Ischaemic Monomelic Neuropathy and Compartment Syndrome: A Spectrum of Ischaemia
Tom Challoner*, Mei Sien Liew and Rajive Jose
Registrar, Plastic Surgery, Queen Elizabeth Hospital, UK
Received Date: 12/12/2024; Published Date: 30/01/2025
*Corresponding author: Tom Challoner, Registrar, Plastic Surgery, Queen Elizabeth Hospital, Mindelsohn Way, Birmingham, B15 2GW, UK
Abstract
Ischaemic Monomelic Neuropathy (IMN) is a rare sequelae of arteriovenous fistula formation in the upper limb. It typically presents with sensory disturbance and represented ischaemic to peripheral nerves. A case of ischaemia following fistula revision is presented and ongoing ischaemic leading to acute compartment syndrome. The pathophysiology of IMN is unclear, however the ischaemic insult to the nerves must also affect the other structures in the forearm, including muscles, and should be recognised as spectrum of ischaemia. Progression to compartment syndrome is a significant risk with devastating consequences and should therefore be considered in any neurovascular disturbance following fistula formation.
Keywords: Compartment Syndromes; Vascular fistula; Ischemia
Introduction
Ischaemic Monomelic Neuropathy (IMN) is a rare peripheral neuropathy complication secondary to an ischaemic injury following the creation of arteriovenous (AV) fistulae of the upper limb providing access for haemodialysis. The estimated incidence rate of IMN is 0.5% following vascular access procedure, but the exact pathophysiology of IMN is poorly understood [1]. Still, it is caused by an arterial steal, and poor perfusion of vasa nervorum, resulting in multiple axonal loss mononeuropathies in the distal limb [2]. The symptoms commonly occur immediately postoperatively with predominantly neurological signs, but often without notable clinical ischaemia affecting the limb. IMN can lead to permanent functional loss of the affected limb and irreversible chronic pain. Whilst recognised amongst transplant surgeons, a spectrum of ischaemic insults can occur with all forearm structures at risk. We present a case of acute compartment syndrome associated with the revision of the brachiocephalic fistula for haemodialysis access which the diagnosis was delayed.
Case Presentation
A 35-year-old, right-handed male underwent revision of a brachiocephalic fistula for haemodialysis. He had previously undergone a live donor kidney transplant which had failed, and the flow in his existing right-sided fistula had reduced, requiring revision. Under general and regional supraclavicular block anaesthesia, a 6mm GORE® ACUSEAL Vascular Graft (Gore Medical, Arizona, USA) was anastomosed proximal to the previous cephalic vein anastomosis in the upper arm with an end-to-side anastomosis. It was tunnelled distally and anastomosed to the cephalic vein. The hand was perfused following the procedure, and radial artery flow confirmed with handheld doppler.
The patient was reviewed 4 hours postoperatively due to significant pain in the forearm which had been present since the procedure. The right forearm was warm, but the hand slightly cooler, with a digital capillary refill time of 3 seconds. Further analgesia was prescribed.
The patient was reviewed overnight with the same complaint of significant pain which was improved at rest. There was sensory disturbance to the entire hand in all territories distal to the wrist, and weakness of both the intrinsics and long flexors and extensors to the digits. The capillary refill time was <2 seconds and the hand warm, however the radial pulse could not be palpated. There was no collection at the surgical site. A fentanyl PCA was commenced, with a diagnosis of IMN considered and the sensory disturbance was considered a consequence of the regional block wearing off.
The following morning, approximately 18 hours postoperatively, due to persistent sensory disturbance, pain, and a contracture of the digits, the patient was returned to theatre for exploration. It was identified that there was no flow in the radial and ulnar arteries whilst the graft was patent. When clamped, normal flow was restored, demonstrating a significant vascular steal. The graft was tied off and wounds were closed.
