Lumbosacral Radiculoplexus Neuropathy Following Herpes Zoster Infection
Joanna Faughender, Jeremy I Simon, Jeffrey Gehret and Philip J Koehler III*
Department of Physical Medicine and Rehabilitation, Rothman Orthopaedic Institute, Philadelphia, PA
Received Date: 23/09/2024; Published Date: 04/11/2024
*Corresponding author: Philip J. Koehler III, DO, MS, FAAPMR, DABPM, Department of Physical Medicine and Rehabilitation, Rothman Orthopaedic Institute, 825 Old Lancaster Rd, Ste 100, Bryn Mawr, Philadelphia, PA
Abstract
Diabetic lumbosacral radiculoplexus neuropathy or Bruns-Garland Syndrome is a subacute, often painful, asymmetric lower extremity neuropathy. It is attributed to an autoimmune attack resulting in ischemia to the lumbosacral roots, plexus, and/or peripheral nerves, leading to weakness and subsequent atrophy of the lower limb musculature. Diabetes, obesity, and autoimmune disorders are all risk factors for the development of this disorder, but it can also occur in patients without diabetes. The diagnosis of DLRPN can be made on a clinical basis but is best supported by electrodiagnostic evaluation to exclude other conditions. Most patients will recover but may experience a delayed and incomplete recovery. It is important to consider this condition whenever evaluating a patient with weakness of the hip girdle or lower extremity in the setting of altered immunity superimposed on metabolic dysfunction. In this case, we present a patient with a past medical history of non-insulin dependent diabetes mellitus presenting with subacute, painless, weakness of the right hip girdle and lower extremity that began one month after herpes zoster infection.
Keywords: Diabetic amyotrophy; Bruns-Garland Syndrome; Herpes Zoster; Shingles; Case Report
Introduction
Diabetic Lumbosacral Radiculoplexus Neuropathy (DLRPN) is a condition attributed to an autoimmune attack resulting in ischemia to lumbosacral roots, plexus, and/or lower limb nerves [1,2]. It is described in middle age to older type II diabetic patients and presents typically as unilateral pain in the hip girdle and thigh with unexplained weight loss and atrophy of lower extremity musculature. Symptoms can occur bilaterally and occasionally affect the upper extremity or truncal nerves [3,4]. Pain is typically the most notable and earliest symptom but severe weakness and atrophy in the proximal or even distal lower limb musculature becomes the most prominent symptoms. Sensory and autonomic symptoms are also reported [4]. This condition may also occur in patients without diabetes and presents with similar symptoms, but is not as well described as DLRPN [5]. Occasionally diabetics with DLRPN may develop weakness and atrophy from this condition without any pain [6]. Risk factors for developing this condition include diabetes, autoimmune disorders and obesity with altered immunity and metabolic dysfunction being significant contributors [3].
Case Report
An 86-year-old male presented to our electrodiagnostic laboratory complaining of four months of weakness in the right lower extremity that began within one month after developing herpes zoster in a right lower thoracic dermatomal pattern diagnosed by his primary care physician. Bloodwork ordered at that time showed an elevated blood urea nitrogen and creatinine (55mg/dL/3.0mg/dL) and blood glucose (336mg/dL). Past medical history was significant for a right total hip arthroplasty and no insulin dependent diabetes mellitus. He described numbness in the anterior right thigh and significant hip flexor weakness as well as chronic low back pain. He followed up with his orthopaedic hip surgeon who found the hip replacement to be in good position and an MRI of the lumbar spine was ordered for suspected lumbar radiculopathy. The surgeon sent the patient to us for an electrodiagnostic evaluation. His lumbar MRI did not reveal significant neural compression, disc herniation or spinal stenosis.
A thorough physical examination revealed a slightly forward flexed gait with difficulty with hip flexion. Strength in the lower extremities was 5/5 in the bilateral tibialis anterior, gastrocsoleus, and extensor hallucis. Strength in the right hip flexor and adductor was 3/5. Sensation was diminished to light touch in a stocking glove distribution in bilateral legs and the anterior right thigh. Reflexes were 2+ in the left patella and absent in the right patella and ankles.
We mutually decided with the patient to move forward the planned electrodiagnostic study and confirmed skin temperature at 30 degrees Celsius with an infrared thermometer. Nerve conduction studies demonstrated diffuse axonal sensory and motor neuropathy. Needle electromyography demonstrated axonal lumbosacral plexopathy (Figure 1).
The patient was told to follow up with his primary care doctor to monitor his blood sugar. We provided him a prescription for physical therapy and informed him that he may have permanent strength deficits. The patient followed up 4 weeks following the electrodiagnostic study and reported improvement with physical therapy. His right hip flexor strength was improved to 4/5 strength and right hip adductor unchanged at 3/5 strength. Light touch sensation was unchanged. He was recommended alpha lipoic acid and to continue therapy with additional follow up in 2 months.
