Pleomorphic Adenoma of the Lacrimal Gland Revealed by Exophthalmos
Ayoub Bakhil*, Buckat Hugues, Adam Benbachir, Amina Kahoul, Hicham Sabani, Lahcen Khalif, Jalal Hamama and Karim El Khatib
Department of Plastic and Maxillofacial Surgery, Mohammed V Military Hospital, Mohammed V University, Rabat, Morocco
Received Date: 09/12/2024; Published Date: 22/01/2025
*Corresponding author: Ayoub Bakhil, Department of Plastic and Maxillofacial Surgery,. Mohammed V Military Hospital, Mohammed V University, Rabat, Morocco
Abstract
Tumors of the lacrimal gland are dominated by benign tumors, of which pleomorphic adenoma is the most frequent. We report the case of a patient admitted for exophthalmos with diplopia and decreased visual acuity, whose radiological exploration showed an encapsulated tumor of the right lacrimal gland. When a pleomorphic adenoma is suspected, cytopuncture and biopsy are contraindicated, given the risk of recurrence, and surgical excision without capsular invasion is ideal. If left untreated, in addition to the risk of eyeball compression, malignant transformation is possible.
Keywords: Pleomorphic adenoma; Exophthalmos; Orbitotomy
Introduction
The orbit of the eye is a bony cavity in the viscerocranium, which contains a large number of delicate anatomical structures that play an essential role in the normal functioning of vision and can give rise to a variety of neoplasms. The lacrimal gland occupies the upper-external part of this cavity and is made up of glandular parenchyma that excretes tears which protect the cornea.
Tumours of the lacrimal gland account for around 6% of orbital tumours, causing non-axial exophthalmos and affecting vision, which can lead to blindness if left untreated due to compression of the structures of the eyeball. Tumour proliferation may be epithelial or non-epithelial.
Pleomorphic adenoma is a frequent tumour of the salivary glands, particularly the parotid gland, and its intra-orbital lacrimal location is rarer.
In this article we report the case of a patient admitted for exophthalmos with visual acuity impairment revealing a pleomorphic adenoma of the lacrimal gland.
Case Report
Patient aged 40, with no notable pathological history, admitted for management of right exophthalmos. The history of the disease dates back 3 years to the patient's observation of an asymmetry of the two eyeballs with a protrusion on the right side. The evolution was marked by a rapid accentuation of the exophthalmos in the last 6 months with a drop in visual acuity, which prompted the patient to consult a doctor.
On admission, the patient was conscious and haemodynamically and respiratorily stable. The ophthalmological examination revealed a drop in visual acuity to 6/10ths in the right eye, with normal eye tone and a strictly normal examination of the left eye.
On the right side, there is a non-reducible, painless, non-axial exophthalmos with downward and inward deviation of the eyeball (Figure 1) and binocular diplopia. There were no inflammatory signs or lagophthalmos.
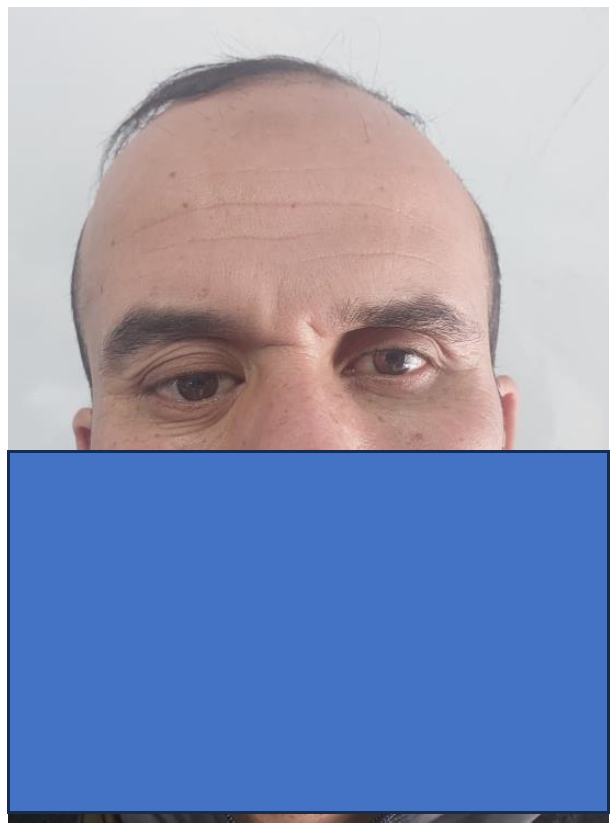
Figure 1: Non-axial right exophtalmous.
