Atypical Appearance of a Subdural Hematoma Plugging a Cortico-pial Branch Dissection
Soukaina Bahha*, Chaimae Abourak, Asmae Guennouni, Salma El Aouadi, Firdaous Touarsa, Najwa El Kettani, Meriem Fikri and Mohammed Jiddane
Radiology Department, Ibn Sina Hospital, Rabat, Morocco
Received Date: 28/11/2024; Published Date: 03/01/2025
*Corresponding author: Soukaina BAHHA, Radiology Department, Ibn Sina Hospital, Rabat, Rabat, Morocco
ORCID: https://orcid.org/0009-0007-9343-0999
Abstract
Background: Subdural hematoma has a typical appearance known to radiologists, but this article reports one of the atypical aspects of this diagnosis that radiologists should be aware of.
Case Presentation: 40 years old man, victim of a public road accident, and having already been victim of a public road accident 3 months previously with cerebral impact, presenting 4 days after the recent accident with right hemi cranial headaches, vertigo, and three episodes of vomiting, clinical examination found a conscious but confused patient with a GCS of 14/15, with facial injuries. A injection-free cerebral CT scan was ordered, and came back in favor of bilateral hemispheric cerebral subdural collections, which were markedly hypodense, possibly related to post-traumatic hygroma ( considering his past history), it also showed a right frontal extra-axial cerebral formation embedded within the chronic subdural collection, oval, well limited, spontaneously hyperdense (hematic density) with no fracture facing it, with individualization of a vascular structure within it after injection of contrast agent.
Conclusion: Post-traumatic intracerebral hemorrhage is an extreme medical and neurosurgical emergency. Cerebral imaging, and especially CT scan, given its availability and rapidity, is of considerable help in the diagnosis and management of patients suffering from cerebral trauma. Radiologists must be familiar with the atypical appearance of cerebral hematoma to optimize patient care.
Abbreviations: MRI: Magnetic Resonance Imaging; CT: Computed Tomography; MVAs: Motor Vehicle Accidents; SDH: Subdural Hematoma
Introduction
Intracranial hemorrhage is common in the setting of trauma, and is easily detected by radiological neuroimaging [1].
Motor vehicle accidents (MVAs) are the most frequent overall cause of head injuries, followed by falls. Falls tend to affect the very young or elderly, while MVAs mainly affect young adults.
Cerebral imaging is extremely important and provides a great contribution to the diagnosis of traumatic brain injuries.
We report in this article the case of a young adult who was the victim of a traffic accident and in whom the cerebral CT scan found an atypical aspect of a cerebral hematoma.
This article is specific for two reasons: firstly, the atypical form of the hematoma, which is neither subdural nor extradural, and secondly, the fact that it is embedded in a hemispheric subdural collection.
No literature was found reporting a case similar to this one.
Case Report
Our patient is 40 years old, with no medical or surgical history, victim of a public road accident (motorcyclist hit by a car), having already been victim of a public road accident 3 months previously with cerebral impact, presenting 4 days after the recent accident with right hemi cranial headaches, vertigo, and three episodes of vomiting, clinical examination found a conscious but confused patient with a GCS of 14/15, with facial injuries.
A injection-free cerebral CT scan was ordered, and came back in favor of bilateral hemispheric cerebral subdural collections, which were markedly hypodense, possibly related to post-traumatic hygroma ( considering his past history), it also showed a right frontal extra-axial cerebral formation embedded within the chronic subdural collection, oval, well limited, spontaneously hyperdense (hematic density) with no fracture facing it, with individualization of a vascular structure within it after injection of contrast agent (appearance suggestive of a hematoma plugging a cortico-pial vessel dissection).
A cerebral MRI was also performed, which confirmed the results found on the CT scan and also showed ischemic contusions in the contralateral cerebral parenchyma, and signs of diffuse meningeal hemorrhage, as well as chronic foci of contusion and hemosiderin deposits in the cortical sulci (probably related to his previous trauma).
