Headache in an Elderly, Traumatic Subarachnoid Fat Emboli Secondary to Ruptured Spinal Dermoid Cyst
Mohamed Hussein El Damasy1,*, Arshad Ali Khan2, Ibriak Mohamed3 and Islam Ashor3
1Internal Medicine Senior House officer, Whipps Cross University Hospital, London
2ED consultant, Basildon university hospital, Essex, UK
3A&E clinical fellow, Basildon university hospital, Essex, UK
Received Date: 26/11/2024; Published Date: 20/12/2024
*Corresponding author: Mohamed Hussein El Damasy, MBBCH (hons), MRCSed, Internal Medicine Senior House officer, Whipps Cross University Hospital, London
Abstract
Following a referral from her general practitioner, a lady in her 70s in good health arrived at our emergency room. She had been experiencing headaches for two months, which were mostly caused by a fall she had during her shower that resulted in her lower back being hit. The headaches were intermittent but progressing. After admission, a thorough cranial and spinal MRI scan along with a perineural sacral dermoid cyst validated the first CT scan of the head's distributed subarachnoid fat emboli findings. The diagnosis was considered to be conservative since the neurospinal MDT reviewed the case and found it to be straightforward. The following few months have seen an improvement in the pa-tient's symptoms, who recovered well.
Background
An unusual form of fat embolism syndrome (FES) that affects the skull is called sub-arachnoid fat embolism (SFE). When a transthecal displacement of fatty marrow occurs due to a nearby spinal fracture or when a ruptured spinal or cranial dermoid cyst occurs, lipid-dense material may be deposited in the subarachnoid space [1]. The incidence of cerebral fat embolism is 0.9%–2.2% [2]; however, because transthecal fat embolism is a rare disorder, there are no reliable data on the incidence or prevalence of this condition in the literature. Due to the fact that the severity varies greatly based on the underlying rea-son, it is essential to diagnose the condition as soon as possible with a proper head scan (ideally an MRI of the brain and spine).
Our case demonstrates the fact that this abnormality can ensue as a result of minor trauma with no associated fracture or neurological deficit.
Case Presentation
We describe the case of a lady in her 70s who came to our emergency department on a referral from her General Practitioner (GP) with complaints of a generalised headache that had been becoming worse over the previous two months and was intermittent. She slid in the bathtub and fell on her lower back during a shower, which is when the discomfort first began. She didn't seek emergency medical assistance because the injury wasn't serious and she wasn't experiencing any additional symptoms. A non-contrast CT scan of the head was ordered by the GP (Figure 1), which revealed a number of dispersed, small hy-podense foci in the basal cisterns and ventricular system.
The abnormality seen in the CT scan guaranteed admission to the acute medicine ward for additional monitoring and MRI scanning in the hopes of elucidating the nature and po-tentially the source of these foci, even though the patient remained vitally and clinically stable, had no neurological deficit, and had no more complaints. An MRI of the head and entire spine was done, and the results did certainly identify the offender. MRI imaging re-vealed that the hypodense foci observed in the CT scan were consistent with fat emboli (Figure 2). The source of these fat emboli was identified by a spinal MRI scan as a 38 mm perineural cyst posterior to the S2 vertebra. The cyst had a few T1 hyperintense foci consistent with intralesional fat and was most likely a dermoid cyst (Figure 3). The overall appearance was suggestive of disseminated fat droplets within the subarachnoid space secondary to a traumatic rupture of the dermoid cyst.
The patient was discharged with her condition remaining stable and uncomplicated, and a referral to the neurospinal surgery team was established. After discussing her case with the neurospinal surgery MDT, it was determined that conservative treatment would be the best course of action, with no attempt at surgery.
Investigations
● Non-contrast CT scan of the head revealed scattered several tiny hypodense foci throughout the ventricular system and the basal cisterns.
