Effective Management of Chronic Lower-Extremity Ulcers (CLEU) by Fu’s Subcutaneous Needling (FSN)
Jidong Wu1,2,3, Jianfeng Zheng4, Yingming Wu5, Yuzhong Liu6, Guozheng Wang2,7* and Zhonghua Fu8,*
1Fu‘s Subcutaneous Needling Association of Europe, Cambridge, UK
2Association of Traditional Chinese Medicine and Acupuncture (ATCM), London, UK
3 Cambridge Acupuncture Clinic, 452 Milton Road, Cambridge, CB4 1ST, UK
4FSN clinic, 17 Yingbing East Road, Nanyan Town, Yiyang County, Jiangxi Provence, China
5 ChangChang Village Clinic, Jiazizhen, Qiongshan District, Hainan Province, China
6Liu Yuzhong Clinic, Yaozhuang, Xinxing Town, Gangu County, Tianshui, Gansu Provence, China
7CIMI, The University of Liverpool, Liverpool, UK
8The Institute of Fu's Subcutaneous Needling, Beijing University of Chinese Medicine, Chaoyang District, Beijing 100029, China.
#These authors contributed to this paper equally
Received Date: 16/02/2024; Published Date: 01/11/2024
*Corresponding author:
Dr. Zhonghua Fu, MD, Ph.D. The Institute of Fu's Subcutaneous Needling, Beijing University of Chinese Medicine, No. 11 Beisanhuan East Road, Chaoyang District, Beijing 100029, China
Dr. Guozheng Wang, MD, Ph.D. CIMI, The University of Liverpool, Liverpool, L69 7BE, UK
Abstract
Chronic Lower-Extremity Ulcers (CLEU) are very common in the elderly population, such as chronic Venous Leg Ulcer (VLU), and in uncontrolled diabetes, such as Diabetic Foot Ulcer (DFU). Since there is no specific therapy, the ulcer normally takes a long time to heal, and in some cases the ulcer never heals. This significantly affects quality of life of large population, estimated 1% of the adult population and 3.6% of people older than 65 years. Here we report Fu’s Subcutaneous Needling (FSN) as a novel intervention in management of 6 cases of CLEU, 3 cases caused by trauma (one was due to surgery), 2 cases caused by uncontrolled diabetes and one case related to vasculitis. Complete healing was achieved after first FSN treatment in 4 cases with no recurrence. However, one case with vasculitis had lower leg ulcer healed, but new ulcer appeared in adjacent area, which is still under FSN treatment. One case after cardiac surgery had heart failure and developed severe leg oedema that stopped FSN therapy. FSN is a newly invented technique which is different from traditional acupuncture in both tools and methods as well as principles. FSN uses a special trocar acupuncture needle which is inserted underneath the skin to stretch the subcutaneous layer using a sweeping movement. FSN relaxes skeletal muscle tension to improve both arterial and venous flow. In this way, FSN targets the fundamental pathogenic mechanism of chronic VLUs and diabetic neuropathy and vasculopathy, thereby effectively improve the healing processes and quality of life, particularly maintain the ulcer surface clean and dry without odor in all the reported cases. However, further case-control and mechanistic studies are required to consolidate therapeutic efficacy and demonstrate proposed biological mechanisms.
Keywords: Chronic lower-extremity ulcers (CLEU); Chronic venous leg ulcer (VLU); Diabetic foot ulcer (DFU); Fu’s Subcutaneous Needling (FSN); Sensors for FSN; Autonomic nervous system; Muscle tone relaxation
Introduction
Chronic Lower-Extremity Ulcers (CLEU) is difficult to heal and a common lesion that significantly affects life quality [1,2]. CLEU is defined as a skin ulcer below the level of knee over 6 weeks without hope to heal in a short period [3] and affects about 1% of the adults but up to 3.6% in > 65 years old population [3]. Vascular diseases, neuropathy, particularly in uncontrolled diabetes, are the common causes with metabolic disorders, haematological disorders, and infective diseases as fewer common causes [3].
