Food Debris in the Bladder: Uncovering a Rare Vesicoenteric Fistula in Bladder Squamous Cell Carcinoma
Hamza AIT MAHANNA1,*, Mehdi SAFFIEDDINE1, Oussama BJANE1, Adil Kbiro2,3, Amine Moataz2,3, Mohamed DAKIR2,3, Adil DEBBAGH2,3 and Rachid ABOUTAIEB2,3
1Department of Urology, CHU Ibn Rochd, Casablanca, 20000, Morocco
2Department of Urology, University Hospital Center Ibn Rochd Casablanca, Morocco
3Faculty of Medicine and Pharmacy of Casablanca Morocco
Received Date: 10/11/2024; Published Date: 26/11/2024
*Corresponding author: Hamza AIT MAHANNA, Department of Urology, University Hospital Center Ibn Rochd Casablanca, Morocco
Abstract
Enterovesical fistulas are abnormal connections between the bladder and gastrointestinal tract, often resulting from malignancy, surgery, or inflammation. This report describes a rare vesicoenteric fistula discovered incidentally during transurethral resection of a bladder tumor (TURBT) in a 70-year-old male with hypertension, ischemic heart disease, and heavy smoking history. He presented with hematuria and lower urinary tract symptoms, requiring multiple TURBTs. During TURBT, food debris was found in the bladder, a rare clue suggesting an enterovesical fistula, later confirmed by imaging. Histopathology showed bladder squamous cell carcinoma.
The recurrent tumor and multiple procedures likely contributed to the fistula formation. Awareness of atypical symptoms like fecaluria or recurrent infections is crucial for timely diagnosis. This case underscores the importance of vigilance in patients with bladder cancer, especially squamous cell carcinoma, when unexpected findings arise.
Keywords: Bladder squamous cell carcinoma; Vesicoenteric fistula; Food debris; Urinary bladder fistula
Introduction
An Enterovesical Fistula (EVF) is an abnormal connection between the intestine and the bladder. Though rare, EVFs can lead to substantial health issues and significantly diminish the patient’s quality of life. These fistulas most often arise from advanced disease stages or result from traumatic or iatrogenic injury [1].
Enterovesical fistulas, often resulting from malignancies, trauma, or inflammatory diseases, pose diagnostic and therapeutic challenges.
Invasive bladder tumors are often linked to fistula formation, particularly following surgical procedures. This case highlights an unusual discovery of food particles in the bladder during TURBT, suggestive of a enterovesical fistula.
EVF is an uncommon complication of bladder tumors invasion, with some cases reported in the literature. Here, we present this exceptionally rare complication in Morocco.
Case Presentation
A 70-year-old male farmer, with a history of hypertension, ischemic heart disease, and active smoking (40 pack-years), presented with total hematuria and lower urinary tract symptoms that began two years ago. His symptoms included both obstructive elements, such as urinary retention, and irritative symptoms like pollakiuria and urgency. His condition had been complicated by recurrent episodes of acute urinary retention that required catheterization. Despite undergoing three transurethral resections of a bladder tumor (TURBT) within the last three months, his symptoms persisted, leading to a referral to our center for further evaluation and management. On examination, slight conjunctival, a digital rectal exam revealed a firm prostate, with signs of infiltration at the bladder base, laboratory tests revealed mild anemia, a firm prostate.
A CT scan of the abdomen and pelvis revealed a large bladder mass, measuring 91x90 mm and extending over 146.5 mm, causing bilateral ureterohydronephrosis due to obstruction. During the subsequent TURBT, a large tumor with extensive necrosis occupied the entire bladder wall (Figure 1).
Notably, food debris of tomatoes was observed within the bladder cavity, raising suspicion of a vesico-digestive fistula (Figure 2).
Further intraoperative exploration confirmed the leakage of irrigation fluid from the bladder into the rectum during rectal examination. Upon questioning, the patient reported experiencing watery diarrhea over the past three months, consistent with fecaluria.
An enteroscanner was then performed, which confirmed the presence of a vesico-digestive fistula (Figure 3).
The pathological examination of the bladder tumor resection revealed a high-grade papillary urothelial carcinoma infiltrating the stroma, with marked squamous differentiation and the presence of calcified schistosomal eggs.