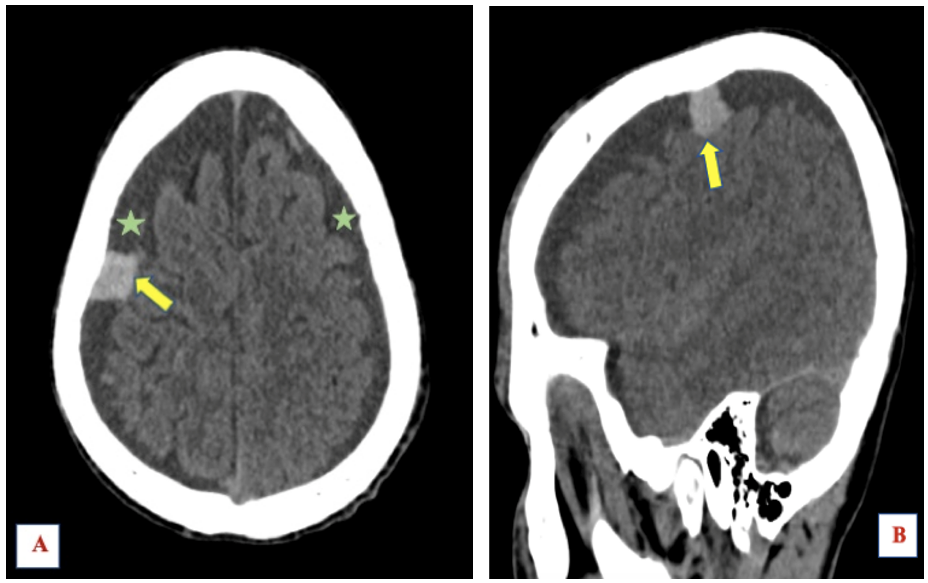
Figure 1: Injection-free cerebral CT scan parenchymal window showing right extraaxial frontal lesion spontaneously hyperdense (yellow arrow) and bilateral hygromas (green stars), (A): axial section, (b): sagittal section.
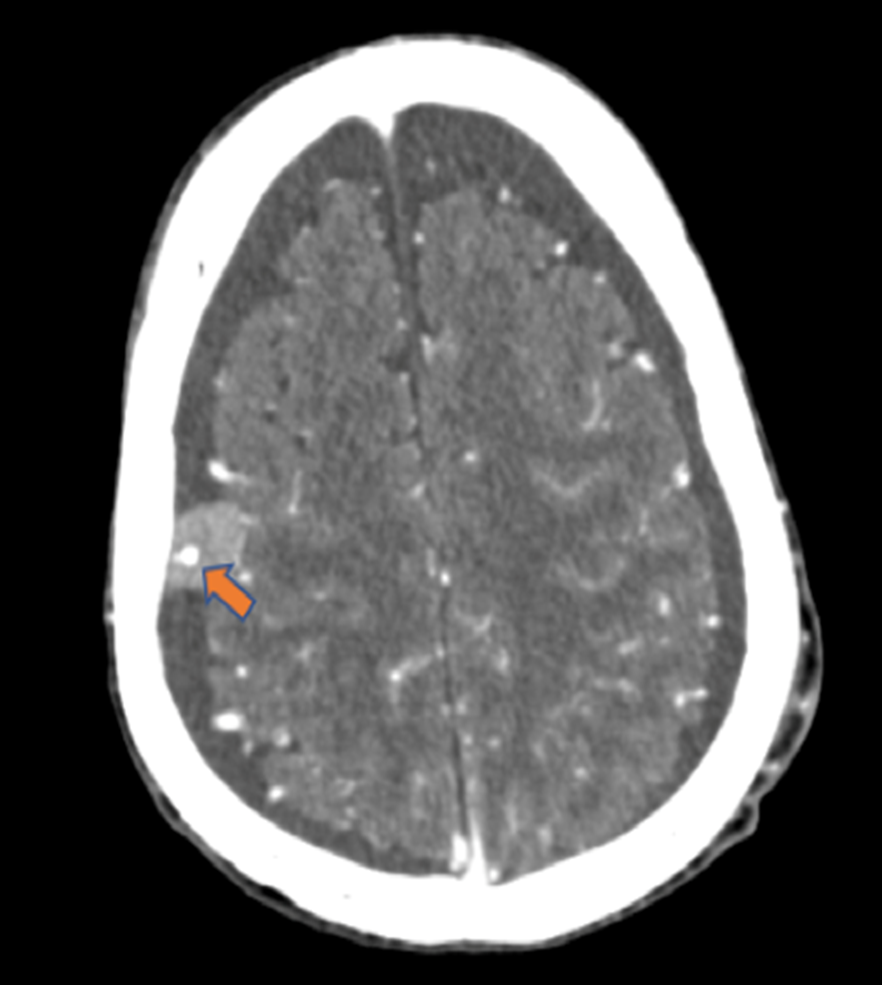
Figure 2: Cerebral CT scan with injection showing the right extra-axial frontal lesion with a vascular structure within it (orange arrow).