Chronic venous leg ulcers (VLU) are the most common types of CLEU. As a chronic condition in elderly people, VLU resolves very slowly and may not be completely healed after 12 months [4,5]. VLU can be extremely painful and malodorous, require constant attention, and are highly disruptive to the patients’ lives [6]. VLU affects 0.6–3% of the elderly population (> 60), increasing to 5% in the geriatric population (>80), with morbidity ranging from 1.9% to 13.1%. The UK alone has >200,000 cases, which cost about 1 billion annually in care and treatment costs [7].
In patients with uncontrolled diabetes, the low legs and feet are often affected and develop ulcers due to diabetic neuropathy and peripheral vascular disease [8,9]. The skin is easy to get damaged and infection, but difficult to heal due to poor blood circulation so has high risk for developing ulcers or gangrene (dry death of tissue due to ischemia) [10]. The lifetime risk of foot ulcer is 19% to 34%, rising with disease progressing [11]. Lifetime lower-extremity amputation incidence is around 20%, and 5-year mortality is about 50–70% [11]. Over 1 million people with diabetes suffer limb loss annually and 80% of diabetes-related lower extremity amputations are preceded by foot ulcer [12]. Diabetic foot ulcer (DFU) becomes a major part of CLEU.
The diagnosis of CLEU is relatively easy, but treatment is very difficult and mainly relies on personal care [13-15]. Therefore, many guidelines for better management have been proposed [12,16,17] and many therapies have been developed, including cleaning and disinfecting the wound with antibiotics to prevent bacterial infection and reduce pain, compressing legs using bandages or stockings to improve the blood flow [18] as well as artery stent to increase blood flow and skin transplantation [19] to accelerate healing process. If the underlying cause of the ulcer is clear, such as immobility, obesity, previous deep vein thrombosis, varicose veins, uncontrolled diabetes, etc. elimination of these causes is essential to prevent recurrence [20]. In China, traditional herbal medicine has been used as an alternative treatment, but acupuncture is rarely reported in CLEU management.
Fu’s Subcutaneous Needling (FSN) is a newly developed form of acupuncture. Traditional acupuncture requires specific needling sensations by the patients and acupuncturists, called de- qi in Chinese, but this is not required by FSN [21]. FSN focuses on muscle tone to release high tension for pain relief [22,23], and is also effective in treating many other conditions caused by high muscle (both skeletal and smooth muscles) tension [21]. Since it is a novel therapy for CLEU, only a few cases tried FSN. Here we report 6 cases of CLEU that has been successfully treated by FSN.
Materials and Methods
Typical FSN treatment: FSN uses a modified trocar acupuncture needle, including 3 parts: soft plastic tube, protecting plastic sheath, and stainless-steel needle core. The FSN needle is 1.08 mm in diameter, which is 4–5 times thicker compared to the traditional acupuncture needle [22]. During the treatment, the acupuncturists need to find the adjacent muscles with abnormal high tension and select the points on top of the muscle or surrounding area for needle insertion [21]. The needle is horizontally inserted into subcutaneous layer avoiding contact with muscle [21]. A typical FSN manoeuvre combines sweeping the needle and exerting resistance to targeted muscle movement, termed “reperfusion approach” aiming to increase local blood supply. The soft plastic tube can be retained without needle for 2 to 24 hours as an option.
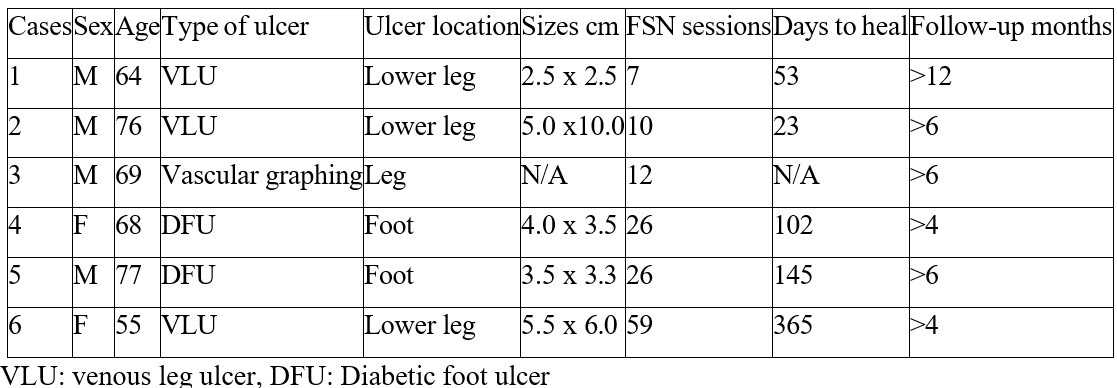
Clinical data collection and follow-up: Clinical data are from acupuncturists / authors who directly treated the patients. Table 1 presents the summary of all 6 cases. Photos were taken at each visit by acupuncturists and typical ones were presented. All cases were followed up for at least 4 months after the completion of FSN treatment courses.