The patient was referred to the upper limb service following this secondary procedure as his symptoms had not improved. On examination, the right hand was held in a clawed position, with pain on passive extension of the digits, a tense volar compartment of the forearm, and paraesthesia to the entire hand distal to the wrist crease, suggestive of median, ulnar, and superficial branch of radial nerve palsy involvement. Creatinine kinase was 5894 (Figure 1). A clinical diagnosis of compartment syndrome was made, and the patient planned for return theatre for right forearm fasciotomy.
This was delayed primarily due to emergency and trauma case burden, but also a potassium level of 6.5mmol/L, necessitating urgent dialysis due to the risk of intraoperative reperfusion injury upon muscle decompression and causing cardiac complications.
The patient underwent volar compartment fasciotomy and carpal tunnel decompression approximately 25 hours following the original procedure and therefore onset of ischaemia. Flexor digitorum profundus and superficialis were extensively necrosed, with sparing of flexor carpi ulnaris, Flexor Carpi Radialis (FCR), and the median nerve. The patient returned to theatre 48 hours later for further debridement and it was noted FCR was necrosed. The patient has further two operations following the relook of right forearm fasciotomy wound and all wounds were closed primarily.
Four months following the final surgical procedure, the patient has been commenced on pregabalin and tramadol under the care of the chronic pain service. He maintains excellent range of motion in the small joints of the hand due to engagement in hand therapy. There is no sensation in either the median or ulnar nerve territories of the hand. He has been planned for an extensor indicis proprius opponensplasty, and extensor carpi radialis longus to flexor digitorum profundus. Nerve conduction studies are planned to assess function of the median and ulnar nerves and if appropriate, neurolysis will be performed. Haemodialysis was continued using an internal jugular vein tunnelled line, with fistula formation to the contralateral limb under consideration.
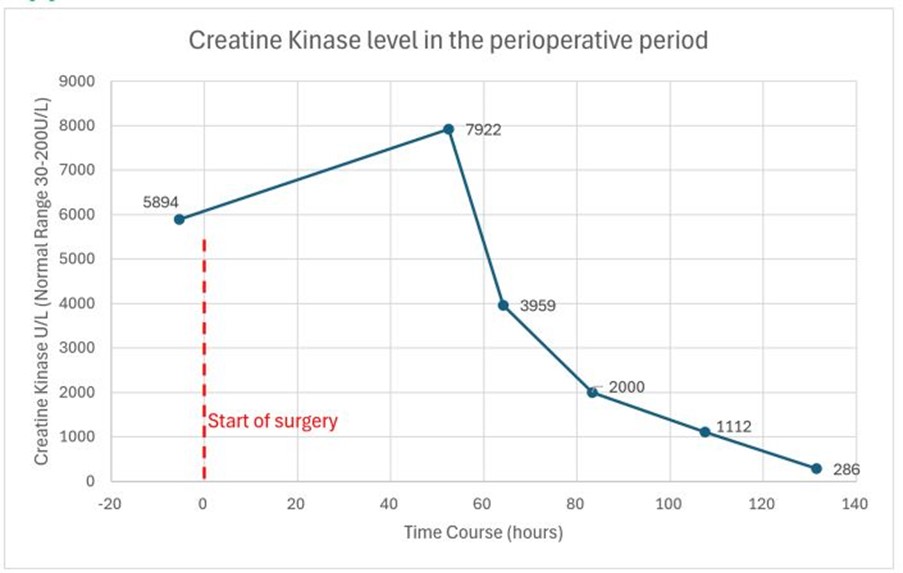
Figure 1: Creatine Kinase level in the perioperative period.
Discussion
Ischaemic monomelic neuropathy is a rare complication of AV fistula formation with an estimated incidence of 0.5% following vascular access procedures [1]. The exact incidence of IMN is unknown as it is under-recognised and often misdiagnosed [3]. Brachiocephalic fistulae are most at risk as the brachial artery serves as the sole arterial supply to the distal upper limb. First described in 1983 [4], the shunting of arterial blood supply away from the distal limb causes ischaemia to multiple peripheral nerves in a limb, and presented with global sensory disturbance to the limb in all neurological territories, diffuse motor weakness, and pain. The hand may be warm, with palpable radial and ulnar pulses or present using a pencil doppler probe. Symptoms tend to be worse distally to the limb, less severe proximally and present immediately after fistula formation.
