Diagnostic Pitfalls and Management of a Rare Cervical Lipoblastoma in a Pediatric Patient
Hamza Bensaghir*, Chaimae Ben Driss, Oussama Mai, Ali Lahrech and Nawfal Fejjal
Plastic Surgery Unit, Department of Surgery C, Children's Hospital of Rabat, Morocco
Faculty of Medicine and Pharmacy of Rabat, University Mohammed V, Rabat, Morocco
Received Date: 29/01/2025; Published Date: 04/03/2025
*Corresponding author: Hamza Bensaghir, Plastic Surgery Unit, Department of Surgery C, Children's Hospital of Rabat, Morocco; Faculty of Medicine and Pharmacy of Rabat, University Mohammed V, Rabat, Morocco
Abstract
Background: Lipoblastoma is a rare benign mesenchymal tumor derived from embryonic fat, primarily affecting children under three years old. Although typically occurring in the extremities, posterior cervical lipoblastomas are exceptionally uncommon and pose significant diagnostic and management challenges due to their proximity to vital structures.
Case Presentation: We report a case of a 3-year-old girl with a posterior cervical lipoblastoma initially misdiagnosed as a cystic lymphangioma on MRI. The definitive diagnosis was established postoperatively through histopathological analysis. The mass was completely excised without complications, and the patient had an uneventful recovery.
Conclusion: This case highlights the importance of considering lipoblastoma in the differential diagnosis of pediatric cervical masses and underscores the role of histopathological confirmation in achieving an accurate diagnosis. Complete surgical excision remains the cornerstone of treatment, ensuring a favorable long-term prognosis.
Keywords: Lipoblastoma; Cervical tumor; Pediatric surgery; Diagnosis; Case report
Introduction
Lipoblastoma is a rare, benign tumor originating from embryonic fat cells, most commonly diagnosed in infants and young children. Accounting for less than 1% of pediatric soft tissue tumors, it typically arises in the extremities, trunk, and retroperitoneum. Posterior cervical localization remains exceedingly rare, with only a few cases reported in the literature [1-3].
Clinically, posterior cervical lipoblastomas may present as a painless, slow-growing mass but can become symptomatic if they compress nearby structures, leading to restricted neck movement, spinal cord compression symptoms, or cosmetic concerns [4]. Given the overlapping features with malignant liposarcomas and other soft tissue tumors, precise diagnosis relies on imaging and histopathological examination [5].
This case report describes an atypical instance of posterior cervical lipoblastoma, which was initially misdiagnosed as a cystic lymphangioma on MRI. The discussion aims to contribute to the limited literature on this topic and emphasize the challenges of preoperative diagnosis in pediatric cervical masses.
Case Presentation
A 3-year-old girl with no notable medical history presented with a progressively enlarging posterior cervical mass on the left side, first noticed by her mother due to mild discomfort. There were no signs of vascular or neurological compression. On physical examination, the mass was painless, non-indurated, mobile in relation to the deep plane, and measured approximately 5 cm. No inflammatory signs were noted.
Imaging and Diagnosis
- Ultrasound: Initially described an inhomogeneous tissue mass with oval contours, difficult to assess with an avascular probe, suggesting a subcutaneous lesion measuring 40 mm × 20 mm.
- MRI (Figure 1): A well-defined, oval-shaped mass measuring 42 mm × 30 mm with a 37 mm extension under the left occipital region, insinuating between the levator scapulae and trapezius muscles. It showed T2 hypersignal, T1 hyposignal, no diffusion restriction, and thick septa enhancing after gadolinium injection. The radiological conclusion favored a macrocystic lymphatic malformation suggestive of a cystic lymphangioma.
Surgical Management
The patient was taken to the operating room under general anesthesia in the prone position (Figure 2). A transverse incision was made over the posterior cervical region, and careful dissection was performed to avoid injury to the surrounding neurovascular structures (Figure 3). The mass was resected completely and sent for histopathological examination (Figure 4).
Histopathological Findings
Contrary to the radiological diagnosis, histopathological examination confirmed the presence of immature adipocytes with no signs of malignancy, leading to a definitive diagnosis of lipoblastoma.
Follow-Up
The patient had an uneventful postoperative recovery (Figure 5). Follow-up evaluations showed no recurrence, and the child remained asymptomatic.
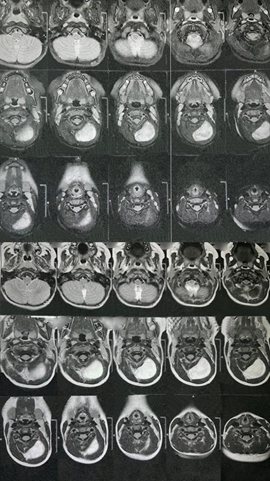
Figure 1: MRI image showing the lesion that was determined to be cystic lymphangioma.
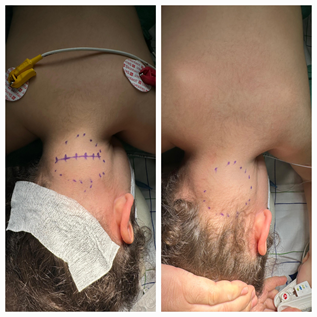
Figure 2: Image showing preoperative mass identification.