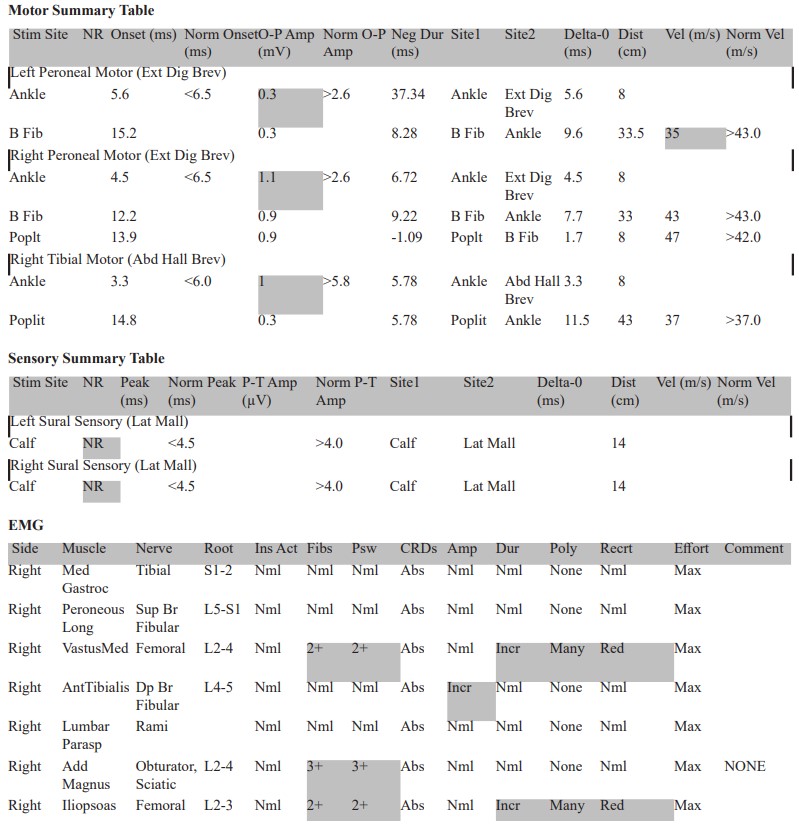
Figure 1: Electrodiagnostic study demonstrating diffuse axonal sensory and motor neuropathy on nerve conduction studies. Needle electromyography demonstrating axonal lumbosacral plexopathy.
Discussion
The diagnosis of DLRPN can be made on a clinical basis but is supported by electrodiagnostic evaluation. EMG/NCS can help exclude other conditions such as radiculopathy, myopathy or other types of neuropathies. As stated previously, the exact mechanism of DLRPN is not fully known but is thought to be attributed to an autoimmune process, as likely occurred in our patient. Prior to the onset of shingles, our patient was frequently in a hyperglycemic state which may have interplayed with the alteration in immunity that occurred because of herpes zoster infection. Although considered a monophasic illness with improvement occurring in almost all patients, recovery can be delayed and incomplete for most patients [5]. Increased morbidity and disability are often present due to the severity of disease, profound weakness, and gait disturbance. Patients are often unable to work or perform activities of daily living due to severe pain and can often require hospitalization for adequate pain control. Patients should be counseled in severe cases that recovery may be incomplete. Modalities such as antidepressant medications, physical therapy, appropriate bracing, and assistive devices should be considered to help maximize function, improve safety, and improve quality of life.
Consent: Patient written consent was obtained prior to submission
Funding: No funding source or acknowledgments
References:
- Barohn RJ, Sahenk Z, Warmolts JR, Mendell JR. The Bruns-Garland syndrome (diabetic amyotrophy). Revisited 100 years later. Arch Neurol, 1991; 48(11): 1130-1135. doi: 10.1001/archneur.1991.00530230038018.
- Raff MC, Asbury AK. Ischemic mononeuropathy and mononeuropathy multiplex in diabetes mellitus. N Engl J Med, 1968; 279(1): 17-21. doi: 10.1056/NEJM196807042790104.
- Pinto MV, Ng PS, Howe BM, et al. Lumbosacral Radiculoplexus Neuropathy: Neurologic Outcomes and Survival in a Population-Based Study. Neurology, 2021; 96(16): e2098-e2108. doi: 10.1212/WNL.0000000000011799.
- Dyck PJ, Engelstad J, Norell J. Microvasculitis in non-diabetic lumbosacral radiculoplexus neuropathy (LSRPN): similarity to the diabetic variety (DLSRPN). J Neuropathol Exp Neurol, 2000; 59(6): 525-538. doi: 10.1093/jnen/59.6.525.
- Dyck PJ, Windebank AJ. Diabetic and nondiabetic lumbosacral radiculoplexus neuropathies: new insights into pathophysiology and treatment. Muscle Nerve, 2002; 25(4): 477-491. doi: 10.1002/mus.10080.
- Garces-Sanchez M, Laughlin RS, Dyck PJ, Engelstad JK, Norell JE. Painless diabetic motor neuropathy: a variant of diabetic lumbosacral radiculoplexus Neuropathy? Ann Neurol, 2011; 69(6): 1043-1054. doi: 10.1002/ana.22334.

