Pituitary Apoplexy in a Pediatric Prolactinoma
Faraj Kaoutar*, Hmamouche Oualid Mohammed, Hammoud Marouane, Lakhdar faycal, Benzagmout mohammed, Chakour khalid and El Faiz Chaoui Mohammed
Department Neurosurgery, Centre hospitalier universitaire HASSAN II, Morocco
Received Date: 22/02/2025; Published Date: 21/03/2025
*Corresponding author: Faraj Kaoutar, Department Neurosurgery, Centre hospitalier universitaire HASSAN II, Morocco
Abstract
We report the case of a 78 –year-old male, still practicing pediatrician, with a medical history of recurrent respiratory infections for the past decades treated with antibiotics. He was referred with a suspicion of an endobronchial malignancy with endoluminal polypoid lesion occluding the right lower lobe bronchus. The tumor was exstirpated completely using laser cauterization. Tissue sampling showed fragments of mature hyaline cartilage with no evidence of malignancy, consistent with the diagnosis of chondroma. Chondromas are rare tumors of the tracheobronchial tree usually involving the lung parenchyma. They usually do not cause any symptoms, however in some cases, they may lead to non-specific symptoms like cough, pneumonia, hemoptysis, wheezing or dyspnea. Benign endobronchial tumors should be considered as a differential diagnosis in recurrent respiratory infections and evaluation with chest CT and bronchoscopy is warranted. Bronchoscopic resection is considered standard of care in cases without involvement of lung parenchyma.
Keywords: Benign tumors; Pulmonary lesion; Chondroma; Respiratory infections
Introduction
Pituitary tumor apoplexy is an acute clinical emergency caused by infarction or hemorrhage within a pituitary adenoma [1], representing a rare and potentially fatal endocrinological and neurosurgical emergency.
The most common clinical manifestations of pituitary apoplexy include the sudden onset of headaches, altered consciousness, severe visual disturbances, often in the form of chiasmal syndrome, oculomotor palsies, and endocrinological signs, particularly presenting as hypopituitarism.
Pituitary tumor apoplexy typically occurs in the fifth or sixth decade of life, with a slight male predominance. Pituitary apoplexy in adolescents is an extremely rare condition [2].
Macroadenomas, particularly non-functional prolactinomas, are most prone to apoplexy; however, cases of apoplexy in microadenomas have also been documented [3].
Pituitary adenomas in children are rare, with a prevalence of one per million (1:1,000,000). They represent less than 6% of all intracranial tumors in adolescents and less than 3% of supratentorial tumors in children. The most frequent type is prolactinomas (50%), which most commonly affect adolescent females [4].
Few case reports detailing pituitary tumor apoplexy in children have been published, resulting in a lack of consensus regarding appropriate management for this condition [5].
We report a case of a 12-year-old girl who presented with pituitary apoplexy secondary to a macroprolactinoma and was surgically treated via transnasal transsphenoidal approach. This article outlines the clinical, radiological, and biological presentation of prolactinoma in apoplexy, the therapeutic management protocol, and the postoperative clinical, biological, and radiological evolution.
Case Report
A 12-year-old female presented with a three-month history of headaches resistant to symptomatic treatment, accompanied by asthenia. One week later, she developed an intense thunderclap headache and sudden visual impairment in her left eye, without vomiting or other neurological deterioration. An ophthalmological examination revealed blindness in the left eye due to optic neuropathy and right divergent strabismus.
MRI findings suggested a macroadenoma in apoplexy, measuring 20 × 23 × 33 mm, compressing the optic chiasm and pituitary stalk, with intimate contact with both cavernous sinuses. The patient was subsequently referred to the emergency department.
On admission, she was conscious, oriented, and hemodynamically stable. Her vital signs were normal, with a Glasgow Coma Scale score of 15/15 and no sensory or motor deficits.
The patient's anthropometric measurements include a weight of 46 kg (+2.5 SD), a height of 134 cm (-1.5 SD), and a BMI of 25.6 kg/m²
Her pubertal development was normal (Tanner stage I for breast and pubic hair), with no spontaneous or induced galactorrhea.
