Decompressive Hemicraniectomy for Stroke Due blunt to traumatic Internal Carotid Artery Dissection
Faraj Kaoutar*, Hmamouche Oualid Mohammed, Hammoud marouane, Lakhdar faycal, Benzagmout mohammed, Chakour khalid and El Faiz Chaoui Mohammed
Department Neurosurgery, Centre hospitalier universitaire HASSAN II, Morocco
Received Date: 11/02/2025; Published Date: 13/03/2025
*Corresponding author: Faraj Kaoutar, Department Neurosurgery, Centre hospitalier universitaire HASSAN II, Morocco
Abstract
Traumatic internal carotid artery dissection (TICAD) is a condition in which the layers of the carotid artery separate, potentially compromising blood flow to certain regions of the brain and leading to a stroke. The most common presentation of TICAD is stroke, with 80% of patients experiencing a stroke within the first week after the trauma. It is the most frequent cause of strokes in younger patients.
TICAD typically occurs following direct cervical trauma or blunt trauma, which can cause acceleration-deceleration forces along with neck hyperextension and rotation, leading to an intimal tear of the carotid artery. Timely diagnosis is crucial to minimize the potential morbidity and mortality associated with this condition.
In this case report, we present a 31-year-old patient who developed TICAD after a motor vehicle crash. He developed ischemic stroke symptoms on the 3rd day of hospitalization in the intensive care unit. The patient underwent decompressive hemicraniectomy and received acetylsalicylic acid, resulting in a full neurological recovery.
This case report aims to highlight the characteristics of a classic stroke secondary to TICAD and to discuss its clinical presentation, diagnostic workup, and treatment.
Keywords: Decompressive Hemicraniectomy; Internal Carotid Artery Dissection; Blunt Trauma; Traumatic Stroke; Carotid Artery Dissection
Introduction
Internal Carotid Artery Dissection (ICAD) can occur spontaneously or as a result of trauma. Traumatic internal carotid artery dissection (TICAD) can affect either the extracranial or intracranial portion of the internal carotid artery. It is a rare condition, most often caused by motor vehicle accidents, amusement park activities, sports injuries, blunt trauma that leads to excessive hyperextension or rotation of the neck, direct blows to the anterolateral side of the neck, or cervical chiropractic manipulation [1-3].
The reported incidence of TICAD has increased with the widespread use of advanced imaging techniques, such as ultrasound, CT angiography, and MRI. While TICAD can be asymptomatic in some cases, most patients eventually develop ischemic stroke. It is one of the leading causes of stroke in young and middle-aged adults [4]. TICAD occurs in 10-20% of such patients, and the onset of symptoms can vary significantly. In some cases, symptoms begin immediately (up to 10% of cases), while in others, they may appear days or months later.
However, only 6% of blunt TICAD cases are diagnosed at the time of initial medical evaluation. For this reason, screening of asymptomatic TICAD patients following traumatic events is recommended. Timely recognition and appropriate treatment are critical to prevent fatal brain infarction [5, 6] and to minimize the potential morbidity and mortality associated with the condition.
Case Report
We report the case of a 32-year-old patient with no significant past medical history, who sustained polytraumatic injuries secondary to a motor vehicle crash and was admitted to the emergency department. Upon arrival, the patient was conscious, and neurological examination was normal (Glasgow Coma Scale of 15), without any disturbance of consciousness or other neurological complications. However, his Airway, Breathing, Circulation, Disability, and Exposure (ABCDE) assessment was disturbed.
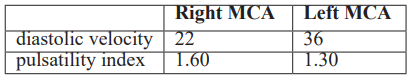
Physical examination revealed a blood pressure of 130/60 mmHg, a respiratory rate of 30 breaths per minute, and oxygen desaturation at 40%. He was intubated and sedated based on respiratory criteria. A trauma CT scan showed normal brain status (Figure 1A), along with alveolar hemorrhage, pneumatocele, minimal pneumothorax, and renal and splenic lacerations. X-ray imaging revealed an acetabular fracture, which was planned for surgical treatment.
The patient was transferred to the intensive care unit (ICU), where he remained intubated and sedated for three days. The decision to stop sedation was made following a follow-up chest imaging, which showed improvement in lung damage. During his ICU stay, his evolution was marked by a delayed awakening. A pathological transcranial Doppler (TCD) revealed a right Pulsatility Index (PI) of 1.60 and a Diastolic Velocity (DV) of 22, and a left PI of 1.30 with a DV of 36 (Table 1). His pupils were in miosis.
A control brain CT scan was performed, revealing a cortico-subcortical hypodense area with subfalcine and temporal herniation (Figure 1B), consistent with an extensive left middle cerebral artery infarction. Additionally, there was cessation of diffusion in the supply area of the right middle cerebral artery (MCA).