Table 1: Summary of 6 cases of CLEU.
Results
Case 1: A 64-year-old Caucasian, male, came to acupuncture clinic for his chronic VLU in November 2019. The ulcer was caused by an accidental damage of left shin in July 2019. When the skin broke down it revealed a non-infected wound about 1cm deep and 2.5 cm diameter at the first consultation with his GP in early September. The ulcer was irrigated with saline and dressed with a Sorbsan ribbon with Kliniderm to cover and redressed twice a week. The patient has no history of diabetes but suffered from asthma since childhood and high dose steroid treatment led to acquired Addison’s disease.
On first examination at the acupuncture clinic, the ulcer area (2.5cm in diameter) was covered in a moist yellowish substance that represented the Flaminal Forte dressing while at its margins a reddish coloured zone of re-epithelisation was present (Figure 1A). FSN needle was horizontally inserted beneath the skin in the tibialis anterior and horizontal sweeping movement were performed for 1-2min. Concurrently, the patient moved his leg to cause contraction and relaxation of large muscles, mainly gastrocnemius, soleus and tibialis. This procedure was repeated once after 30min. The solid steel needle was removed with the cannula detained and removed after 24h. The ulcer started to visibly heal immediately after the first treatment (Figure 1B). At 7th session (53 days after the first FSN treatment), the ulcer was almost completely healed (Figure 1C). The 9-months follow up in September 2020 (Figure 1D) showed the formation of smooth scar tissue covering the lesion and consent form for publication was signed by the patient.

Figure 1: Case 1. (A) Initial visit, a 2.5 cm x 2.5 cm ulcer with yellow ointment due, in part, to Flaminal Forte dressing. (B) 7 days after first FSN treatment. The ulcer surface became dry and fresh granulated tissue grew. (C) 53 days from first visit after 7th FSN treatment. The ulcer was almost sealed. (D) Follow up for 6 months, white scar tissue formed. No recurrence so far.
Case 2: A 76-year-old Chinese, male, suffered from right lower leg ulcer for two months after a suspected insect bite. At the beginning, the skin of right lower leg was itching, swollen and painful on movement. Two days later, a 1.5x1.5 cm2 area developed ulcer. Routine treatments showed no improvement, and the ulcer became deeper and larger with malodourous exudates. Right leg pain became severe, and the patient had difficulty in straightening the leg during walking. The patient had no history of diabetes or other chronic diseases.
He came to the acupuncture clinic for pain relief on 17th July, 2020. The ulcer was irregular (maximum 10cm x 5cm) with visible necrotic tissue on the surface of the ulcer (Figure 2A). On examination there was extremely high muscle tension of right triceps surae, gluteus medius, iliopsoas and rectus abdominis. The first FSN treatment at multiple insertion points relaxed all these muscles and relieve the pain so his right leg could straighten immediately after the treatment. At the second visit, 2 days later he could walk normally and the exudate from ulcer had significantly reduced. Five dates after first visit the surface of the ulcer became dry and cleaner. On day15 after first visit, the area of ulcer became smaller (Figure 2B) and on day 23, the ulcer was largely healed (Figure 2C). The first follow-up 6 weeks after first visit, the ulcer completely healed and white scar formed (Figure 2D). Second follow up after 6 months found no recurrence.