Table 1: Hormonal laboratory findings.
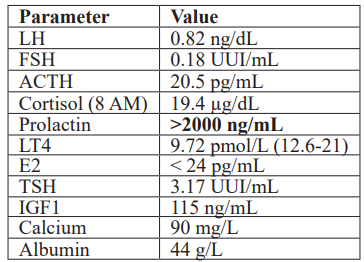
The patient was diagnosed with a prolactinoma, her hormonal biological assessment revealed an elevated prolactin level exceeding 2000 ng/ml, along with impairment of the thyrotropic axis, leading to supplementation with L-thyroxine at 25 µg/day. The other analyzed parameters were within normal ranges, as were the phosphocalcic and ionic profiles (Table 1).
MRI findings confirmed a macroadenoma with apoplexy, with hemorrhagic necrosis, compressing the optic chiasm and elevating the pituitary stalk, with intimate involvement of both cavernous sinuses (Figure 1, 2).
The patient underwent endoscopic endonasal transsphenoidal decompression of the macroadenoma. Intraoperatively, adenomatous tissue with hemorrhagic debris of different ages was identified. A subtotal tumor resection was achieved without notable surgical complications.
The histopathological analysis confirmed the diagnosis of an apoplectic prolactinoma, and the Ki-67 index was low, estimated at 1%.
Postoperatively, the patient showed progressive improvement in left eye vision, and prolactin level showed improvement, although it did not normalize completely, which required the use of dopamine receptor agonists.
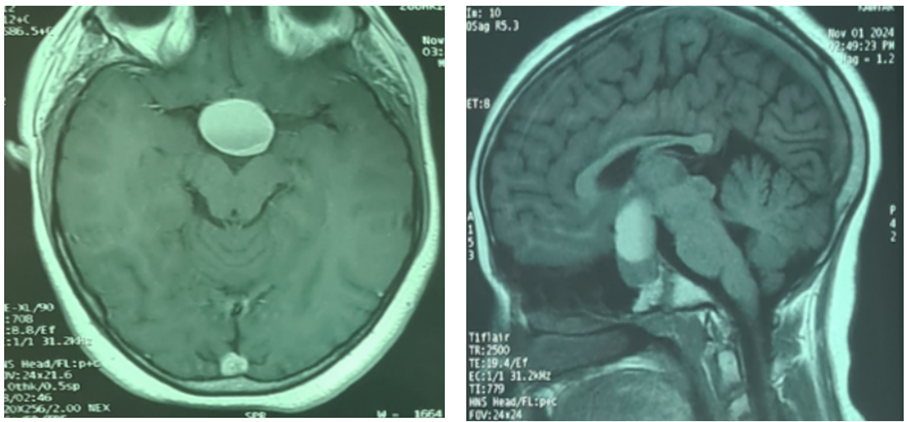
Figure 1: Sagittal and axial MRI images (T1-weighted) showing a mixed lesion, isointense to hypo intense in the anterior part of the sella and a hyperintense lesion occupying the posterior and superior part with suprasellar extension up to the floor of the third ventricle.
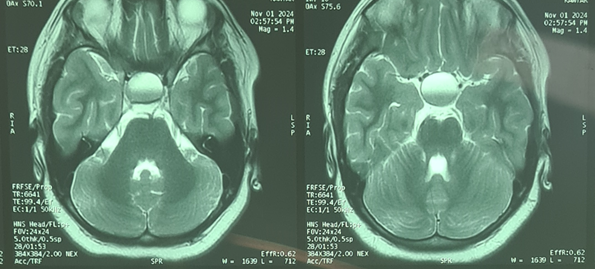
Figure 2: Axial T2-weighted images revealed a mixed lesion isointense lesion in the anterior part of the sella and hyperintense in the posterosuperior part. This fluid-fluid pattern is suggestive of hemorrhage.