Table 1: Transcranial doppler findings.
Further investigation revealed an occluded right internal carotid artery (ICA) (Figure 2A) due to dissection, confirmed by the abrupt cessation of opacification in the extracranial portion of the right ICA, particularly in the cervical region in front of the 3rd and 4th cervical vertebrae ‘Flame-shaped appearance suggestive of dissection (Figure 2B).
The patient underwent osmotherapy and deep sedation with a combination of Midazolam, Fentanyl, and Propofol. Additionally, the patient underwent a right hemicraniectomy to relieve cerebral edema (Figure 1C), along with an enlargement duraplasty. The skull bone flap was preserved by placing it between the right anterior abdominal wall muscles. The patient was also administered acetylsalicylic acid to reduce the risk of progressive thrombosis.
Normalization of the transcranial Doppler was observed, and the patient's neurological condition showed favorable progress. After 10 days, the patient was extubated, regained consciousness with left-sided hemiplegia, and began to properly saturate with ambient air.
He was then transferred to the neurological department for rehabilitation.
The patient made a remarkable neurological recovery and is scheduled to undergo cranioplasty 8 weeks later.
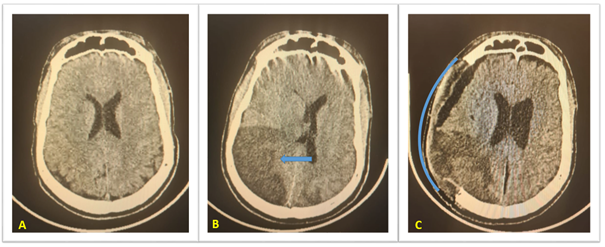
Figure 1: CT Scan findings: A : Normal brain CT scann , B :Right parieto-occipital ischemic area, C:Post-decompressive hemicraniectomy CT scan.
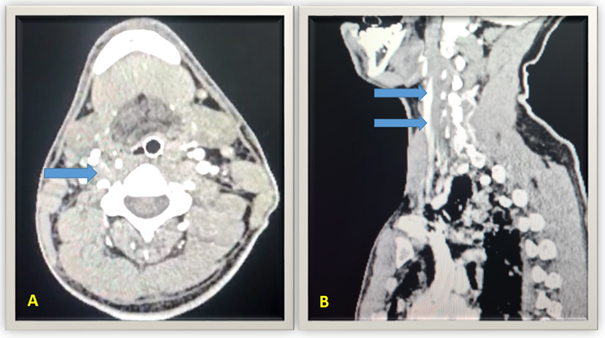
Figure 2: CT Scan findings A: Abrupt cessation of opacification of ICA. B: Flame-shaped appearance of ICA suggestive of dissection dissection (arrow).
Discussion
TICAD often occurs when high-velocity traumatic cerebrovascular injuries are sustained. Rapid and excessive neck movement, which stretches the artery, or a direct impact on the artery, can lead to a sudden defect in the intimal layer of the carotid artery.
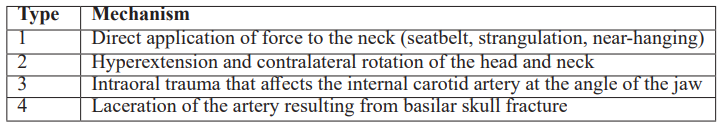
Four characteristic mechanisms of blunt carotidal injury are listed in Table 1 [7].
Table 2: Characteristic mechanisms of blunt carotidal injury.
This defect creates a pathway for blood to flow into the intimal layer of the vessel, resulting in the formation of a hematoma within the blood vessel wall, commonly referred to as a false lumen. Blood entering this false lumen can cause stenosis or occlusion of the carotid artery. Disruption of the elastic lamina may lead to the expansion of the adventitia, potentially resulting in the formation of a traumatic aneurysm [8].
The outcome depends on whether the hematoma develops towards the intima or adventitia. This process can lead to a stroke due to complete vascular occlusion at the site of the dissection. It may also serve as a source for thrombus formation, which can later migrate distally, causing a stroke or transient ischemic attack (Figure 3) [10]. If the vessel ruptures intracranially, it may result in a subarachnoid hemorrhage. Additionally, a pseudoaneurysm can develop as a consequence of a carotid dissection [9].
The cervical internal carotid artery (ICA) is particularly susceptible to stretch injury in the area between the soft tissues of the neck and the petrous canal. The distal cervical ICA is also at risk for stretch injury over the second and third cervical vertebrae during extreme hyperextension, lateral flexion, or rotation. Moreover, hyperflexion and significant rotation can put the ICA in danger of compression by the angle of the mandible and styloid process. In our case, the portion of the ICA that was stretched is located in front of the 3rd and 4th cervical vertebrae.