● MRI Head revealed tiny hypodense foci scattered throughout the ventricular system demonstrating T1 hyperintense signal with signal drop out on the fat saturation se-quences in keeping with fat emboli.
● MRI spine revealed 38 mm perineural cyst posterior to the S2 vertebra containing a few T1 hyperintense foci in keeping with intralesional fat likely representing a der-moid cyst.
Differential Diagnosis
Given the patient’s presentation and history of trauma a skull fracture and pneumo-cephalus is a possibility that would be supported by the hypodense foci that looks like air locules inside the cranium.
Cerebral fat embolism was more likely to be the top differential after discovering the patient’s spinal dermoid cyst in her MRI scan as fatty material grossly resembles air hypo-density on a CT scan of the head.
Treatment
The patient was treated conservatively with reassurance, pain management and outpa-tient follow ups to ensure non-progressive course of her cerebral symptoms.
Outcome and Follow-Up
The patient has generally improved, her headache took a regressive course, feels gener-ally better especially after being assured by the specialist that the burden of her emboli wasn’t severe and less likely to affect her on the long run.

Figure 1: Axial view of non-contrast CT scan of the head shows several hypodense foci scattered throughout the ventricular system.
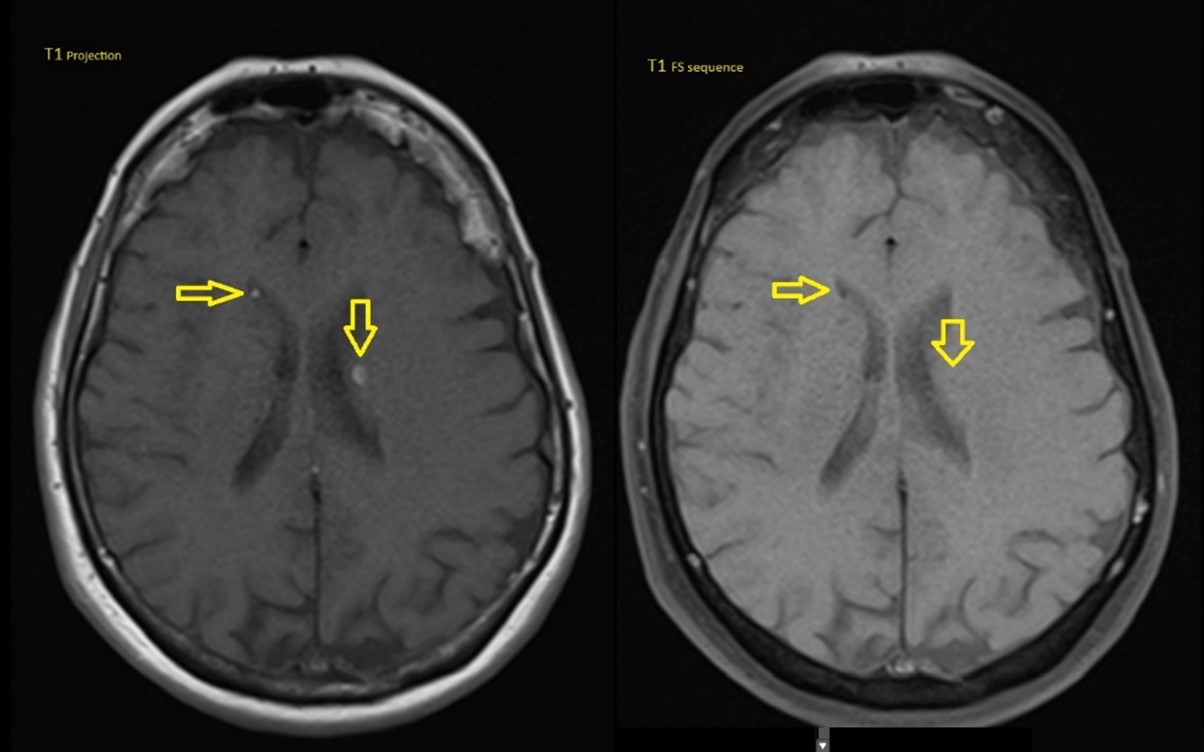
Figure 2: T1 and fat saturation projection of the brain MRI showing hyperintense foci in the subarachnoid space that seem to be of fatty nature on the fat saturation sequence.