Figure 2: Case 2. (A) The appearance of lower left leg large irregular ulcer (maximum 10cm x 5cm) with dead tissues taken during the initial visit to the acupuncture clinic. (B) 15 days after first FSN treatment, the ulcer became dry and smaller. (C) 23 days after first FSN, the ulcer largely healed. (D) Follow up at 6 weeks after first FSN treatment showed complete heal and white scar tissue formed. No recurrence so far.
Case 3: A 69-year-old Chinese, male, had type II diabetes and Grave’s disease apart from coronary condition. He underwent coronary artery bypass on 28th March 2022. After operation, the wound on median side of left leg where blood vessel was taken for graft became inflamed and irritant. The patient complaint several pain on the left leg which made him unable to rest and sleep. On examination on 19th April 2022, patient appeared with a distressed complexion, unable to walk because of left lower leg pain with intensive swelling (Figure 3A). FSN was performed on left thigh, above rectus femoris area, gentle manipulation and exercise and move movement were performed to reduce the pain. After 3 sessions, the pain was reduced, and sleep was greatly improved too. In June 2022, the lower leg ulcers became major problem (Figure 3B). Then 12 sessions of FSN acupuncture were performed to assist wound healing. On 1st September 2022, about 70% of the ulcer areas were healed (Figure 3C) and FSN was stopped.
On 25th October 2022 follow-up, local area was dry and close to complete healing (Figure 3D), which does not affect daily activity anymore.

Figure 3: Case 3. (A) First visit to FSN clinic due to severe left leg pain after coronary artery bypass grafting. The wound was covered by dressing. (B) Two months late after first visit, the ulcer developed and became the major problem. (C) Four and half months after first visit, about 70% of the ulcer areas were healed. (D) On the follow-up at 6 months after first visit, local areas were dry and did not affect daily activity anymore.
Case 4: A 68-year-old Chinese, female, came to visit on 26th April 2019 due to an ulcer above the fifth metatarsophalangeal joint on the right dorsum with severe pain for more than two months. Two months ago, the skin at the base of the fifth toe on the dorsum of the right foot became itchy, redness, swelling and painful, and then soon evolved into ulcers. With more than 40 days of treatment after diagnosed as diabetic foot in the local hospital, the ulcer was enlarged with intensified pain and coldness of the entire right lower extremity. Amputation of the affected limb was eventually suggested by doctors. The patient refused the suggestion and came to try FSN treatment. Physical examination: an elderly woman had a 4 cm × 3.5 cm oval ulcer surface with a depth of about 1.5 cm located on the fifth metatarsophalangeal joint on the lateral dorsal side of the right foot (Figure 4A). The ulcer was covered with dark brown dirt secrets with an extensor tendon exposed. The surrounding skin was dark red and swollen. She had hypertension for more than 10 years and was diagnosed diabetes mellitus 8 years ago with insulin injection to control blood sugar in the past years, but blood sugar levels were fluctuated. Diabetic foot was diagnosed and FSN was used to reduce the high muscle tension in pectoralis major, rectus abdominis, right adductors, quadriceps, hamstrings, tibialis anterior, gastrocnemius. The ulcer was also cleaned and covered with sterile dressing. After the 3rd treatment on 28th April, the coldness of the right lower extremity was significantly improved and the pain around the wound was relieved (Figure 4B). At 7th visit on 18th May 2019, the ulcer surface was dry and clean and surrounding skin became red (Figure 4C). At the 15th visit on 25th June, the skin colour around the ulcer became normal. At the 26th visit on 6th August, the ulcer was almost healed, and she could walk normally (Figure 4D). Follow up for over 4 months (Figure 4E), no recurrence occurs so far.

Figure 4. Case 4. (A) First visit showed a 4cm×3.5cm oval ulcer surface with a depth of about 1.5 cm located on the fifth metatarsophalangeal joint on the lateral dorsal side of the right foot. The ulcer was also cleaned and covered with sterile dressing. (B) At 3rd visit, 2 days late the coldness of the right lower extremity was significantly improved and the pain around the wound was relieved. The ulcer surface became dryer and surrounding skin became less swollen. (C) At 7th visit (22 days after first visit) the ulcer surface was dry and clean and surrounding skin became red. (D) At 26th visit (102 days after first visit), the ulcer was almost healed, and the patient could walk normally. (E) Follow up for over 4 months, and no recurrence occurs so far.
