Extensive Dermatophytosis Due to Self-Medication: About Two Cases and Literature Review
Rachid Douge1,2,*, Mourad Belaouni1, Fouzia Merhari1,2, Manal El Yadari1,3 and Mohammed Er-rami1,4
1Parasitology-Mycology Department, Moulay Ismail Military Hospital, Meknes, Morocco
2Abdelmalek Essaâdi University, Faculty of Medicine and Pharmacy, Tangier, Morocco
3Mohammed V University, Faculty of Medicine and Pharmacy, Rabat, Morocco
4Sidi Mohamed Ben Abdellah University, Faculty of Medicine and Pharmacy, Fez, Morocco
Received Date: 27/11/2024; Published Date: 02/01/2025
*Corresponding author: Dr. Rachid Douge, Address: Department of Medical Biology, Mohamed VI University Hospital Center of Tangier, Morocco
Abstract
Self-medication, particularly with steroids is very common in the context of dermatophytosis with the possible complication was spread of infection. We report two cases of extensive dermatophytosis following irrational use of steroids by self-medication. In the first case, the starting point of the fungal infection was untreated Trichophyton rubrum onychomycosis of the right foot, due to self-medication with a topical steroid, the infection spread to the foot and leg on the same side. In the second case, it was Microsporum canis ringworm of the scalp, and after self-medication with steroids, the infection spread to the face, left ear and right arm. Evolution of our cases was favorable after discontinuation of steroids and initiation of antifungal therapy. This work illustrates the dangers and risks of self-medication, notably the use of steroids in the treatment of dermatophytosis, and justifies the importance of a mycological diagnosis before any therapy in this context.
Keywords: Dermatophytosis; Self-medication; Topical steroid; Antifungal
Introduction
Dermatophytosis are cosmopolitan superficial fungal infections of the skin and appendages, caused by microscopic keratinophilic filamentous fungi from three genera: Trichophyton, Microsporum and Epidermophyton. They affect millions of people worldwide, and are most frequently encountered in the daily practice of dermatology and of medical mycology [1,2]. These infections, which manifest as pruritic lesions and scaling, can not only cause physical discomfort, but also have a considerable impact on patients' quality of life [2,3].
The practice of self-medication is very common in this context, particularly through the use of topical steroids. Although this approach may seem convenient, it presents major complications and risks, notably masking the symptoms of fungal infections and promoting their spread [3,4].
We report two cases of extensive dermatophytosis following irrational self-medication with steroids. Through the analysis of this case report and of a literature review, we highlight the consequences of self-medication particularly steroids in the treatment of dermatophytosis, as well as its clinical, biological and therapeutic aspects.
Cases Presentation
Case 1
This is a 54-year-old female, housewife, with no specific pathological history notably of diabetes, psoriasis or other autoimmune disease, and no immunosuppressed background. She had presented with untreated toenail lesions for two years, with erythematosquamous and pruritic lesions appearing for four months on the foot and right leg, following self-medication with a topical corticosteroid (Betamethasone dipropionate 0.05%). Clinical examination finds an erythematosquamous placard associated with scratching lesions on the foot and distal leg of the right lower limb. Disto-lateral onychomycosis of toes on the same foot was also found, characterized by hyperkeratosis, onycholysis, xantonychia and melanonychia, associated with plantar dermatophytitis (Figure 1).
Direct examination of nail samples and skin rash after clearing with a potassium hydroxide preparation (10%) was positive, showing the presence of mycelial filaments. Cultures on Sabouraud-chloramphenicol and Sabouraud-chloramphenicol-cycloheximide (Actidione®) media at 28°C were positive on the 6th day of incubation, in favor of Trichophyton rubrum, of which macroscopic examination showed pleated colonies with a downy appearance, whitish on the front and yellowish-brown on the back, and whose microscopic examination after staining with lactophenol blue, has observed fine septate and poorly branched filaments with a rare pyriform microconidia arranged in an acladium pattern (Figure 2).
Treatment based on a combination of oral terbinafine 250mg and topical fluconazole for three months was prescribed for this patient after discontinuation of steroid. The evolution was favorable, with complete regression of lesions.