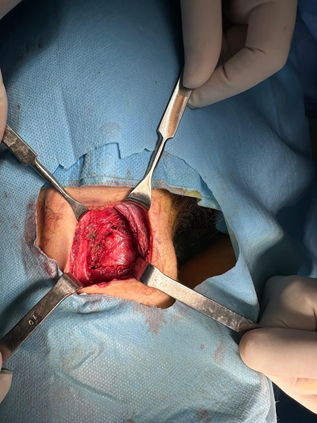
Figure 3: Image showing the mass intraoperatively.

Figure 4: Image showing the mass after its resection and before its sending to anatomopathology.

Figure 5: Image showing the post-operative appearance of the patient.
Discussion
Epidemiology and Pathogenesis
Lipoblastomas arise from immature adipocytes and are classified into two forms: well-circumscribed lipoblastomas and diffuse lipoblastomatosis [5]. They are predominantly seen in children under three years old and exhibit rapid growth due to their embryonic origin. Posterior cervical involvement is rare, accounting for less than 10% of cases, making early recognition crucial [6].
Diagnostic Challenges
This case highlights the diagnostic challenges associated with posterior cervical lipoblastomas, particularly their potential for misdiagnosis. The MRI findings of a T2-hyperintense, well-encapsulated lesion with septations closely resembled those of cystic lymphangioma. Such misinterpretations can delay appropriate surgical planning and patient management [7].
The differential diagnosis for a posterior cervical mass in a young child includes:
- Cystic lymphangioma: Characterized by a multilocular cystic structure with septal enhancement [8].
- Neurogenic tumors: Typically exhibit a more heterogeneous signal with nerve root involvement [9].
- Rhabdomyosarcoma: Shows diffusion restriction and contrast enhancement, suggesting a malignant nature [10].
This case emphasizes the necessity of histopathological confirmation, as imaging alone may not always provide a definitive diagnosis [11].
Surgical Considerations and Outcomes
Complete surgical excision remains the treatment of choice, given the tumor's propensity for local recurrence if incompletely resected. The delicate posterior cervical anatomy presents significant operative challenges, particularly in preserving vital structures such as the spinal cord, vertebral arteries, and deep cervical muscles. In our case, meticulous dissection allowed for total excision without complications, aligning with best practices reported in recent studies.
Prognosis and Follow-Up
Lipoblastomas are benign but have a recurrence rate of up to 25%, primarily linked to incomplete excision. Regular follow-up with imaging is recommended, particularly in cases where complete excision is uncertain. Malignant transformation is extremely rare but should be considered in recurrent or atypical cases [12].
Comparison with Literature
Our findings align with previously reported cases, reinforcing the importance of MRI in preoperative planning while also highlighting its limitations in distinguishing lipoblastomas from other cystic lesions. Given the rarity of posterior cervical lipoblastomas, this case contributes to the growing body of literature advocating for early surgical intervention to prevent spinal cord compression and local invasion [13].
Conclusion
Posterior cervical lipoblastoma is an uncommon pediatric tumor that necessitates early diagnosis and surgical intervention to prevent complications. This case underscores the importance of histopathological confirmation, as radiological findings can sometimes lead to misdiagnosis. Complete surgical excision remains the cornerstone of treatment, ensuring a favourable long-term prognosis. Further case studies and multicenter reviews are needed to refine diagnostic approaches and optimize management strategies.
Declarations
Ethical Approval: Not required for de-identified case reports based on institutional policies.
Consent: Written informed consent was obtained from the patient's legally authorized representatives.
Competing Interests: The authors declare no competing interests.
Funding: None.
References
- Coffin CM, Dehner LP. Lipoblastoma: A clinicopathologic study of 59 cases. Am J Surg Pathol,
- Enzinger FM, Weiss SW. Benign lipoblastic tumors in infancy. J Pediatr Surg,
- Chung EB, Enzinger FM. Lipoblastoma and lipoblastomatosis in children. Cancer,
- Capraro PA, Dickson JH. Lipoblastoma of the neck in a 2-year-old child. Pediatrics,
- Dilley AV, et al. Soft tissue tumors in children. J Pediatr Surg,
- Murphey MD, et al. Imaging of pediatric soft tissue tumors. Radiographics,
- Coffin CM, Alaggio R. Mesenchymal tumors in children. Am J Clin Pathol,
- Requena L, et al. Adipocytic tumors. Pathology,
- Montgomery E, et al. Pediatric adipocytic tumors. Arch Pathol Lab Med,
- Weiss SW, Goldblum JR. Benign fatty tumors. Enzinger & Weiss's Soft Tissue Tumors,
- Navarro OM, et al. Pediatric soft tissue tumors and pseudotumors. Radiographics,
- Montgomery EA, et al. Recurrence rates in lipoblastomas. Mod Pathol,
- Al-Ibraheemi A, et al. A review of pediatric fatty tumors. Pediatr Dev Pathol,