Case 5: A 77-year-old Chinese, male, came to visit on 24th November 2021 due to an ulcer on the lateral ankle of the right foot for more than 2 months. After treatment in local hospitals, the ulcer continued to expand, and the pain was aggravated. Physical examination found a 3.5 cm × 3.3 cm ulcerated surface on the right lateral malleolus, about 0.8 cm deep, covered with yellow-black secretions (Figure 5A). Obvious oedema was found on right lower extremity. He had hypertension for 16 years, and diabetes for 9 years. Diabetic foot was diagnosed and FSN was used to relax pectoralis major, rectus abdominis, oblique, femoral adductors, gastrocnemius, peroneus longus, and soleus. The ulcer surface was cleaned, and a sterile dressing was applied. On 30th November 2021, at the third visit, the oedema of the right lower extremity was significantly reduced (Figure 5B). The purulent secretions on the wound surface were reduced too. At 15th visit on 28th December 2021, the oedema completely subsided, the ulcer became dry and fresh granulation tissue grew (Figure 5C). At 26th visit on 25th March 2022, the ulcer was completely healed (Figure 5D). After 6 months follow-up, the condition was stable (Figure 5E).

Figure 5: Case 5. (A) At the first visit, a 3.5cm × 3.3cm ulcerated surface on the right lateral malleolus, about 0.8 cm deep, covered with yellow-black secretions and surrounding oedema. (B) At 3rd visit (3 days after first visit), the oedema of the right lower extremity was significantly reduced. The purulent secretions on the wound surface were reduced. (C) At 15th visit (31 days after first visit), the oedema completely subsided, the ulcer became dry and fresh granulation tissue grew. (D) At 26th visit (145 days after first visit), the ulcer was completely healed. (E) After 6 months follow-up, the condition was stable.
Case 6: A 55-year-old Chinese, female, came a FSN clinic on 28th December 2020 due to vasculitis with right lower leg chronic ulcer for 6 years and worsen after trying many different therapies, including artery stent and herbal medicines. The local skin was dark brown colour and hard like leather with a dressed ulcer, 5.5 x 6.0cm (Figure 6A). The patient was in great pain and FSN was used immediately to relieve the pain. On her 2nd visit next day, the exudates on the surface of ulcer were obviously reduced (Figure 6B). On her 11th visit one month late, the skin colour was improved significantly, and new tissues grew in the ulcer (Figure 6C). On her 33th visit (4 months after first visit), the original ulcer was dry and became smaller, but a new injury occurred at adjacent area (Figure 6D). On 59th visit, exactly one year after her 1st visit, the old ulcer was fully sealed, but new injury developed ulcer (Figure 6E). The new ulcer is still under treatment.

Figure 6: Case 6. (A) At the first visit, a 5.5 cm x 6.0 cm ulcer was covered with dressing and surrounding skin became dark brown colour and hard like leather. (B) At 2nd visit next day, the exudates on the surface of ulcer were obviously reduced. (C) At 11th visit (30 days after first visit), the skin colour was improved significantly, and fresh granulated tissues grew in the ulcer. (D) At 33th visit (120 days after first visit), the original ulcer was dry and sealed but a new injury occurred at adjacent area. (E) At 59th visit, exactly one year after her 1st visit, the old ulcer was fully sealed, but new injury developed ulcer. Up-to-date the new ulcer is still under treatment.
Discussion
FSN has been established for over 27 years and mainly focuses on the human anatomy and physiology, concentrating on muscle tone and tension, rather than meridians and acupoints [21,24]. Recently we reported 2 cases of diabetic foot ulcers managed by FSN [25]. In this work, we reported 6 cases of chronic lower-extremity ulcers treated with FSN. The first 3 cases developed ulcers due to local injury and received general treatments in local hospital for over 6 weeks. Cases 4 and case 5 suffered from diabetes for many years and developed foot ulcers, whilst case 6 suffered from vasculitis and developed lower leg ulcer for 6 years. All the cases had obvious increased muscle tension in the affected leg companied with severe pain. The immediate responses to FSN treatment were significantly reduced muscle tension and pain relief. Then the exudates on the surfaces of ulcers were significantly reduced and become dry and less smelly. These changes significantly improved the quality of life soon after FSN treatment. Most of cases gave up the dressing which was used every day before FSN treatment to facilitate their daily activity. Since those cases had long history of ulcers, it is believed that FSN treatment accelerated the ulcer healing processes. However, it is too early to make a conclusion without case-control studies.