Discussion
Hemorrhage associated with a pituitary tumor was first described by Bailey in 1898, but it was only in 1950 that Brougham et al. introduced the term "pituitary apoplexy" [7-8].
Pituitary apoplexy represents a rare medical emergency [6], even rarer in children and adolescents [9-15]; Due to the complexity and severity of the clinical presentation, requiring a multidisciplinary approach for the decision on conservative or surgical management. This involves emergency physicians, neuroradiologists, neurosurgeons, endocrinologists, and neuro-ophthalmologists.
Pituitary apoplexy has been found in 42.5% of pediatric and adolescent pituitary tumors [15]. Unlike in adult patients, where apoplexy is more common in non-functional adenomas, in children and adolescents, pituitary apoplexy is more frequently observed in functional adenomas, primarily prolactinomas (73.5%) [13, 15].
There is no gender predilection, it has been noted that apoplexy in prolactinomas is more frequent during puberty, with the average age at diagnosis being 16.6 ± 2.6 years in most cases reported in the literature, including the present case and the case of the team led by E. Culpin et al. [13] (average age of 14 years).
Prolactinomas present with both a tumor syndrome and endocrine symptoms, such as hyperprolactinemia, leading to decreased fertility, reduced libido, and galactorrhea [16-17]. However, diagnosing prolactinomas in children and adolescents presents unique challenges, as symptoms can be mistaken for age-related developmental variations. Their endocrinological symptoms are often overlooked or underestimated, which can delay diagnosis and treatment. In most cases, the diagnosis is made incidentally during an apoplexy of the adenoma [18].
The clinical presentation of pituitary apoplexy can be acute and severe, with significant neurological deficits, even leading to coma. Alternatively, it may be subacute, with milder symptoms developing over several days or weeks, depending on the speed of infarction or hemorrhage onset and the volume of bleeding. These factors influence the degree of compression on adjacent vascular and neuro-ophthalmological structures, as well as the pituitary gland itself [19].
The clinical picture supports the diagnosis of a pituitary tumor syndrome and an endocrine syndrome of hypersecretion or hypopituitarism. However, hypothalamo-pituitary imaging is essential to confirm the diagnosis.
MRI remains the gold standard for diagnosing pituitary apoplexy, with a sensitivity of approximately 90%. It detects hemorrhagic infarction, necrosis, optic chiasm compression, and adjacent vasculonervous structures. It also allows for assessing the degree of invasion according to the Knosp classification system [15].
MRI can also identify lesions that may mimic pituitary apoplexy, such as aneurysms, Rathke's pouch cysts, craniopharyngiomas, and mucoceles [20].
In the acute phase (0 to 7 days), a hypointense signal is observed on T2-weighted images, and an isointense or slightly hypointense signal is observed on T1-weighted images.
In the subacute phase (7 to 21 days), methemoglobin shortens T1 relaxation time, making the hemorrhage appear hyperintense on both T1 and T2 sequences.
In the chronic phase (> 21 days), the presence of hemosiderin and ferritin causes marked hypointensity on both T1 and T2 images [21].
CT imaging, although less sensitive, may be useful when MRI is unavailable or contraindicated, detecting sellar expansion in over 80% of cases, but can identifies only about 30% of pituitary apoplexies [22].
Ophthalmological evaluation, including visual acuity, visual field testing, and ocular motility, should be performed [23]. Additionally, a hormonal assessment should be conducted to detect any pituitary hormone deficiencies or hypersecretion conditions. A comprehensive metabolic workup is also necessary to assess electrolytes, renal function, liver function, coagulation, and complete blood count [23].
The ideal therapeutic approach for pituitary apoplexy in the young population is not clearly defined and remains controversial. There are very few case series of clinical pituitary apoplexy in the pediatric population that focus on treatment guidelines [24].
Applying adult treatment strategies to adolescent patients remains uncertain [25-26]. It is now widely acknowledged that a conservative approach using dopaminergic agonists should be the first-line treatment for the majority of adult prolactinomas presenting with apoplexy, given that surgery shows similar effectiveness to conservative management in terms of visual outcomes [13]. However, for children, no published guidelines exist for management.