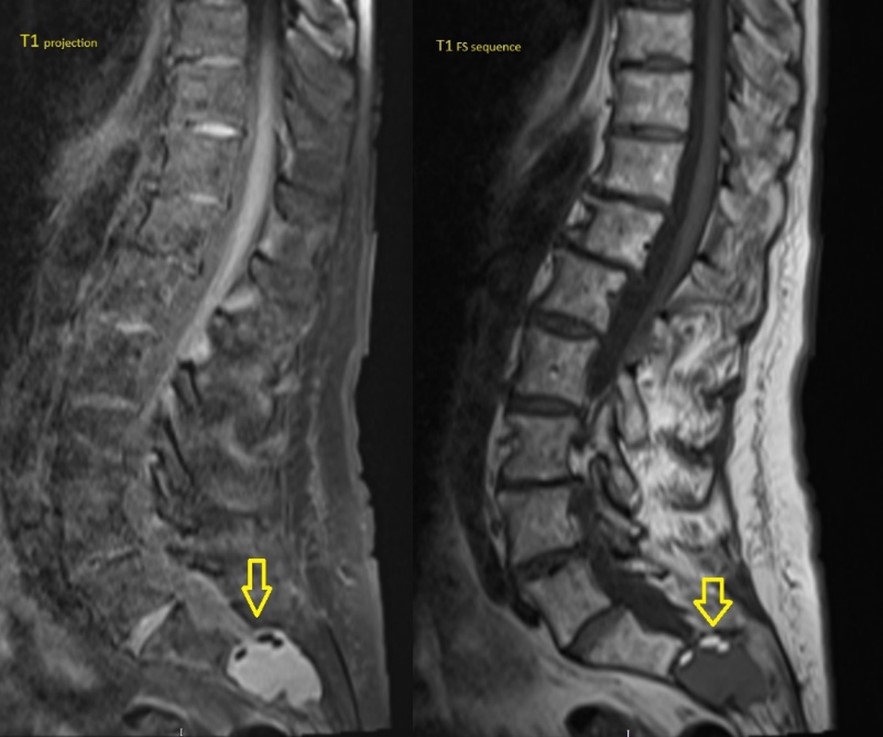
Figure 3: T1 and Fat Saturation projection of the spinal MRI scan showing the sacral dermoid cyst with intralesional fat proven on the fat saturation sequence.
Discussion
Benign spinal tumours consisting of skin and skin appendages with embryonic origin are called spinal dermoid cysts. Usually asymptomatic, incidentally found in both genders with the same aetiology. Aseptic chemical meningitis is caused by the rupture of a der-moid cyst and the subsequent discharge of its contents into the subarachnoid space, which travels retrogradely to the cranium. The fatty acids in the ruptured cyst cause se-vere irritation [3].
Dissemination of fatty material in the subarachnoid space and intraventricularly is un-common. Subarachnoid Fat Embolism (SFE) happens secondary to Spontaneous, Trau-matic or iatrogenic rupture of lipid-rich cranial and spinal tumors mostly dermoid or epi-dermoid cysts and teratomas. Release of fatty material from bone marrow into CSF is more commonly linked to sacral fractures which can occasionally be associated with subarachnoid hemorrhage [1]. In 1977, K Maravilla described the earliest intraventricular fat deposition secondary to a spontaneously ruptured intracalvarial dermoid cyst. Trau-matic rupture of intracranial dermoid cysts is rare unlike spinal dermoids as in our patient.
