Left Paraduodenal Hernia : About a Case
El Wassi A, Benzidane K*, El Kinani S, Benjelloun K, Hajri A, Erguibi D, Boufettal R, Jai R and Chehab F
Department of General Surgery, IBN ROCHD University Hospital Center, Casablanca, Morocco
Received Date: 08/11/2024; Published Date: 10/12/2024
*Corresponding author: Benzidane K, Department of General Surgery, IBN ROCHD University Hospital Center, Casablanca, Morocco
Abstract
Internal hernias are a rare pathology. They represent one of the rare causes of acute intestinal obstruction, discovered mainly intraoperatively. They correspond to a protrusion of the hollow abdominal viscera into an intra-abdominal or retroperitoneal orifice. The hernia orifice can be a pre-existing anatomical structure, such as Winslow's foramen, or pathological of congenital origin (foramen omental) or acquired (surgical, post-traumatic, infectious). Preoperative diagnosis is often clinically difficult due to non-specific symptoms and signs, so imaging examinations such as CT scan and small bowel transit play an important role.
We report the observation of a left paraduodenal hernia in a 21-year-old man.
Keywords: Internal hernia; Acute intestinal obstruction
Introduction
Internal hernias are a rare and still underestimated pathology [1]. They represent one of the rare causes of acute intestinal obstruction, discovered mainly intraoperatively. They correspond to a protrusion of the hollow abdominal viscera in an intra-abdominal or retroperitoneal orifice, but remaining inside the abdominal cavity. The hernia orifice can be a pre-existing anatomical structure, such as Winslow's foramen, or pathological of congenital origin (foramen omental) or acquired (surgical, post-traumatic, infectious) [2].
They can be revealed by an acute picture of intestinal obstruction, most often with an ischemic component due to vascular strangulation; they are responsible for 0.2 to 5.8% of small bowel obstructions [3]. Autopsy statistics show a frequency of 0.2 to 2% of internal hernias, most of which are asymptomatic [2].
Preoperative diagnosis is often clinically difficult due to non-specific symptoms and signs, so imaging examinations such as CT scan and small bowel transit play an important role.
They are associated with high morbidity and mortality due to the increased risk of strangulation and delayed diagnosis.
We report the observation of a left paraduodenal hernia in a 21-year-old man.
Case Report
21-year-old patient, with no medical or surgical pathological history, who presented to the emergency department for pain in the left hypochondrium associated with nausea and bilio-food vomiting, evolving for 7 days in a context of general condition preservation.
The clinical examination on admission found a conscious patient, stable on the hemodynamic and respiratory levels, with on abdominal examination, there was a non-distended abdomen, with tenderness of the left hypochondrium, without palpable mass and a rectal examination without abnormality with the presence of normo-colored stools.
An abdominopelvic CT scan performed objectified an agglutinated appearance of the proximal jejunal loops, not dilated, at the level of the left anterior pararenal space within a pseudo closed-loop sac measuring 97x 74 mm, with an attraction and a stretched appearance of the superior mesenteric vessels within it. It is associated with a moderate upstream duodenal dilatation without a hydro-aeric level, nor a detectable gastric stasis. In conclusion, CT scan in favor of a left paraduodenal hernia with duodenal dilatation upstream without signs of detectable CT scan digestive distress.
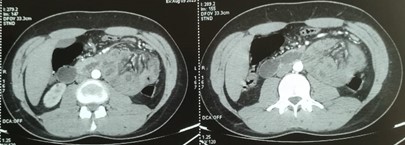
Figure 1: CT scan image showing the left paraduodenal hernia.
The biological assessment was without abnormalities:
- NFS : Hb:14,5 g/dl ; GB:5700 /mm3 ; PLQ:183000 /mm3
- Bilan hydro-electrolyte : Na+: 140 mg/l ; K+:3,7 mmol/l
- Renal assessment: Urea: 0.27g/l Creat: 8.1 mg/l
- CRP: 2.7 mg/l
The patient was admitted to the operating room as an emergency with exploration: presence of incarceration of the 1st jejunal loop at the level of the left paraduodenal dimple with an upstream duodenal distension, without signs of suffering. The gesture was a reduction in the contents of the hernia.