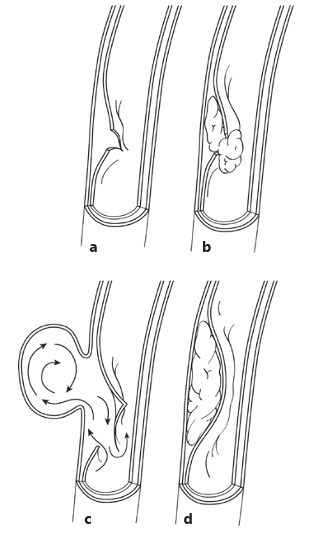
Figure 3: Traumatic cerebrovascular injuries.
a Intimal disruption. b Intimal disruption with thrombus formation. c Elastic laminae disruption allowing traumatic aneurysm formation (arrows). d Hematoma within the artery wall with luminal stenosis.
The clinical manifestations of TICAD are variable and depend on the location of the affected artery, the site and grade of the injury, as well as the underlying clinical condition of the patient. Patients with TICAD may present with a range of symptoms, from mild signs such as headache, cranial nerve palsy, or neck pain, to more severe symptoms, such as stroke [11]. The incidence of stroke following TICAD can range from 60% to 80%, depending on the population studied [12]. The onset of ischemic symptoms can vary significantly [13]. Typically, a latent period exists between the time of injury and the onset of symptoms, which can make diagnosis more challenging [14]
The average time for stroke to develop is typically between 12 to 75 hours post-trauma [3]. In our case, the asymptomatic period lasted 5 days. One of the primary goals in managing this condition is to establish an accurate diagnosis before a stroke occurs [15]. In cases of severe trauma, screening for TICAD is often recommended, as, although rare, TICAD carries high morbidity and mortality rates (up to 43%). In our case, no clinical signs were initially present, and the initial CT scan was normal. However, the patient presented 5 days later with consciousness disturbances and pathological findings on transcranial Doppler ultrasound.
The diagnosis of TICAD primarily relies on neuroimaging findings. When TICAD occurs, imaging studies are used to assess the cerebral parenchyma and the corresponding supply artery. The cerebral parenchyma can be easily visualized using CT or MRI. TICAD can also be detected through conventional angiography and magnetic resonance angiography [14,17].
The TICAD can be divided into five subtypes: 1. Luminal irregularity or dissection with <25% stenosis; 2. Dissection or intramural haematoma with ≥25% stenosis; 3. Traumatic aneurysm; 4. Occlusion; 5. Transection (Table 2) [10].
Table 2: Blunt carotid arterial injury classification by digital angiography.

Due to the low incidence of TICAD, there are no evidence-based guidelines available for its management. The treatment for TICAD remains a subject of debate. Since cerebral infarction can occur several hours after traumatic injury, it is crucial to treat TICAD promptly. When suspected, the foundation of treatment is antithrombotic therapy, including antiplatelet agents such as acetylsalicylic acid (AAS) and anticoagulants.
Endovascular therapy, such as mechanical thrombectomy or stenting, may be considered in selected cases [10].
As recently described, stenting of the carotid arteries through an endovascular approach may provide immediate revascularization, improve perfusion, and limit embolus formation in patients presenting with embolic or hemodynamic symptoms [18]. However, if the definitive diagnosis is made too late, vascular recanalization may no longer be an option for treatment.
The present case was classified as subtype 4; however, the definitive diagnosis was made 4 days after the trauma, making it too late for treatment with vascular recanalization.
As the patient exhibited deteriorating levels of consciousness, a decompressive craniectomy was performed to alleviate the refractory high intracranial pressure, the patient received antiplatelet drugs and made a remarkable neurological recovery, followed by cranioplasty 8 weeks later.
The prognosis of patients with TICAD mainly depends on the degree of stenosis and thrombosis of the dissected artery. Therefore, we hypothesize that in some cases, the clinical presentation and prognosis of TICAD may be influenced by the extent of collateral circulation opening [19].
Conclusion
TICAD is a rare but potentially life-threatening condition, referring to arterial dissection caused by an intimal tear in the internal carotid artery (ICA) after trauma. Thromboembolism and hypoperfusion are the main pathological factors. Although TICAD is present in only 1–2% of all blunt trauma admissions, it is becoming increasingly recognized as an important cause of ischemic stroke.
Once considered a rare occurrence, TICAD is now being diagnosed more frequently in recent years, partly due to the implementation of new screening protocols such as angio-CT.
In most cases, there is a variable latent period between the injury and the onset of symptomatic stroke. Early and efficient diagnosis of TICAD is crucial for initiating appropriate treatment.
References
- Bouzat P, Francony G, Brun J, Lavagne P, Picard J, Broux C, et al. Detecting traumatic internal carotid artery dissection using transcranial Doppler in head-injured patients. Intensive Care Med, 2010; 36: 1514–1520. doi: 10.1007/s00134-010-1919-0.