The clinical presentation of Cerebral Fat Embolism (CFE) is highly variable as it can hap-pen in the context of fat embolism syndrome (diagnosed first by Von Bergmann in 1873 [4]) most commonly with multi-system dysfunction or in isolation. Fat embolism syn-drome commonly involves the lungs, brain, skin and occasionally generalized symptoms such as fever, hematuria, disseminated intravascular coagulation (DIC), shock and death [5]. Neurological symptoms could be observed in 33-86% of patients including confusion, agitation, altered consciousness, seizures or even coma [5]. Having mentioned that, SFE can present with subtle symptoms not guaranteeing immediate medical attention like intermittent headache as described in our case.
Diagnosis of transthecal CFE has proven to be challenging due to the fact that clinicians (especially acute care clinicians) are not oriented to such condition given its rarity and the complex pathophysiology that requires multiple interacting factors. CT scan of the brain might show hypoattenuating material that can be difficult to visually differentiate from gas (Pneumocephalus). The Gold standard imaging is MRI with contrast which shows high signal intensity on both T1- and T2-weighted images, while gas has very low signal intensity [2]. However, MRI is not readily available and much more expensive in comparison with CT, especially in acute setting.
M Scarpino et al [2] recommend the use of intravenous corticosteroids (Dexamethasone or Methylprednisolone) for both the prevention and treatment of CFE syndrome despite conflicting evidence which is mainly due to the lack of specific treatment guidelines, however symptomatic and supportive treatment remains the mainstay given the fact that most of the cases are self-limiting.
Lastly, even though this illness is uncommon, it's crucial to keep it in mind, particularly when trauma patients appear less cognizant. Early intervention and prompt recognition are essential.
Learning Points
- Subarachnoid fat embolization can happen in the context of a ruptured spinal or cra-nial dermoid cyst or transthecal displacement of fatty marrow owing to an adjacent spinal fracture.
- Minor trauma can cause subarachnoid fat embolism.
- The presentation of cerebral fat embolism is highly variable and can present in the acute setting or primary care with long standing headache.
- Not all patients with ruptured spinal dermoid cyst would require surgery, conserva-tive treatment is considered if the patient’s condition is uncomplicated.
Author contribution:
Mohamed Hussein El Damasy: Responsible for clinical care, design of the case report, wrote the manuscript, approval of the sub-mitted version.
Arshad Ali Khan: Involved in patient care, suggestion of case report, patient consenting and approval of final version for submission.
Ibriak Mohamed: Revised the manuscript, approved the version to be published.
Islam Ashor: Revised the manuscript, approved the version to be published.
Conflict of interest: None
References
- Marlena Berezniak, Piotr Palczewski, Jaroslaw Czerwinski, Malgorzata Deregowska-Cylke, Marek Golebiowski. Intracranial trasthecal fat migration after a sacral frac-ture: 2 case reports. American Journal of Case Reports, 2021; V22. DOI: 10.12659/AJCR.932760.
- Maenia Scarpino, Giovanni Lanzo, Francesco Lolli, Antonello Grippo. From the diag-nosis to the therapeutic management: Cerebral fat embolism, a clinical challenge. In-ternational Journal of General Medicine, 2019; 12: 39–48. DOI: 10.2147/IJGM.S177407.
- Gokhan kuyumcu, Miral Jhaveri. Ruptured spinal dermoid cyst. Canadian Journal of Neurological Sciences, 2017; 44: 5. DOI: https://doi.org/10.1017/cjn.2017.26.
- Von Bergmann E. Ein fall todlicher fettenbolic [incidence of the deadly fat embo-lism] Berl Klin Wochenscher, 1873; 10: 385.
- Shaikh N, Parchani A, Bhat V, Kattren MA. Fat embolism syndrome: clinical and imag-ing considerations: case report and review of literature. Indian J Crit Care Med, 2008; 12(1): 32-36. DOI: 10.4103/0972-5229.40948.