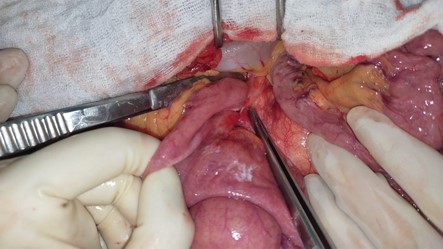
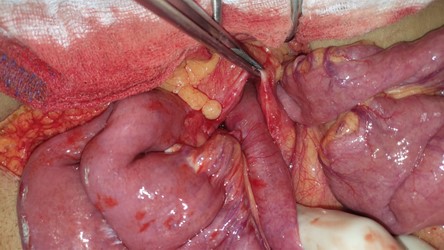
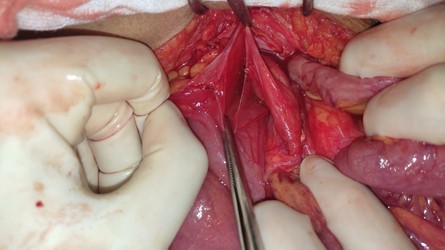
Figure 2: Intraoperative images showing the 1st jejunal loop incarcerated at the level of the left paraduodenal dimple (A); (B) and the bag after reduction of the contents (C).
The post-operative follow-up was simple with resumption of the operative transit on postoperative day 2 and then declared discharged on postoperative day 3. The patient was seen again on D15, D30 and D90 post-operatively, no longer presenting abdominal pain or nausea or vomiting.
Discussion
The rarity of internal hernia has been reported in the literature [4-6] where its rate is reported to vary between 0.2 and 0.9% of autopsies, 0.5 - 1% of all intestinal obstructions and 0.2 - 2% of all hernias [7].
The first description of an internal hernia dates back to 1742, it was a para-duodenal hernia related by Hensing [8] [9].
Internal hernias are the result of visceral protrusion through openings in the visceral peritoneum. The nature of the orifice, as well as the existence or absence of a hernia sac, divide these hernias into two different etiopathogenic groups.
Thus, the GULLINO CLASSIFICATION (1993) [10,11], commonly used in the literature, divides internal hernias into 2 categories:
- Hernias with sac: These are the real hernias. Hernias are distinguished through a normal orifice (the foramen omental) and hernias through a paranormal orifice (peritoneal dimples such as para-duodenal (right and left), ileocecal, paracolic, broad ligament of the uterus, supra-bladder, inter and meso-sigmoid) hernias
- Bagless hernias: these are internal prolapses or prolapses either through a pathological orifice formed through a meso or omentum (transmesenteric, trans-mesocolic, trans-epiploic or by colo-epiploic disinsertion) or through an abnormal orifice formed through congenital anomalies (a ligament such as the sickle ligament of the liver or a meso such as the meso of Meckel's diverticulum).
There is also the QUENU CLASSIFICATION (1967) [12] which is as used as the previous one and which divides internal hernias into 4 distinct groups.
- Hernias through an abnormal orifice: The abnormal orifice can be congenital or acquired. A distinction is made between: trans-mesenteric, trans-epiploic, trans-mesocolic hernias and hernias through the broad ligament
- Hernias through a normal orifice: these are hernias through the foramen omental in the posterior cavity of the omentums.
- Retroperitoneal hernias: These are thought to be the result of abnormalities in the rotation of the intestine during embryogenesis. A distinction is made between: para-duodenal, peri-cecal and inter-sigmoid hernias
- Unclassified hernias: The hernia opening may be iatrogenic abnormal or congenital abnormal. A distinction is made between: suprabladder hernias, internal hernias of the sickle ligament and hernias through orifices accidentally created by the surgeon during the operation.
Paraduodenal hernias alone account for about 53% of all internal hernias. Although their initial description dates back to the nineteenth century under various names, depending on whether they are right or left, they are based on mechanisms whose pathophysiology remains controversial to this day [8,20]. They are defined by the engagement of a segment of the intestine in a dimple in the duodenal area. These dimples result from a defect in the adhesion of the 2 peritoneal layers of the fascia of Treitz [21]. According to Moynihan [9], there are 9 of them, five of which can lead to intestinal incarceration: superior duodenal dimple, inferior duodenal dimple, the union of these 2 dimples forming the Treitz dimple, the retroduodenal dimple behind the pancreas and the 4th portion of the duodenum, Landzert's para-duodenal dimple and Waldeyer's dimple on the right or mesenteric-parietal dimple [22].
Left paraduodenal hernias are defined by an engagement of the intestine in the Landzert dimple. They represent about 3 quarters of all paraduodenal hernias [20,23]. According to the vascular ratios, 3 types can be described [24,25]:
- Treitz's hernia characterized by an intestinal involvement behind the vascular arch of Treitz, consisting of the inferior mesenteric vein and the left superior colonic artery.
- Estrada's retro-mesocolic hernia: this is a protrusion of the intestine through a breach in the posterior area of the vascular arch of Treitz.
- The third type is located in front of the vascular arch.
The symptomatology of internal hernias is not specific, it is that of acute or subacute intestinal obstruction: pain, vomiting, cessation of matter and gas [10,11,13]. Most often, the diagnosis is made during a laparotomy performed in the presence of an occlusive syndrome whose mechanism remained obscure before the operation [14]. In some cases, this hernia, which is perfectly asymptomatic, is discovered during an operation for another surgical condition [15,16].