Some authors advocate for early transsphenoidal surgical decompression in all patients, particularly those with neurological symptoms, visual disturbances, or those who do not tolerate the side effects of dopaminergic agonists. Others recommend a conservative approach in some cases, utilizing dopaminergic agonists [13-27].
There is, however, a correlation between the Ki-67 marker and the degree of tumor aggressiveness and proliferation, as well as resistance to treatment with dopaminergic agonists. Literature suggests that younger patients tend to have higher Ki-67 indices compared to older patients, indicating a higher proliferative potential and a considerable risk of tumor aggressiveness [28-31]. This underscores the potential benefits of prioritizing surgical intervention as the initial approach.
In our case, the decision for surgical decompression was made immediately due to the tumor size exceeding 2 cm, chiasmatic compression, and invasion of vascular structures, with a KNOPS score of 1 on the left and KNOPS 2 on the right. In the series by Culpin E et al. [13] and the series by Hiroki et al. [24], all patients underwent immediate pituitary surgery to preserve visual function primarily.
Surgical intervention as the first-line treatment [18] seems to be more effective in younger patients due to their higher Ki-67 indices and the difficulties associated with managing more aggressive and invasive tumors, in order to preserve both visual and vital functional prognosis due to vascular compression.
Moreover, surgical treatment often results in a faster normalization of hyperprolactinemia compared to treatment with dopaminergic agonists alone, providing rapid symptomatic relief and effective decompression [32]. In the Hiroki et al. series, normalization of prolactin levels was noted seven days postoperatively [24].
Given the well-established correlation between resistance to dopaminergic agonists and tumor aggressiveness, and the higher Ki-67 index observed in younger patients, as well as the favorable evolution in terms of hormonal profile normalization and visual improvement, we propose that surgical intervention should be preferred over conservative medical treatment as the first-line approach in patients presenting with progressive neurological symptoms, signs of visual pathway compression, and vascular compression, based on the KNOPS score.
However, further case studies or series involving the younger population are needed to establish better recommendations and guidelines for standardizing therapeutic approaches.
Conclusion
Pituitary apoplexy is a rare but critical emergency in children and adolescents, often presenting with variable and non-specific symptoms. MRI is essential for diagnosis, and management requires a multidisciplinary team.
Due to limited pediatric studies, treatment strategies remain unclear. Our experience highlights the potential benefits of early surgical intervention, particularly in cases with significant tumor burden, visual impairment, or vascular compression, to optimize clinical outcomes.
Further studies are needed to establish standardized treatment guidelines for pediatric pituitary apoplexy.
References
- Capatina C, Inder W, Karavitaki N, Wass JA. Prise en charge des maladies endocriniennes : apoplexie tumorale hypophysaire. Eur J Endocrinol, 2015; 172: R179–190. doi: 10.1530/EJE-14-0794.
- Jankowski P, John R Crawford, Paritosh Khanna, Denise M Malicki, Joseph D Ciacci, Mike L Levy. Pituitary tumor apoplexy in adolescents. World Neurosurg, 2015; 83(4): 644-651. doi: 10.1016/j.wneu.2014.12.026.
- Randall BR, Couldwell WT. Apoplexie dans les microadénomes hypophysaires. Neurochir, 2010; 152: 1737-1740.
- alenave S, Ancelle D, Bahougne T. Macroprolactinomas in children and adolescents: factors associated with the response to treatment in 77 patients. J Clin Endocrinol Metab, 2015; 100(3): 1177–1186.
- Özçetin M, Karacı M, Edebali N. Un cas pédiatrique de macroadénome hypophysaire présentant une apoplexie hypophysaire et une atteinte des nerfs crâniens : rapport de cas. Turk Arch Paediatr, 2016; 3(51): 162–165. doi : 10.5152/TurkPediatriArs.2016.1945.
