Case Study of Iliac Osteomyelitis in a Pediatric Patient, Manifesting as Septic Arthritis of the Hip
Sharath Raj1,*, Tharun Teja Aduri1, Shrinivas VB1, Vivek P Ksheerasagar1, Nitish Jagdish Jyoti2 and Vijay Goni3
1Senior Resident, Department of Orthopaedics Surgery, Post Graduate Institute of Medical Education and Research (PGIMER), India
2Senior Resident, Department of Orthopaedics, All India institute of Medical science (AIIMS), Delhi, India
3Professor and Head, Department of Orthopaedics Surgery, Post Graduate Institute of Medical Education and Research (PGIMER), India
Received Date: 12/11/2024; Published Date: 05/12/2024
*Corresponding author: Sharath Raj, Senior Resident, Department of Orthopaedics Surgery, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. Email ID: sharathraj.pgi@gmail.com
Abstract
Osteomyelitis of the pelvis is a serious bone infection that can cause localized pain, swelling, fever, and malaise. The ilium bone is the most affected due to its location and vascular supply, which can be compromised by trauma or underlying conditions. Staphylococcus aureus is the primary pathogen, often entering through skin breaks or surgical sites. Other pathogens, such as Streptococcus and Escherichia coli, may also be present. A six-year-old female patient was diagnosed with iliac osteomyelitis, accompanied by abscesses in the iliopsoas and iliacus muscles. She underwent an open joint washout procedure, followed by an MRI scan, which confirmed her diagnosis. She received additional surgical debridement and antibiotic treatment, leading to her complete recovery. Pelvic osteomyelitis may resemble hip septic arthritis, making early magnetic resonance imaging a valuable tool for accurate diagnosis. However, the prognosis is generally favourable, and long-term complications are infrequent.
Keywords: Pelvic osteomyelitis; Iliac osteomyelitis; Hip septic arthritis
Introduction
Osteomyelitis of the pelvis is a rare condition that often presents significant challenges in diagnosis. The primary etiology is typically attributed to the hematogenous dissemination of pathogens, predominantly Staphylococcus aureus, although various other microorganisms have also been recognized as potential causative agents [1,2,4]. The clinical manifestations of this disease can closely resemble a range of other medical conditions, such as acute abdominal pain, septic arthritis, typhoid fever, nephrolithiasis, osteomyelitis of the proximal femur, discitis, and neoplastic processes [1-3]. This case report emphasizes the diagnostic similarities between iliac osteomyelitis and septic arthritis of the hip.
Case Report
A six-year-old girl was referred to the Orthopaedic department due to a five-day history of right hip pain, fever, and difficulty in bearing weight. There was no reported history of trauma or recent illness. The patient, of Nepali descent, had not traveled recently and had no known infectious contacts or significant past medical history.
Upon examination, her temperature was recorded at 39.5 degrees Celsius, and the right hip was positioned in flexion, exhibiting localized tenderness at the anterior joint line. Both passive and active movements of the hip were painful and limited. The examination of the left hip, knees, and ankles yielded normal results, while mild tenderness was noted in the right iliac fossa during abdominal examination.
Laboratory tests indicated neutrophilia with a left shift, alongside elevated levels of C-Reactive Protein (CRP) and erythrocyte sedimentation rate (ESR). A sickle cell screening returned negative, and initial pelvic X-rays appeared normal. The diagnosis of hip septic arthritis was made, leading to an open washout of the hip joint, during which two millilitres of blood-stained fluid were aspirated. The patient was started on intravenous (IV) antibiotics. However, the following day, she remained febrile, and both CRP and ESR levels continued to rise. A second open washout of the right hip was conducted, but no pus or fluid was obtained.
Subsequent blood and joint fluid cultures confirmed the presence of Staphylococcus aureus. A magnetic resonance imaging (MRI) scan of the right hip revealed collections in the right iliacus and distal iliopsoas, along with abnormal marrow signal in the right iliac wing, indicative of osteomyelitis (Figure 1).
The patient was diagnosed with iliac osteomyelitis and underwent exploration of the right iliopsoas abscess was performed. This procedure uncovered a significant collection of pus and some necrotic muscle, which were thoroughly washed out and debrided.
Following the intervention, she gradually recovered and was discharged home after a total hospitalization of 30 days. Oral antibiotics were prescribed for an additional 28 days on an outpatient basis.
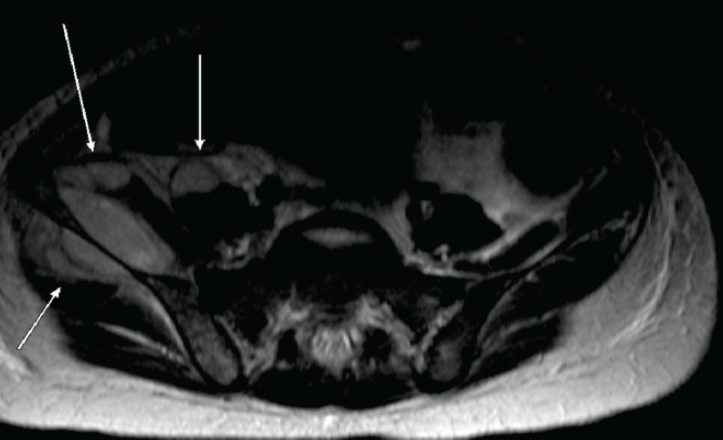
Figure 1: A T1-weighted axial MRI scan reveals fluid collections in the right iliacus and distal right iliopsoas regions, as well as a collection on the contralateral side of the iliac wing that extends into the gluteus minimus and medius muscles. Additionally, there is an abnormal signal in the marrow of the right iliac wing, indicative of osteomyelitis.