The clinical examination allows other than the search for signs in favor of occlusion, must look for signs of severity of occlusions.
The ASP is the examination traditionally performed as a first-line treatment in the context of an occlusive syndrome. Its diagnostic yield is relatively low, estimated at between 50% and 60%. [88] He looked for the presence of hydro-aeric levels, a pneumoperitoneum and the distribution of dilated digestive loops when another image was taken from the front in the supine position and vertical direction radius.
In the case of left peptic hernias, the most suggestive sign is the absence of a small intestine in the pelvis. In addition, we can note the existence of a semicircular, regular line, encircling the descending colon and the sigmoid [17]. ASP may also show dilation of the spindly loops forming an ovoid mass in the left hypochondrium [18].
CT with contrast agent injection is currently the best examination for making the diagnosis with high reliability [18]. The topography of the distended loops and above all the precise analysis of the point of convergence of their mesenteric leaflets, which should suggest and locate the exact location of the "trap" and the type of internal hernia encountered [19].
Thin-section images provide the necessary information such as detailed knowledge of the anatomy, etiology and imaging landmarks of the different types of hernias, thus allowing an accurate and specific preoperative diagnosis [20].
Left paraduodenal hernias are manifested by a cluster of jejunal loops contained in a peritoneal sac located between the body or tail of the pancreas, and the stomach. A mass effect on the posterior wall of the stomach and adjacent organs may be observed. Abnormalities of the mesenteric vessels such as engorgement and stretching of the vessels contained in the sac as well as a displacement of the mesenteric axis to the left are the keys to the diagnosis. CT makes it possible to make the diagnosis with a sensitivity of 63%, a specificity of 76% and an accuracy of 77% [18].
Small bowel transit no longer seems to be an issue and abdominal ultrasound remains of no interest in the diagnosis of internal hernias [11,21].
A complete blood test should be requested to look for the general impact of occlusive syndrome and to monitor for metabolic and electrolyte disorders often associated with these obstructions, such as hypokalemia, hyponatremia, hypovolemia, and leukocytosis.
The management of an internal hernia is always surgical and urgent (in case of strangulation) to avoid necrosis of the herniated loop and peritonitis.
It must be rapid, starting with resuscitation measures and then surgical management aimed at removing the obstacle by reducing the internal hernia, treating any intestinal lesions or other viscera, restoring digestive continuity and preventing hernia recurrence [13,22]
The removal of the hernia sac can sometimes be forbidden (in the case of left paraduodenal hernias), useless, and even impossible, or even dangerous. In the case of a hernia through a paranormal orifice, the closure of the collar can be achieved by separate stitches of absorbable or non-absorbable threads, although it is a delicate procedure that can cause a vascular wound [11,23].
Therapeutic abstention with monitoring over a long period of time of these hernias shows that the progression is towards complications. It therefore seems justified to treat all diagnosed internal hernias, even if they are asymptomatic or mildly symptomatic [24].
The prognosis of internal hernias is good, even excellent, provided that the operation is early, anticipates the various complications of occlusions and that the surgeon knows how to find his bearings in the face of complex anatomical pictures and knows how to safeguard the large vessels of the hernia neck [6].
Conclusion
Internal hernia is a surgical emergency that requires early management. It is a rare cause (0.2 to 5.8%) of acute bowel obstruction.
This rarity and their non-specific presentation make the preoperative diagnosis of internal hernias very difficult.
Abdominal computed tomography with contrast agent injection, performed in an emergency, is the examination of choice to be carried out in the presence of an acute intestinal obstruction both in terms of diagnosing the mechanism of the obstruction and especially the etiological diagnosis in the preoperative period and in terms of the therapeutic indication, thus making it possible to guide the procedure and the surgical approach.
The treatment is essentially surgical, consisting of a removal of the herniated loop with the closure of the hernia orifice in order to prevent a possible recurrence when possible.
Only early diagnosis and treatment prevent complications and improve the prognosis.
References
- Singh S, Das A, Chawla AS, Arya SV, Chaggar J. A rare presentation of midgut malrotation as an acute intestinal obstruction in an adult : Two case reports and literature review. International Journal of Surgery Case Reports, 2013; 4(1): 72-75. https://doi.org/10.1016/j.ijscr.2012.10.005.
- Régent D, Ranchoup Y, M'Benge A, Phi IN, Chikhaoui N, Mathias J. Radiological imaging of internal hernias, 2015.
- Murali Appavoo Reddy UD, Dev B, Santosham R. Internal Hernias : Surgeons Dilemma-Unravelled by Imaging. Indian Journal of Surgery, 2014; 76(4): 323-328. https://doi.org/10.1007/s12262-012-0620-7.