- Glezer A, Bronstein M. Apoplexie hypophysaire: physiopathologie, diagnostic et prise en charge. Arch Endocrinol Metab, 2015; 59(3): 259–264. doi : 10.1590/2359-3997000000047.
- Bailey P. Rapport pathologique d'un cas d'acromégalie, avec référence particulière aux lésions de l'hypophyse cérébrale et de la glande thyroïde ; et un cas d'hémorragie dans l'hypophyse. Phila. Med. J.
- Brougham M, Heusner AP, Adams RD. Modifications dégénératives aiguës dans les adénomes du corps pituitaire – avec une référence particulière à l'apoplexie pituitaire. J. Neurosurg, 1950; 7: 421–439. doi : 10.3171/jns.1950.7.5.0421.
- Picón Jaimes YA, Orozco Chinome JE, López Cepeda D, Quintana Pájaro L, Galindo-Velásquez H, Ramos-Villegas Y, et al. Apoplexie hypophysaire chez les patients pédiatriques : Revue systématique. Rév. Fac. Cien. Médicas Cordoue Argent, 2022; 79: 141-145. doi: 10.31053/1853.0605.v79.n2.27984.
- Enns JP, Al-Khindi T, Wu C, Machaidze M, Sung J. L'apoplexie hypophysaire comme imitateur de la méningite infectieuse chez une patiente adolescente. Ann. Intern. Med. Clin. Cases, 2023; 2: e221328. doi: 10.7326/aimcc.2022.1328.
- Agrawal P, Newbold S, Busaidi AA, Kapoor RR, Thomas N, Aylwin SJ, et al. Apoplexie hypophysaire chez un adolescent atteint d'un macroprolactinome se présentant comme un infarctus du territoire de l'artère cérébrale moyenne. Ann. Pédiatrie. Endocrinol. Métab, 2022; 27: 320–324. doi : 10.6065/apem.2142204.102.
- Kasl RA, Hughes J, Burrows AM, Meyer FB. Accident vasculaire cérébral ischémique pédiatrique dû à un prolactinome apoplectique. Childs Nerv. Syst. ChNS, 2015; 31: 1387–1392. doi : 10.1007/s00381-015-2712-8.
- Culpin E, Crank M, Igra M, Connolly DJA, Dimitri P, Mirza S, et al. Apoplexie tumorale hypophysaire dans les prolactinomes chez les enfants : une pathologie plus agressive ? Hypophyse, 2018; 21: 474–479. doi : 10.1007/s11102-018-0900-8.
- Ohata H, Shinde B, Nakamura H, Teranishi Y, Morisako H, Ohata K, et al. Apoplexie hypophysaire chez un enfant puberté : rapport de cas et revue de la littérature. Interdiscip. Neurochirurgie, 2021; 25: 101160. doi : 10.1016/j.inat.2021.101160.
- Wang R, Wang Z, Song Y, Li L, Han X, Han S. Analyse comparative de l'adénome hypophysaire avec et sans apoplexie chez les patients pédiatriques et adolescents : une série clinique de 80 patients. Neurosurg. Rev, 2022; 45: 491–498. doi : 10.1007/s10143-021-01551-z.
- Ottenhausen M, Conrad J, Wolters LM, Ringel F. La chirurgie comme traitement de première intention du prolactinome ? Discussion de la littérature et résultats d'une série consécutive de patients traités chirurgicalement. Neurosurg. Rev, 2023; 46: 128. doi: 10.1007/s10143-023-02033-0.
- Molitch ME. Diagnostic et traitement des adénomes hypophysaires : une revue. JAMA, 2017; 317: 516–524. doi: 10.1001/jama.2016.19699.
- Yu-Hung Tsai,Chi-Ruei Li, Yu-Ting Wang, Se-Yi Chen. Faisabilité d'un traitement chirurgical précoce pour les patients adolescents atteints de prolactinome: rapport de cas et revue de la littérature, 2024 ;60(8): 1345. doi: 3390/medicina60081345.