- Tveita IA, Madsen MRS, Nielsen EW. Dissection of the internal carotid artery and stroke after mandibular fractures: a case report and review of the literature. J Med Case Rep, 2017; 11: 148. doi: 10.1186/s13256-017-1316-1.
- Kowalski RG, Haarbauer-Krupa JK, Bell JM, Corrigan JD, Hammond FM, Torbey MT, et al. Acute Ischemic Stroke After Moderate to Severe Traumatic Brain Injury: Incidence and Impact on Outcome. Stroke, 2017; 48: 1802–1809. doi: 10.1161/STROKEAHA.117.017327.
- Debette S, Mazighi M, Bijlenga P, et al. ESO guideline for the management of extracranial and intracranial artery dissection. Eur Stroke J, 2021; 6: XXXIX–LXXXVIII.
- Löhrer L, Vieth V, Nassenstein I, Hartensuer R, Niederstadt T, Raschke MJ, et al. Blunt cerebrovascular injuries in acute trauma care: a screening protocol. Eur Spine J, 2012; 21: 837–843. doi: 10.1007/s00586-011-2009-x.
- Furtner M, Werner P, Felber S, Schmidauer C. Bilateral carotid artery dissection caused by springboard diving. Clin J Sport Med, 2006; 16: 76–78. doi: 10.1097/01.jsm.0000173267.84112.a0.
- Crissey MM, Bernstein EF, Calcaterra TC, Holt GP, DeWeese JA, Rob CG, et al. Delayed presentation of carotid intimal tear following blunt craniocervical trauma. Surgery, 1974; 75: 543–549.
- Goodfriend SD, Tadi P, Koury R. Carotid Artery Dissection. In: StatPearls, Treasure Island (FL): StatPearls Publishing, 2025.
- Griessenauer CJ, Foreman PM, Deveikis JP, Harrigan MR. Optical coherence tomography of traumatic aneurysms of the internal carotid artery: report of 2 cases. J Neurosurg, 2016; 124: 305–309. doi: 10.3171/2015.1.JNS142840.
- Foreman PM, Harrigan MR. Blunt Traumatic Extracranial Cerebrovascular Injury and Ischemic Stroke. Cerebrovasc Dis Extra, 2017; 7(1): 72-83. doi: 10.1159/000455391.
- Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol 2014; 13: 844-854. DOI: 10.1016/S1474-4422(14)70120-6.
- Galyfos G, Filis K, Sigala F, Sianou A. Traumatic Carotid Artery Dissection: A Different Entity without Specific Guidelines. Vasc Spec Int, 2016; 32(1): 1–5. Doi: 10.5758/vsi.2016.32.1.1.
- Makhlouf F, Scolan V, Detante O, Barret L, Paysant F. Post-traumatic dissection of the internal carotid artery associated with ipsilateral facial nerve paralysis: diagnostic and forensic issues. J Forensic Leg Med, 2013; 20(07): 867–869.
- Wang GM, Xue H, Guo ZJ, Yu JL. Cerebral infarct secondary to traumatic internal carotid artery dissection. World J Clin Cases, 2020; 8(20): 4773-4784. doi: 10.12998/wjcc.v8.i20.4773.
- Cohen JE, Gomori JM, Itshayek E, Spektor S, Shoshan Y, Rosenthal G, et al. Single-center experience on endovascular reconstruction of traumatic internal carotid artery dissections. J Trauma Acute Care Surg, 2012; 72: 216–221.
- Ben Hassen W, Machet A, Edjlali-Goujon M, Legrand L, Ladoux A, Mellerio C, et al. Imaging of cervical artery dissection. Diagn Interv Imaging, 2014; 95: 1151–1161.
- Crönlein M, Sandmann GH, Beirer M, Wunderlich S, Biberthaler P, Huber-Wagner S. Traumatic bilateral carotid artery dissection following severe blunt trauma: a case report on the difficulties in diagnosis and therapy of an often-overlooked life-threatening injury. Eur J Med Res, 2015; 20: 62.
- Daou B, Hammer C, Mouchtouris N, Starke RM, Koduri S, Yang S, et al. Anticoagulation vs Antiplatelet Treatment in Patients with Carotid and Vertebral Artery Dissection: A Study of 370 Patients and Literature Review. Neurosurgery, 2017; 80: 368–379.
- Bajkó Z, Maier S, Moţăţăianu A, Bălaşa R, Vasiu S, Stoian A, et al. Stroke Secondary to Traumatic Carotid Artery Injury - A Case Report. J Crit Care Med (Targu Mures), 2018; 4(1): 23-28. doi: 10.1515/jccm-2018-0003.