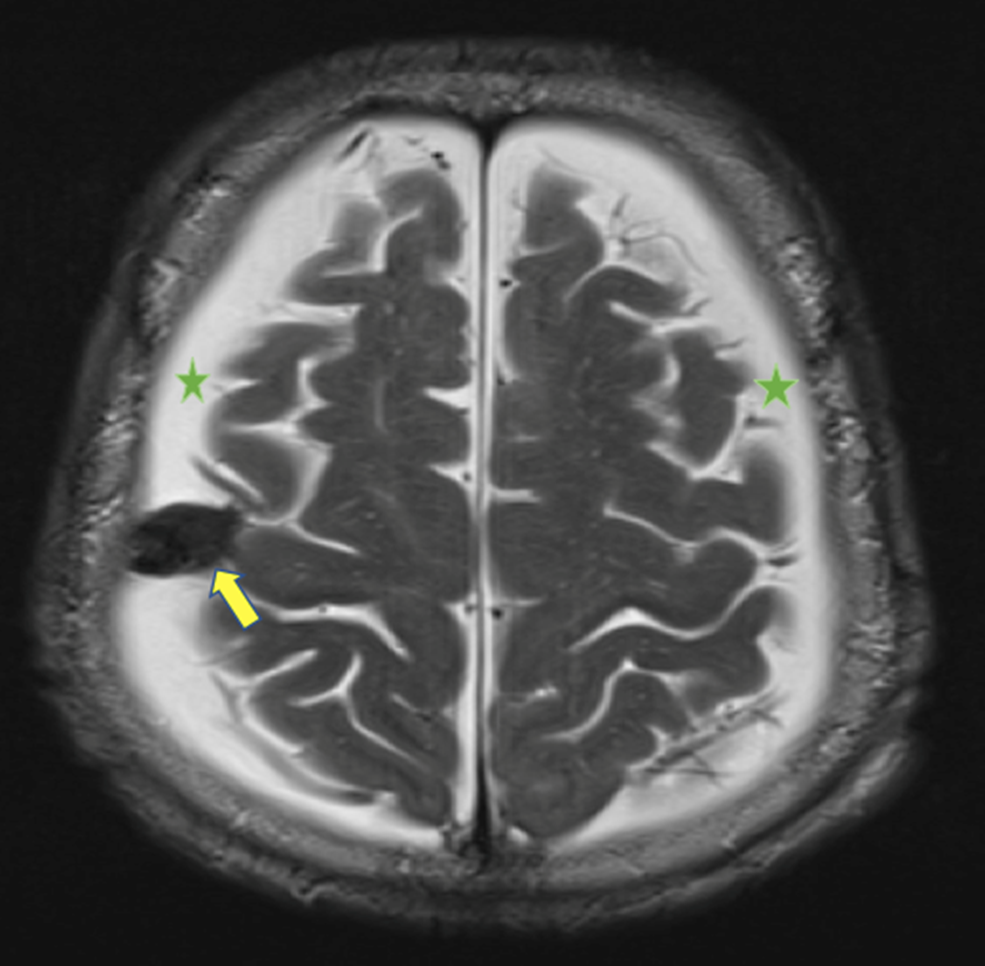
Figure 3: T2-weighted MRI image in axial section showing the hematoma embedded in the subdural collection, which is T2 hyposignal.