Oculomotor examination showed limited abduction of the right eye, and the fundus was unremarkable.
In view of this clinical picture, a radiological work-up was requested, consisting of an orbito-cerebral MRI, which showed the presence of a tissue process of the lacrimal gland located at the level of the superior-external angle of the right orbit, with lysis of the cortex of the orbital roof and compression of the right external oculomotor muscle, with no signs of intracerebral extension (Figure 2).
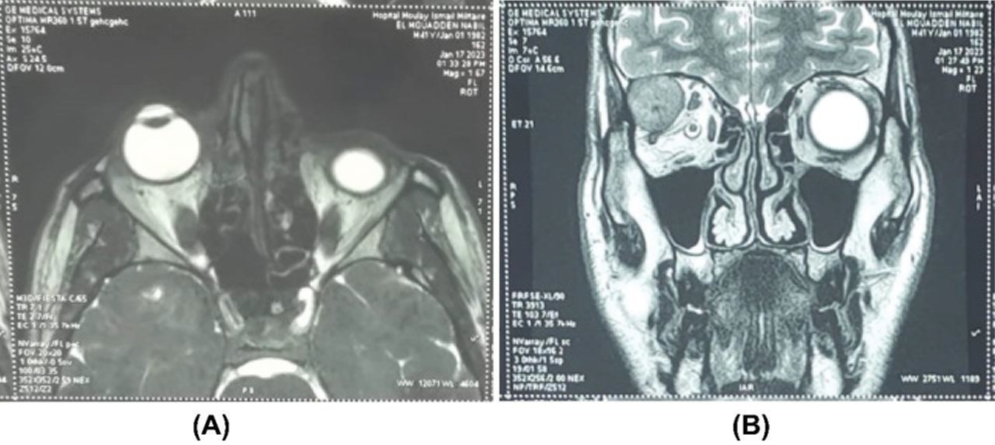
Figure 2: MRI in axial section A and coronal section B. Lesion process in the superior external angle of the right orbit, with a slightly heterogeneous signal, hyperintense in T2 and moderately heterogeneously enhanced.
In view of the functional and morphological repercussions, the patient was admitted for removal of the tumour under general anaesthetic, with the incision concealed in the upper palpebral crease and extended into a fold of the crow's feet outside the external canthus.
A lateral orbitotomy with removal of the lateral wall by two osteotomies, subperiosteal detachment and discovery of the tumour. Dissection of the tumour was delicate so as not to touch the eyeball, and a monobloc excision was performed (Figure 3).

Figure 3: Lateral orbitotomy and tumour removal.
The post-operative course was marked by a reduction in exophthalmos and the absence of complications (Figure 4).
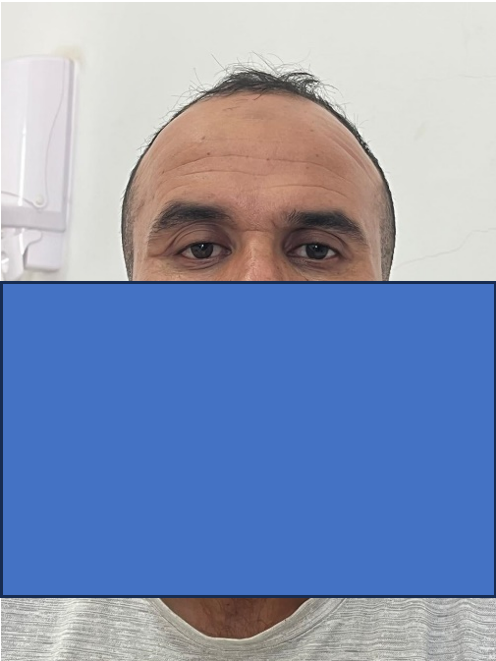
Figure 4: appearance at 6 months.