Case 2
An 11-year-old boy, schoolchild, with no notable personal and family pathological history, particularly of atopy. He presented for three months with scaly lesions on the scalp. At the interrogation, he reported a contact with cats in the street, and his mother reported that two months ago she applied to him a keratolytic corticosteroid lotion and topical (Betamethasone + Salicylic acid), by self-medication, for scalp lesions and for a small erythematous and pruritic patch on the forehead. The evolution was marked by the extension of lesion to the face, left ear and right arm. Clinical examination revealed three scaly lesions on an erythematous background, 3 to 4cm in diameter on the scalp, with fragile, easily peeled hair. Examination also revealed multiple small scaly lesions on the forehead, cheek and left ear, with a large scaly lesion on the right arm (Figure 3).
Samples of scalp and skin lesions were taken, from whom direct examination was positive after clearing with a potassium hydroxide preparation (10%), revealing the presence of mycelial filaments in both samples and a microsporic form of endo-ectothrix parasitism for hair samples (Figure 4). After seven days of incubation on Sabouraud-chloramphenicol and Sabouraud-chloramphenicol-cycloheximide (Actidione®) media at 28°C, culture yielded flat, spreading, white to cream-colored colonies with “asbestos rod” extensions and a fine white down in the center. Microscopic examination of the cultures with lactophenol blue showed the presence of racket-shaped mycelial filaments and spindle-shaped macroconidia with thick, rough walls and an average of nine cubicles, sometimes with curved button ends (Figure 5). All these features were in favor of Microsporum canis.
Our patient was treated with a combination of griseofulvin 250mg orally and terbinafine topically for two months after stopping the current treatment. The outcome was favorable with healing of lesions.

Figure 1: Onychomycosis of toes and dermatophytic skin caused by Trichophyton rubrum.
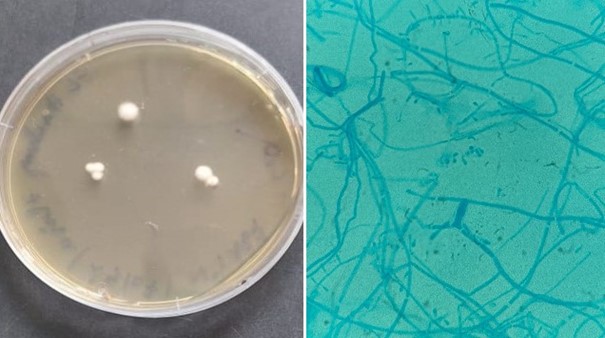
Figure 2: Macroscopic and microscopic (x100) appearance of Trichophyton rubrum colonies.

Figure 3: Scalp ringworm and dermatophytic skin lesions caused by Microsporum canis.
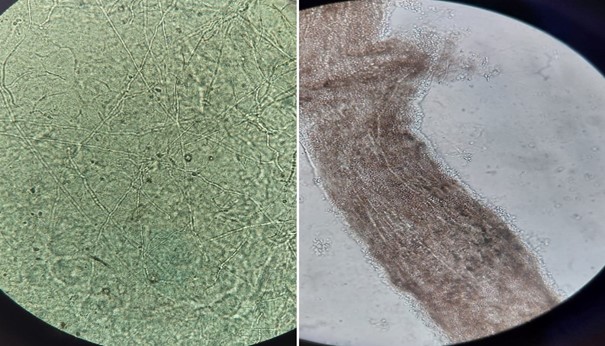
Figure 4: Direct examination (x40) of skin and hair samples showing the presence of mycelial filaments and a microsporic endo-ectothrix hair parasitism.

Figure 5: Macroscopic and microscopic (x100) appearance of Microsporum canis colonies.
Discussion
Superficial skin mycosis, mainly caused by dermatophytic fungi, are part of the world's most frequent fungal infections, affecting over 20% of individuals, particularly in developing countries. Among these infections, dermatophytosis is the most usual [3,5].