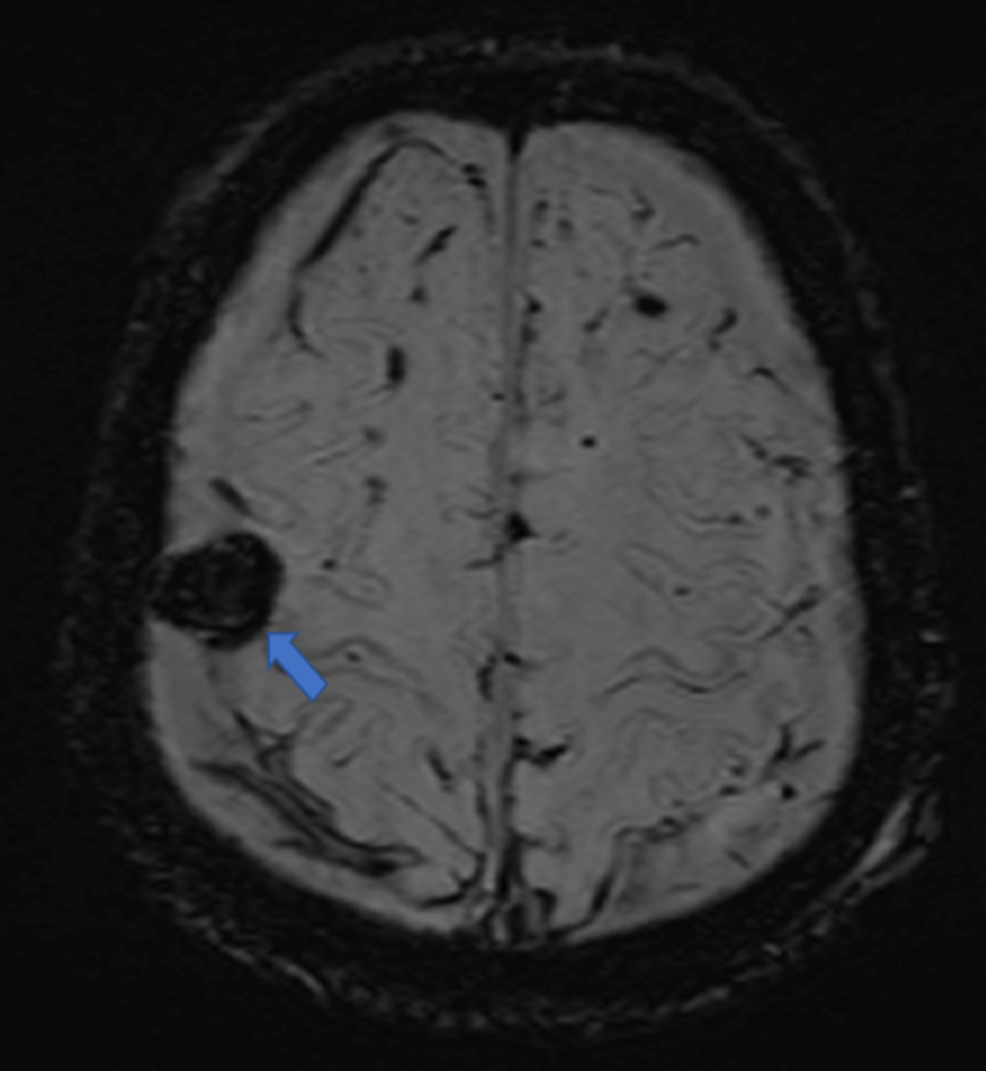
Figure 4: SWI sequence MRI image, axial section showing the hematoma which is in asignal (black): blue arrow.
Discussion
Subdural hematomas are seen in 10-20% of patients with traumatic brain injury [2]. Approximately 95% of subdural hematomas occur in the frontoparietal region, and around 10-15% of subdural hematomas are bilateral. in our patient, it was a unilateral hematoma located in the frontal region.