Anatomopathological examination of the surgical specimen revealed a nodular proliferation limited by fibrous reinforcement, consisting of two components, the first epithelial with an arrangement in cords, tubes and small patches made up of medium-sized ovoid cells with acidophilic cytoplasm and regular round nuclei, without cytonuclear abnormalities, with the presence in some places of foci of squamous metaplasia sometimes with corneal maturation. The second component is a loose connective tissue made up of fibroblasts in myxoid patches, sometimes associated with areas of cartilage metaplasia. In conclusion, the morphological appearance is compatible with a completely excised pleomorphic adenoma.
Discussion
Pleomorphic adenoma is the most common benign tumour of the lacrimal gland, accounting for 40% of epithelial tumours. Formerly known as a benign mixed tumour, it accounts for 3 to 5% of tumours of the orbit and occurs most often in patients between the ages of 20 and 50 [1,2]. It is a tumour that mainly affects the main salivary glands, in particular the parotid gland in 80% of cases, and rarely affects the lacrimal gland.
The clinical signs are non-specific, forming an orbital syndrome. The first reason for consultation is usually non-axial exophthalmos, which progresses slowly or is unsightly, and sometimes oculomotor problems with diplopia. Exophthalmos is evidence of an expansive process inside the orbit which pushes the eyeball forward of the orbital bone frame [2].
For tumours of the lacrimal gland, MRI remains the examination of choice in T1 and T2 sequences, but if MRI is not available or if there is a contraindication, a CT scan with injection of contrast product can be carried out with analysis of the bone and parenchymal windows. On imaging, the pleomorphic adenoma will appear well limited, spontaneously hyperdense and moderately contrast-enhancing. It will enlarge the lacrimal fossa without there ever being any osteolysis or intratumoral calcification. Diagnosis of a malignant tumour is difficult, even on MRI [3].
Pleomorphic adenomas are treated surgically, with en bloc removal of the tumour, respecting the capsule. Any biopsy is formally contraindicated because of the risk of orbital dissemination and recurrence. Capsular invasion is thought to increase the number of recurrences from 3% to 32% [4].
Access to the lacrimal gland requires a lateral oribtotomy, which can be performed with or without bone removal. The skin incision is an elongated S-type Wright incision or an incision in the upper palpebral crease extended at the level of the lateral canthus. When bone removal is performed, it is a Krönlein procedure, removing the lateral pillar of the orbit and then reattaching it at the end of the procedure [5].
In the absence of treatment, in addition to the risk of compression of the eyeball and worsening of exophthalmos, there is a risk of carcinomatous degeneration into a pleomorphic ex-adenoma [6].
Conclusion
Pleomorphic adenoma of the lacrimal gland is a rare pathology that is often revealed by signs of orbital compression. Once the diagnosis is suspected on MRI, a monobloc excision without invasive surgery is essential to avoid recurrences that are difficult to treat.
References
- Elouarradi H and Daoudi R. “Eyelid S-shape deformation revealing a pleomorphic adenoma” Pan Afr. Med. J., 2014; 17: p. 114. doi: 10.11604/pamj.2014.17.114.3948.
- Ducasse A, Merol JC, Bonnet F, Litré F, Arndt C, Larré I. “Tumeurs de l’orbite de l’adulte,” Fr. Ophtalmol., 2016; 39(4): pp. 387–399, 2016, doi: 10.1016/j.jfo.2015.11.009.
- Scientifiques E, Tous ESAS. “Imagerie de l ’ œil et de l ’ orbite : radiologie , échographie , scanner et résonance magnétique,” 2000; 14(19): pp. 25–29. doi: 10.1016/S1879-8551(19)50487-0.
- Rose GE, Wright JE. “Pleomorphic adenoma of the lacrimal gland.,” J. Ophthalmol., 1992; 76(7): pp. 395–400. doi: 10.1136/bjo.76.7.395.
- Abouchadi A, Capon-Degardin N, Martinot-Duquennoy V, Pellerin P. “Eyelid crease incision for lateral orbitotomy” Chir. Plast. Esthet., 2005; 50(3): pp. 221–227. doi: 10.1016/j.anplas.2005.01.002.
- Westwood AC, Chengot P. “Carcinoma ex pleomorphic adenoma,” Diagnostic Histopathol., 2018; 24(10): pp. 429–431. doi: 10.1016/j.mpdhp.2018.08.005.