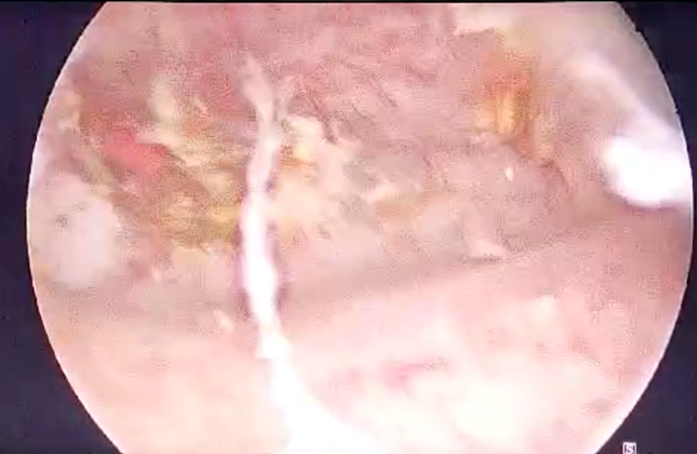
Figure 1: This endoscopic image shows the opening of the fistula in the bladder wall. Inflammatory tissues and food debris are visible, confirming the nature of the entero-vesical fistula.
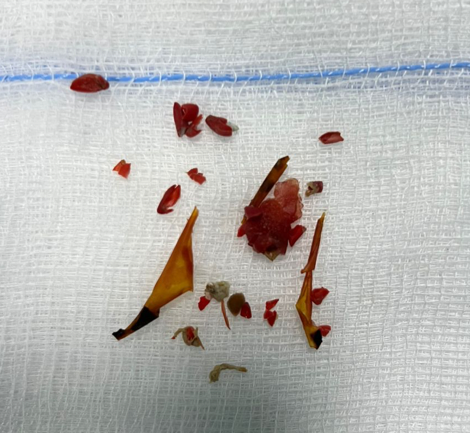
Figure 2: This image shows fragments of debris, including pieces of tomatoes, recovered during cystoscopy. These debris traverse the entero-vesical fistula, confirming the abnormal communication between the intestine and the bladder.
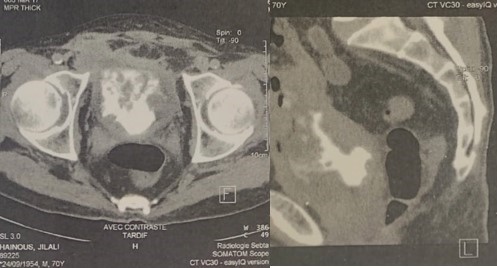
Figure 3: The CT scan images reveal an abnormal communication between the intestine and the bladder. The contrast highlights the presence of a fistula, illustrated by the passage of contrast from the intestine to the bladder.
Discussion
Vesicoenteric fistulas (VEFs) are abnormal passages between the urinary bladder and the intestine, allowing urine to leak into the intestinal lumen. These fistulas are rare, with an incidence of only 0.1%–0.2% in the general population [2].
Vesicoenteric fistulas are typically caused by bowel inflammation or malignancy, most commonly due to diverticulitis (52%), Crohn’s disease (18%), colorectal cancer (11%), or other malignant pelvic conditions (9%). Less commonly, they result from infection, trauma, radiation, or surgical injury.(3) Only a limited number of urological vesicoenteric fistula cases have been documented in the literature, mainly as isolated case reports. The highest incidence occurs between the ages of 55 and 65.
Symptoms of vesicoenteric fistulas can arise from both the urinary and gastrointestinal tracts, though patients with EVF typically present with lower urinary tract symptoms. These include pneumaturia (seen in 50–70% of cases), fecaluria (up to 51%), urinary frequency, urgency, suprapubic pain, recurrent urinary tract infections (UTIs), and hematuria. More than 75% of patients experience the characteristic symptoms of pneumaturia, fecaluria, and recurrent UTIs caused by organisms like Escherichia coli, coliform bacteria, mixed flora, or enterococci [4].
The classic symptom complex for enterovesical fistulas is known as Gouverneur’s syndrome, which includes suprapubic pain, urinary frequency, dysuria, and tenesmus.
Physical signs may include foul-smelling urine and food debris in the bladder is a rare diagnostic clue. along with occasional fever. Additionally, symptoms related to the underlying condition causing the fistula may be present; for example, patients with Crohn’s disease often experience abdominal pain, palpable masses, and abscesses [5].