- Collins D, Kavanagh D, Myers E, Richards S, McDermott E. Incarcerated transmesosigmoid hernia presenting in a 60-year-old man : A case report. Journal of Medical Case Reports, 2008; 2: 161. https://doi.org/10.1186/1752-1947-2-161.
- Lê P, El Braks R, Ramaheriarison Y, Billey C. A retrocecal hernia. Feuillets de Radiologie, 2008; 48(1): 35-38. https://doi.org/10.1016/S0181-9801(08)70317-8.
- Pessaux P, Tuech JJ, Derouet N, Du Plessis R, Ronceray J, Arnaud JP. Internal hernia : A rare cause of intestinal obstruction. Apropos of 14 cases. Annales De Chirurgie, 1999; 53(9): 870-873.
- Bensardi F, Elyamine O, Majd A, Abdelilah EB, Mounir B, Khalid EH, et al. Strangulated internal supravesical hernia associated with left inguinal hernia : A very rare case report of acute intestinal obstruction. Annals of Medicine and Surgery, 2021; 66: 102393. https://doi.org/10.1016/j.amsu.2021.102393.
- Allabert J, Andro JF, Chamoun S, Teniere P, Testart J. Paraduodenal hernias. Apropos of 2 cases. Annales De Chirurgie, 1984; 38(1): 50-53.
- Meyers MA. Paraduodenal hernias. Radiologic and arteriographic diagnosis. Radiology, 1970; 95(1): 29-37. https://doi.org/10.1148/95.1.29.
- Gullino D, Giordano O, Gullino E. Internal hernia of the abdomen. Apropos of 14 cases. Journal De Chirurgie, 1993; 130(4): 179-195.
- Gullino D, Giordano O, Gullino E. Internal hernias of the abdomen. Apropos of 14 cases. Journal De Chirurgie, 1993; 130(5): 260-264.
- Quénu J. Operations on the walls of the abdomen and on the digestive tract. Man, 1967.
- Kotobi H, Echaieb A, Gallot D. Surgical treatment of rare hernias. CME - Surgery, 2005; 2(4): 425-439. https://doi.org/10.1016/j.emcchi.2005.06.001.
- Bedioui H, Daghfous A, Daghfous A, Ksantini R, Nouira K, Chebbi F, et al. Internal herniation through the falciform ligament revealed by acute intestinal obstruction. Presse Medicale (Paris, France: 1983), 2008; 37(1 Pt 1): 44-47. https://doi.org/10.1016/j.lpm.2007.03.040.
- Guivarc’h M, Bex JP. Surgical pitfalls of right paraduodenal hernia. Apropos of an unusual type]. Chirurgie; Memoires De l’Academie De Chirurgie, 1973; 98(13): 788-796.
- Medarhri J, el Ounani M, Rachid K, Iken A, Echarrab M, el Amraoui M, et al. [Left internal paraduodenal hernia. Apropos of a new case]. Journal De Chirurgie, 1996; 133(9-10): 462-465.
- Maillet B, Le Treut YP, Boutboul R, Devred P, Maurin B, Bricot R. Left internal paraduodenal hernia : A case in a young adult. Annales De Gastroenterologie Et D’hepatologie, 1984; 20(6): 363-367.
- Mnif N, Salem A, Bouzaidi S, Rajhi H, Trabelsi O, Najjar T, et al. [Left paraduodenal internal hernia. A new case report]. La Tunisie Medicale, 2002; 80(3): 142-145.
- Mathias J, Phi I, Bruot O, Ganne P-A, Laurent V, Regent D. Internal hernias. EMC - Radiology and Medical Imaging - Abdominal - Digestive, 2008; 3(4): 1-8. https://doi.org/10.1016/S1879-8527(08)72830-2.
- Doishita S, Takeshita T, Uchima Y, Kawasaki M, Shimono T, Yamashita A, et al. Internal Hernias in the Era of Multidetector CT : Correlation of Imaging and Surgical Findings. RadioGraphics, 2016; 36(1): 88-106. https://doi.org/10.1148/rg.2016150113.
- Delamarre J, Henry X, Jouet-Gondry C, Daurat M, Deschepper B, Stoppa R. Cecal hernia through Winslow’s foramen. Radiographic study of a case and review of the literature]. Journal De Radiologie, 1988; 69(6-7): 459-464.
- Internal Hernias: Surgical Anatomy.
- Gargouri F, Frikha F, Amrou H, Ammous H, Abid M, Ghorbel A, et al. Internal abdominal hernias. Report of 8 cases. La Tunisie Medicale, 2001; 79(6-7): 366-369.
- Guibé JP, Kopp JP. A new variety of paraduodenal hernia. Hernia in the right mesocolon. Annales De Chirurgie, 1966; 20(11): 736-740.