The brain scan is the imaging modality of first choice for skull assessment. Recent advances in imaging allow very thin imaging sections to be obtained, and also to arrange images in several planes. It is fast, widely available and sensitive for assessing dense bony structures, and the detection of intracranial hemorrhage in the acute phase, which appears spontaneously hyperdense with an attenuation coefficient in the range of 80–90 HU [1].
The typical CT appearance is a spontaneously hyperdense, crescent-shaped, homogeneous pericerebral collection with anteroposterior extension at a hemispheric convexity, its density depends on its age: when hyperdense, it's an acute hematoma (6 hours - 3 days), when progressively isodense, it's subacute, and when hypodense, it's either hyperacute or chronic [3].
the atypical appearances of acute subdural hematoma found in the literature were mainly cases of subdural hematoma with mixed density.
On MRI, the imaging characteristics of parenchymal hemorrhage are variable and change with the age of the blood. There are five stages of hemorrhage: hyperacute, acute (1-2 days), early subacute (2-7 days), late subacute (1 week to several months) and chronic (1 week to several months) [1]. In our case it was an early subacute hematoma.
SWI is a new magnetic resonance imaging method that maximizes sensitivity to the effects of magnetic susceptibility and is extremely sensitive for the detection of microhemorrhages [1].
Subdural hematoma has a venous origin due to stretching, laceration and rupture of the cortical veins that cross the meningeal spaces to join the adjacent venous sinuses. It results either from direct impact or, more frequently, from acceleration/deceleration, it is favoured by the enlargement of the pericerebral spaces, which increases the tension of the "bridge veins" and leads to their rupture.
In more than 70% of cases, there are lesion associations with subarachnoid hemorrhage, diffuse axonal lesions and/or parenchymal contusions, which impact prognosis. These associated lesions are either homolateral, located close to the subdural hematoma, or contralateral = counter-cut lesions [4]. In our patient's case, we found signs in favor of acute meningeal hemorrhage, as well as ischemic contusion lesions on the counter-lateral side of the hematoma, which were highlighted on MRI.
subdural hematoma is theoretically a neurosurgical emergency if its thickness exceeds 5mm, with displacement of the median line of more than 5mm. In practice, the indication for surgery is essentially made in the presence of a herniation, whatever the thickness of the subdural hematoma. it consists of evacuation of the hematoma via a trepan hole and external drainage, with a very poor prognosis (35-90% mortality) due to associated lesions (involvement, oedema, secondary ischemia). Mortality is doubly higher in cases of combined subdural hematoma and contusions than in isolated subdural hematoma. Strict monitoring in a neurosurgical environment is essential [4].
Conclusion
Post-traumatic intracerebral hemorrhage is an extreme medical and neurosurgical emergency. Cerebral imaging, and especially CT scan, given its availability and rapidity, is of considerable help in the diagnosis and management of patients suffering from cerebral trauma. Radiologists must be familiar with the atypical appearance of cerebral hematoma to optimize patient care.
References
- Rincon S, Gupta R, Ptak T. Imaging of head trauma, in Handbook of Clinical Neurology. Elsevier, 2016; p. 447‑477. doi: 10.1016/B978-0-444-53485-9.00022-2.
- Ahizoune A, Satte A, Ajamat M, Raggabi A, Lemnouer A, Bourazza A. Neuromeningeal tuberculosis in HIV-negative patients: a retrospective study in Rabat, Morocco. Pan Afr. Med. J., 2022; 43. doi: 10.11604/pamj.2022.43.31.28669.
- Young RJ, Destian S. Imaging of traumatic intracranial hemorrhage. Neuroimaging Clin. N. Am., 2002; 12(no 2): p. 189‑204. doi: 10.1016/S1052-5149(02)00003-5.
- Harbury OL, Provenzale JM, Barboriak DP. Vertex epidural hematomas: imaging findings and diagnostic pitfalls. Eur. J. Radiol., 2000; 36(no 3): p. 150‑157, déc. 2000, doi: 10.1016/S0720-048X(00)00175-3.
- Provenzale J. CT and MR imaging of acute cranial trauma. Emerg. Radiol., 2007; 14(no 1): p. 1‑12. doi: 10.1007/s10140-007-0587-z.