The inappropriate use of drugs for dermatophytic infections, particularly through self-medication, is a widespread, growing and worrying phenomenon in many parts of the world [2,6]. Despite the frequency and seriousness of this phenomenon, there are few studies that have evaluated its different aspects and mainly come from India. Accordingly, the data on prevalence of self-medication in this context are poor and varies considerably from study to another. Indeed, one Indian study shows that around 62.26% of dermatophytosis patients self-medicate [7]. Another, reports a self-medication rate of around 39.47% for fungal skin infections [1]. Furthermore, according to the literature on this subject, the most commonly used drugs are topical steroids alone or combined with antifungal agents and/or with antibiotics [1,4,8,9]. The proportion of patients who used creams containing steroids ranged from 30% to 93% depending on the study [1-10], while the use of antifungals alone was much less common, and concerned only 5.7% to 47% of cases [1,4,9,10].
This behavior is linked to a lack of medical information among patients, the absence of professional advice in some over-the-counter settings, and the perception of these drugs as quick and effective solutions for inflammatory skin conditions where the patient's main concern is rapid relief of pruritus and itching [2,4,6,8]. This explains the widespread practice of self-medication in these conditions, particularly with corticosteroids, due to their powerful immunosuppressive effect, offering temporary symptomatic relief while masking the visible signs of the underlying fungal infection [2,3,8]. In some countries, easy access to these remedies without a medical prescription accentuates the risk of their improper use [4,5,8].
Possible complications of self-medication in dermatophytosis include delayed diagnosis, spread of the condition, chronicity and recurrence of lesions, and resistance to treatment [2,3,8]. In fact, patients who have applied corticosteroids to dermatophytosis often respond more slowly to standard antifungal treatments and may require prolonged therapies or drug combinations, making therapeutic management both clinically and economically burdensome [3,9].
Extensive dermatophytosis refers to infections limited to the stratum corneum but with multiple or widespread lesions [11]. These forms of dermatophytosis reported in the literature, mainly concerned patients with innate or acquired immunodepression, as well as cases treated with systemic and/or local corticosteroids, following initial diagnosis errors [11,12]. The lesions presented by our two cases were relatively misleading in their localization and clinical aspects, simulating eczema in the first case and atopic dermatitis in the second case. Due to self-medication and the use of steroids, the infection worsened and the lesions extended. Such presentations often constitute a diagnostic trap in general medical consultations.
This case report clearly illustrates the dangers of self-medication, in particular the use of topical corticosteroids in the treatment of dermatophytosis. It has been shown that the application of these steroids to infected areas can alter the local immune response, thereby promoting the proliferation of dermatophytes, making the host more susceptible to infection progression [3,5,8]. This reaction is the source of corticosteroid modified lesions or “ringworm incognito”, which have become more common in recent years. They are characterized by atypical, extensive lesions that often resemble other skin conditions, making clinically diagnosis more difficult in some cases [3,6,12,13]. Therefore, a mycological examination and fungal culture are recommended at the beginning of treatment for confirmation [13].
There is currently no consensus on the treatment of extensive dermatophytosis, but some studies recommend the combination of systemic and topical antifungal agents, even if they disagree on the combination of the same or different classes of antifungal drugs. However, most authors opt for a combination of antifungals from different classes in order to achieve a synergistic effect, reduce the risk of treatment resistance and ensure broader coverage [13]. This combination should preferably be made between a systemic antifungal and a topical antifungal, which reaches a high concentration at the site of action [13,14]. In our cases, treatment with this antifungal combination for 8 weeks was successful.
These cases underline the crucial importance of adequate patient education on the risks associated with self-medication, and the need for controlled and informed access to drugs and pharmaceutical products. Greater awareness and appropriate regulation are essential to prevent complications from these practices, improve patient prognosis and reduce healthcare costs associated with prolonged and complex management.
Conclusion
Symptomatology of dermatophytosis is not pathognomonic and often mimic other dermatoses diseases, leading some patients to self-medicate and use inappropriate drugs, with the possible consequences of delayed diagnosis and extension of dermatophytic lesions. A mycological diagnosis is strongly recommended before any treatment, and awareness of this problem is therefore necessary to prevent its various complications, which are a growing threat.