Discussion
Although it is a rare disorder, 1% to 11% of cases of haematogenous osteomyelitis are caused by pelvic osteomyelitis [5,6]. The most typical place is the ilium because its bigger size and adequate blood supply [3,5]. The typical age of onset is typically 7–14 years old, with a slight male predominance [1-3,5,7]. The most common cause organism staphylococcus aureus, found in 38% to 46% of instances, but additional pathogens such as streptococcus and salmonella gram-negative bacteria and pneumoniae [1-3,5,7].
Hip or thigh discomfort, which is present in 98% of cases, fever in 57% of cases, and reduced weight bearing in 46% of cases are clinical characteristics linked to pelvic osteomyelitis [1,2,5,7]. Furthermore, there is frequently pain upon lateral pelvic compression, reduced straight leg raising, and soreness upon probing of the sacroiliac joint. Flexion of hip may occur as a result of irritation of the iliopsoas muscle by abscess formation [8]. Hip joint passive range of motion is typically maintained, with pain limited to the joint's extremes of motion [1,6]. Tenderness in the right iliac fossa may also result from the spread of inflammation from the pelvic inner cortex [6].
Raised inflammatory markers are commonly detected by blood tests; 90% of cases have an elevated ESR, and 59% to 66% have a raised white cell count [1-3,5]. Only 50% to 78% of blood and tissue cultures turn out to be positive, and negative cultures do not rule out infection [1,3,5]. Since osteomyelitis's characteristic radiographic characteristics typically take two to three weeks to manifest, first radiographs are typically unremarkable [5,9]. Radionuclide bone scans can identify pyogenic infection early on [1,3,5], and ultrasound scans can show profound soft tissue edema in pelvic osteomyelitis [7]. By showing the location and degree of infection, as well as the existence of lytic lesions, sequestrum, or traumatic fractures, computed tomography can also aid in the early diagnosis process [2,5,10].
MRI is, however the gold standard examination and is reported as being 97% sensitive and 94% specific for the diagnosis of pelvic osteomyelitis. Early on in the course of the disease, it can show signs of soft-tissue and intra-osseous abscesses, as well as marrow oedema and hyperaemia of the infected bone [9,10]. Since the pelvis has a healthy blood supply, there is less chance of sequestrum and the ligamentous structure slows the spread of infection, IV antibiotics are typically the only treatment used for pelvic osteomyelitis [1,5,10]. Generally speaking, surgery is only recommended in cases of significant osseous involvement, non-responsiveness to antibiotic treatment, or formation of an abscess that needs to be drained [1,5,10].
With prompt treatment, the prognosis is typically good, with 95% to 97% of patients achieving a full recovery [3, 5]. However, if treatment is postponed, complications may arise, which might include growth stop, fusion of the sacroiliac joint, irregularity of the acetabulum, and the development of chronic osteomyelitis [5,9].
Conclusion
This case report underscores the challenges associated with diagnosing pelvic osteomyelitis, particularly due to its clinical resemblance to septic arthritis of the hip. The predominant clinical manifestations of pelvic osteomyelitis typically encompass pain in the hip or thigh, fever, and changes in weight-bearing capacity. Magnetic Resonance Imaging (MRI) is considered the definitive diagnostic tool, capable of identifying the condition in its early stages. Generally, antibiotic treatment is sufficient; however, in instances where abscesses develop, surgical debridement becomes necessary.
Ethical Clerance: Not Applicable.
Conflict of interest: No Conflict of interest.
References
- Highland T, Lamont R. Osteomyelitis of the Pelvis in Children. J Bone Joint Surg [Am], 1983; 65: 230-234.
- Rand N, Mosheiff R, Matan Y, Porat S, Shapiro M, Liebergall M. Osteomyelitis of the pelvis. J Bone Joint Surg [Br], 1993; 75-B: 731-733.
- Zvulonov A, Gal N, Segev Z. Actue hematogenous osteomyelitis of the pelvis in childhood: Diagnostic clues and pitfalls. Pediatric Emergency Care, 2003; 19(1): 29-31.
- Calza L, Manfredi R, Briganti E, Attard L, Chiodo F. Iliac osteomyelitis & gluteal muscle abscess caused by Streptococcus intermedius. J Med Microbiol, 2001; 50: 480-482.
- Davidson D, Letts M, Khoshhal K. Pelvic osteomyelitis in chilren: a comparison of decades from 1980-1989 with1990-2001. J Pediatric Orthopedics, 2003; 23: 514-521.
- Beaupre A, Carroll N. Three Syndromes of Iliac Osteomyelitis in children. J Bone Joint Surg [Am], 1979; 61: 1087-1092.
- Mah ET, LeQuesne GW, Gent RJ, Paterson DC. Ultrasonic signs of pelvic osteomyelitis in children. Pediatr Radiol, 1994;24: 484-387.
- Beslikas TA, Panagopoulos PK, Gigis I, Nenopoulos S, Papadimitriou NG, Christoforides JE. Chronic osteomyelitis of the pelvis in children and adolescents. Acta Orthop Belg, 2005; 71: 405-409.
- Connolly SA, Connolly LP, Drubach LA, Zurakowski D, Jaramillo D. MRI for detection of abscess in acute osteomyelitis of the pelvis in children. Am J Roentgenol, 2007; 189: 867-872.
- Viani RM, Bromberg K, Bradley JS. Obtruator internus muscle abscess in children: report of seven cases and review.Clin Infect Dis, 1999; 28: 117-122.