Shunting blood away from the neurological structures must also affect other structures within the forearms such as musculature. Whilst originally hypothesised that there is indeed sufficient inflow to adequately perfuse muscles, it is recognised that muscles are less resistant to ischaemic damage, with irreversible damage caused within 4-6 hours. Early reversal of the fistula may increase the probability of an improvement in neurological symptoms, however any ischaemic injury to muscle or reperfusion of ischaemic muscle can cause oedema and swelling within the tight fascial compartment and result in an acute compartment syndrome.
The diagnosis of acute compartment syndrome is clinical, with patients complaining of severe pain, out of proportion to any injury or incision performed. Pain is often aggravated by passive stretch of the muscles and may be associated with paraesthesia. The compartment feels tense and tender on palpation. Signs of poor perfusion are late and should not be relied upon for diagnosis. Acute compartment syndrome requires urgent open fasciotomy by incising both skin and fascia to reduce the compartment pressure, restore blood flow, and minimise damage to muscle and nerve. Debridement of necrotic muscle may be necessary to maximise the preservation of function and prevent infection.
Regional anaesthesia has grown in popularity as it provides reliable anaesthesia for limb surgery, and excellent postoperative analgesia. It can however mask any postoperative concerns such as ischaemic pain, or haematoma which would require urgent surgical intervention, and such patients should be monitored closely if any concern is raised.
The case described demonstrates not only neurological ischaemia, but a global ischaemic insult to the forearm. The more proximal graft placement increased the risk of a vascular steal, and the calibre of the graft diverted blood away from the normal arterial tree, and therefore all structures supplied by the distal brachial artery, radial and ulnar arteries.
Whilst the hand appeared pink and perfused postoperatively, the follow-up procedural findings demonstrated that inflow to the hand was inadequate, and reversible ischaemic damage to the muscles had occurred. The resulting deficit and functional loss following such significant muscle necrosis are devastating, therefore compartment syndrome should always be considered in patients with significant postoperative pain and sensory disturbance following fistula formation. This ischaemia should be considered on a spectrum, and whilst IMN may be a relatively minor side effect, prolonged and more significant vascular diversion risks a more serious insult.
Conclusion
Compartment syndrome and limb ischaemic should be considered in any altered neurological state following fistula formation. When reversing fistulae for suspected IMN, we would advocate an exploratory incision to inspect the muscles with a low threshold for full compartmental fasciotomy especially if a delay in diagnosis has occurred. Close postoperative monitoring should be performed in those undergoing limb procedures under regional anaesthesia as these can mask clinical signs.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author/s declare/s no conflict of interest.
References
- Watson LJ, Hansrani M. A Systematic Review of 88 Reported Cases of Ischaemic Monomelic Neuropathy Following Vascular Access Procedures. European Vasc Endovascular Surg, 2019; 58: 330-331. 1016/j.ejvs.2019.06.947.
- Thimmisetty RK, Pedavally S, Rossi NF, Fernandes JAM, Fixley J. Ischemic Monomelic Neuropathy: Diagnosis, Pathophysiology, and Management. Kidney Int Rep, 2016; 27: 76-79. 1016/j.ekir.2016.08.013.
- Hye RJ, Wolf YG. Ischemic monomelic neuropathy: an under-recognized complication of hemodialysis access. Ann Vasc Surg, 1994; 8: 578-582. 1007/BF02017415.
- Wilbourn AJ, Furlan AJ, Hulley W, Ruschhaupt W. Ischemic monomelic neuropathy. Neurology, 1983; 4: 6300732. 1212/wnl.33.4.447.