Declarations
Authors' contributions: All authors contributed to the conception of the manuscript. All authors read and approved the final version of this manuscript.
Competing interests: The authors declare no competing interests.
Funding: No funding source was involved in this study.
Consent for publication: informed consent was obtained from the patient and from the child's parents for the publication of these cases and all the accompanying images.
Acknowledgements: None
References
- Bagchi C, Mukherjee S, Chatterjee K. An outpatient-based observational study on demography, self-medication practice, and prescribing pattern in dermatophytosis at a tertiary care teaching hospital in Eastern India. National Journal of Physiology, Pharmacy and Pharmacology, 2022; 12(8): 1117-1124.
- Meena D, Hazarika N, Chauhan P, Goyal P. Steroid abuse, quality of life, and various risk factors in dermatophytosis: a cross-sectional observational study from a tertiary care center in northern India. Acta Dermatovenerol APA, 2022; 31(4): 135-140.
- Manickam N, Manimaran P T, Gopalan K, Somasundaram K, Vellaisamy S G. A Clinico-Epidemiological Study to Assess the Impact on Quality of Life and Financial Burden in Patients with Dermatophytosis. J Commun Dis, 2024; 56(1): 36-42.
- Poudyal Y, Joshi SD. Medication Practice of Patients with Dermatophytosis. J nepal Med assoc, 2016; 55(203): 7-10
- Choudhary N, Panday D, Mishra D, Lahiri K, Sil A, Chaddha R. Over-the-Counter Medicine-Seeking Behavior in Patients with Dermatophyte Infections Across Various Socioeconomic Strata: A Cross-Sectional Study. Cureus, 2024; 16(1): e51686.
- Lakhani S J, Bilimoria F, Lakhani J D. Adverse effects of steroid use in dermatophytic infections: a cross-sectional study. Journal of Integrated Health Sciences, 2017; 5(2): 63-68.
- Koshley V, Halwai A K, Koshley S B, Kurrey P K, Jaiswal S. Treatment Pattern of dermatophytosis at the outpatient clinic of a tertiary healthcare hospital of Chhattisgarh, Central India. Indian Journal of Clinical and Experimental Dermatology, 2018; 4(4): 327-330.
- Khurana A, Gupta A, Sardana K, Sethia K, Panesar S, Aggarwal A, et al. A prospective study on patterns of topical steroids self-use in dermatophytoses and determinants predictive of cutaneous side effects. Dermatologic Therapy, 2020; 33(4): e13633.
- Dabas R, Janney M S, Subramaniyan R, Arora S, Sandeep Lal V, Donaparthi N. Use of Over-the-Counter Topical Medications in Dermatophytosis: A Cross-Sectional, Single-Center, Pilot Study from a Tertiary Care Hospital. Indian Journal of Drugs in Dermatology, 2018; 4(1): 13-17.
- Paudel S, Parajuli N, Dahal S C, Paudel S. Improper Use of Topical Corticosteroids in Tinea Infections in a Tertiary Care Hospital. J Nepal Health Res Counc, 2021; 19(50): 71-75.
- Rouzaud C, Hay R, Chosidow O, Dupin N, Puel A, Lortholary O, et al. Severe Dermatophytosis and Acquired or Innate Immunodeficiency: A Review. Fungi (Basel), 2015; 2(1): 4.
- Gahalaut P, Mehra M, Mishra N, Rastogi M, Bery V. Clinicoepidemiolgic Profile of Dermatophytosis in the Elderly- A Hospital Based Study. Nepal Journal of Dermatology, Venereology & Leprology, 2021; 19(2): 26-33.
- Shenoy M, Poojari S, Rengasamy M, Vedmurthy M, Barua S, Dhoot D, et al. Management of Dermatophytosis: Real‑World Indian Perspective. Indian Dermatology Online Journal, 2023; 14(3): 347-356.
- Inamadar A, Rengasamy M, Charugulla S N. Treatment Approach for Superficial Dermatophytosis Infections and Factors Contributing for Noncompliance to Antifungal Therapy in India: An Epidemiological Survey. Clinical Dermatology Review, 2022; 6(1): 15-21.

