, such as the rectum or coccyx.
MRI is particularly valuable for characterizing the biloculated nature and anatomical relationships of these lesions. In this case, MRI provided critical details on the cyst’s relationship with the rectum and coccyx, facilitating surgical planning. Complete surgical excision remains the treatment of choice, aiming to prevent complications and establish a definitive diagnosis [4].
The surgical approach for retrorectal cysts can vary based on the lesion’s size and location. The Kraske approach, used in this case, is particularly effective for lesions situated low in the retrorectal space. This combined abdominal and perineal approach allowed for optimal visualization and preservation of adjacent structures, minimizing surgical morbidity. Furthermore, early detection and thorough preoperative evaluation, as performed in this case, are critical in guiding surgical decision-making and improving outcomes.
The findings in this case are consistent with the literature regarding retrorectal epidermoid cysts and highlight the challenges posed by large lesions. According to Lev-Chelouche et al. [5], infection and rupture are the most common complications, often requiring prompt intervention. Malignant transformation, although rare (<2%), underscores the importance of complete surgical resection. Dozois et al. [6] emphasized the role of a multidisciplinary approach in achieving complete resection and minimizing postoperative complications.
Conclusion
This case highlights the importance of considering retrorectal cysts in the differential diagnosis of chronic abdominal pain and constipation, particularly in young patients without significant medical history. Comprehensive imaging, including MRI, is invaluable for diagnosis and surgical planning. A combined surgical approach, such as the Kraske technique, ensures complete resection and minimizes the risk of recurrence. Multidisciplinary collaboration is essential in managing these rare but potentially complex lesions. Long-term follow-up is recommended to detect any recurrence or late complications, ensuring optimal patient outcomes.
Conflict of interest: The author(s) declare that they have no conflicts of interest that could have inappropriately influenced them in the writing of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: No ethical approval was required for this article
Informed Consent: Written informed consent was obtained from the patient for the anonymized information to be published in this article.
Guarantor: Amrharhe El Mehdi
References
- Pomorski M, Bartoszewicz Z. Retrorectal cysts in adults: Presentation, diagnosis, and treatment. Int J Colorectal Dis, 2003;18(4):331-335.
- Glasgow SC, Birnbaum EH, Lowney JK, Kodner IJ. Retrorectal tumors: A comprehensive review of their anatomy, diagnosis, and treatment. Dis Colon Rectum, 2005; 48(8): 1581-1593.
- Baek SK, Hwang GS, Jeong SK, et al. Analysis of 18 cases of retrorectal tumors: Clinical characteristics and outcomes. Int J Colorectal Dis, 2016; 31(5): 1157-1163.
- Jao SW, Beart RW Jr, Spencer RJ, Reiman HM, Ilstrup DM. Retrorectal tumors: Mayo Clinic experience, 1960–1979. Dis Colon Rectum, 1985; 28(9): 644-652.
- Lev-Chelouche D, Gutman H, Goldman G, et al. Presacral tumors: A practical classification and treatment of a unique and heterogeneous group of diseases. Surgery, 2003; 133(5): 473-478.
- Dozois EJ, Dozois RR, Mathis KL. Presacral tumors: A review of their anatomy, diagnosis, and treatment. Dis Colon Rectum, 2013; 56(4): 510-520.