- Pyrgelis E-S, Mavridis I, Meliou M. Présentation des symptômes de l'apoplexie hypophysaire. J. Neurol. Surg. Part Cent. Eur. Neurosurg, 2018; 79: 52–59. doi: 10.1055/s-0037-1599051.
- Boellis A, di Napoli A, Romano A, Bozzao A. Apoplexie hypophysaire : mise à jour des caractéristiques cliniques et d'imagerie. Insights Imaging, 2014; 5: 753–762. doi : 10.1007/s13244-014-0362-0.
- Semple PL, Jane JA, Lopes MBS, Laws ER. Apoplexie hypophysaire : corrélation entre l'imagerie par résonance magnétique et les résultats histopathologiques. J. Neurosurg, 2008; 108: 909–915. doi : 10.3171/JNS/2008/108/5/0909.
- Liu ZH, Chang CN, Pai PC, Wei KC, Jung SM, Chen NY, et al. Caractéristiques cliniques et résultats chirurgicaux de l'apoplexie hypophysaire clinique et subclinique. J. Clin. Neurosci, 2010; 17: 694–699. doi : 10.1016/j.jocn.2009.11.012.
- Vicente A, Lecumberri B, Gálvez MÁ. Grupo de Trabajo de Neuroendocrinología Guide de pratique clinique pour le diagnostic et le traitement de l'apoplexie hypophysaire. Endocrinol. Nutr. Organo Soc. Esp. Endocrinol. Nutr, 2013; 60: 582.e1–582.e12. doi: 10.1016/j.endonu.2013.04.013.
- Hiroki Ohata, Bharat Shinde, Honami Nakamura, Yuichi Teranishi, Hiroki Morisako, Kenji Ohata, et al. Pituitary apoplexy in a puberal child: A case report and review of the literature.
- Andereggen L, Tortora A, Schubert GA, Musahl C, Frey J, Luedi MM, et al. Prolactinomes chez les patients adolescents et âgés : une analyse comparative à long terme. Front. Surg, 2023; 10: 967407. doi : 10.3389/fsurg.2023.967407.
- Hinojosa-Amaya JM, Johnson N, González-Torres C, Varlamov EV, Yedinak CG, McCartney S, et al. Outils d'auto-évaluation de la dépression et de l'impulsivité pour identifier les effets secondaires des agonistes dopaminergiques chez les patients atteints d'adénomes hypophysaires. Front. Endocrinol, 2020; 11: 579606. doi : 10.3389/fendo.2020.579606.
- Briet C, Salenave S, Bonneville J-F, Laws ER, Chanson P. Apoplexie pituitaire. Endocr. Rev, 2015; 36: 622–645. doi: 10.1210/er.2015-1042.
- Bălinişteanu B, Cîmpean AM, Ceauşu AR, Corlan AS, Melnic E, Raica M. Une expression élevée de Ki-67 est associée à des adénomes hypophysaires sécrétant de la prolactine. Bosn. J. Basic Med. Sci, 2017; 17: 104–108. doi : 10.17305/bjbms.2017.1750.
- Lu C, Liu Y, Lu Z, Huan C. Ki-67 et corrélations cliniques chez les patients atteints de prolactinomes résistants. Ann. Clin. Lab. Sci, 2020; 50: 199–204.
- Olarescu NC, Perez-Rivas LG, Gatto F, Cuny T, Tichomirowa MA, Tamagno G, et al. Prolactinomes agressifs et malins. Neuroendocrinologie, 2019; 109: 57-69. est ce que je: 10.1159/000497205.
- Tng EL, Teo AE, Aung AT. Macroprolactinome avec résistance secondaire à la DA : rapport de cas et revue de la littérature. J. Med. Case Rep, 2023; 17: 96. doi: 10.1186/s13256-023-03820-5.
- Chen T-Y, Lee C-H, Yang M-Y, Shen C-C, Yang Y-P, Chien Y, et al. Traitement de l'hyperprolactinémie: une expérience d'un seul institut. J. Chin. Med. Assoc, 2021; 84: 1019–1022. doi: 10.1097/JCMA.0000000000000584.