Cystoscopy is considered the most sensitive test for diagnosing vesicoenteric fistulas (VEF), with an accuracy of up to 79%. However, nonspecific findings, such as localized erythema and papillary lesions, can make diagnosis challenging [6].
Previous studies have shown that the sensitivity of cystoscopy for VEF diagnosis varies widely, ranging from 6% to 90% [4].
In our experience, direct visualization of VEF during endoscopic evaluation was negative and contributed limited clinical value, however, the presence of food debris in the bladder provided an indirect indication of VEF.
Imaging is essential for confirming the diagnosis, as in this case where an enteroscanner was pivotal. Scans with oral contrast administered prior to intravenous contrast should be conducted to allow visualization of the orally ingested contrast medium within the bladder.
Beyond confirming the presence of a fistula, CT imaging offers valuable insights into both intraluminal and extraluminal pathologies that are not detected by conventional tests [7]. Due to the superior capabilities of CT scanning for diagnosis and treatment planning, plain cystography and radionuclide renography are rarely used in the assessment of enterovesical fistulae. In our case report, CT imaging successfully confirmed the diagnosis of an enterovesical fistula, whereas cystoscopy was unable to directly visualize the fistula.
A vesicoenteric fistula secondary to bladder squamous cell carcinoma was reported by Kang et al., who described the case in their study. In this instance, a fistula developed between the bladder and the intestine as a complication of advanced bladder squamous cell carcinoma, highlighting the need for careful diagnostic evaluation and management in such case [3].
In cases of malignant vesicoenteric fistulas, Whiteley Jr. and Grabstald suggested that a single-stage en bloc resection, involving removal of both the affected segment of the colon and the adjacent portion of the bladder, is a feasible and safe approach. This technique allows for the treatment of the fistula without necessitating a complete cystectomy, offering a more conservative option [8].
Conclusion
This case highlights the importance of considering Vesicoenteric fistulas in bladder cancer patients, particularly when atypical symptoms are present. Recognizing key diagnostic clues, such as food debris in the bladder, can lead to prompt diagnosis and timely intervention, improving patient outcomes.
Author Contributions
I, AIT MAHANNA Hamza, take responsibility for the integrity of the entire case report and am designated as the guarantor of the manuscript. All authors have made substantial contributions to the conception and design of the case report, the collection or interpretation of data, as well as to the drafting or critical revision of the manuscript, and have approved the final version for publication.
Competing Interests: The author has no competing interests to declare.
Grant Information: The author(s) received no specific funding for this work.
Acknowledgements: The authors have no acknowledgments to declare.
References
- Golabek T, Szymanska A, Szopinski T, Bukowczan J, Furmanek M, Powroznik J, et al. Enterovesical Fistulae: Aetiology, Imaging, and Management. Gastroenterol Res Pract, 2013; 2013: 617967.
- Bouassida M, Mighri MM, Trigui K, Chtourou MF, Sassi S, Feidi B, et al. Meckel’s diverticulum: an exceptional cause of vesicoenteric fistula: case report and literature review. Pan Afr Med J, 2013; 15: 9.
- Kang YJ, Park DJ, Kim S, Kim SW, Lee KS, Choi NG, et al. Vesicoenteric Fistula due to Bladder Squamous Cell Carcinoma. Korean J Urol, 2014; 55(7): 496.
- Stroie FA, Hasan OM, Houlihan MD, McArdle BJ, Hollowell CMP, Blumetti J, et al. Low diagnostic sensitivity of cystoscopy and cystography of surgically confirmed vesicoenteric fistulae. Int Urol Nephrol, 2020; 52(7): 1203–1208.
- Pontari MA, McMillen MA, Garvey RH, Ballantyne GH. Diagnosis and treatment of enterovesical fistulae. Am Surg, 1992; 58(4): 258–263.
- Daniels IR, Bekdash B, Scott HJ, Marks CG, Donaldson DR. Diagnostic lessons learnt from a series of enterovesical fistulae. Colorectal Disease - Wiley Online Library, 2002.
- Jarrett TW, Vaughan ED. Accuracy of Computerized Tomography in the Diagnosis of Colovesical Fistula Secondary to Diverticular Disease. J Urol, 1995.
- Whiteley HW, Grabstald H. Conservative management of distal large bowel cancer invading the urinary bladder. Clin Bull, 1975; 5(3): 99–101.