VLUs are the common types of CLEU and their pathophysiology is not fully understood so far. A few theories have been proposed, including venous hypertension, fibrin cuffs around capillary beds leading to elevated intravascular pressure and decreases in the diffusion of oxygen and other nutrients, additionally inflammatory cells and pro-inflammatory cytokines trapped in fibrin cuff enhance local inflammation etc [26,27]. Overall, the circulatory insufficiency, including arterial, venous and microcirculatory insufficiency, could be the major factor that delays and prevents the healing of the ulcers [28].
Diabetic foot ulcers are common complications of patients suffered from uncontrolled diabetes mellitus due to underlying neuropathy, peripheral vascular disease, or poor foot care [29]. The ulcers are usually in the areas of the foot which encounters repetitive trauma and pressure sensations but less blood supply, so called diabetic foot ulcer which developed in about 5% of patients with diabetes mellitus and about 1% end up with an amputation [30]. The ulcers are of chronic courses and difficulty to heal, thereby require intensive supports from different specialists.
The common factor of both VLUs and diabetic foot ulcers is the deficiency of local blood supply. FSN relaxes skeletal muscle with high tension and improves both arterial and venous sufficiency in their lower legs as well as pain relief (Figure 6). This may be due to arteries that supply blood to skin and deep veins that return blood to heart all travel through or by skeletal muscles. It has been noted that exudate from the ulcers was dramatically reduced and the surrounding skin showed increased perfusion even after first session of FSN treatment, indicating improved local blood circulation, the key factor for ulcer healing. However, other mechanisms, such as an anti-inflammation, may be also involved. Further investigation to demonstrate the underlying pathological mechanisms of CLEU and FSN treatment is required.
The limitation of this report is the lack of control group and experimental evidence. Case control and mechanistic studies will be performed in future. However, this report is sufficient to draw attention to FSN treatment during the management of CLEU and initiate the exploration of the underlying pathophysiology.
Conclusion
This case report has demonstrated the obvious benefits from FSN treatment during the management of CLEU, including muscle relaxation, pain relief, and exudate reduction. Whether the ulcer healing speed has been really accelerated by FSN still needs further evidence from future case-control studies.
Acknowledgments: Thanks to the patients and doctors who are involved in data collection.
Author Contributions: Conceptualization Z.H.F., G.Z.W. and J.D.W.; Methodology, Z.F.F.; Validation, Z.H.F. and G.Z.W.; Investigation, J.D.W., J.F.Z., Y.M.W. and Y.Z.L.; Data Curation, Z.H.F., G.Z.W. and J.D.W.; Writing – Original Draft Preparation, G.Z.W; Writing – Review & Editing, Z.H.F., G.Z.W. and J.D.W.; Project Administration, Z.H.F.
Statement on Funding: No funding for this report
Conflicts of Interest: The authors declare no conflicts of interests.
Institutional Review Board Statement: Ethical review and approval were waived for this study, due to post-respective reports of cases from individual clinics.
Informed Consent Statement: Informed consents were obtained from all patients involved in the study.
References:
- Singer AJ, Tassiopoulos A, Kirsner RS. Evaluation and Management of Lower- Extremity Ulcers. N Engl J Med, 2017; 377: 1559-1567. doi: 10.1056/NEJMra1615243.
- van Acker K, Leger P, Hartemann A, Chawla A, Siddiqui MK. Burden of diabetic foot disorders, guidelines for management and disparities in implementation in Europe: a systematic literature review. Diabetes Metab Res Rev, 2014; 30: 635-645. doi:10.1002/dmrr.2523.
- Agale Chronic Leg Ulcers: Epidemiology, Aetiopathogenesis, and Management. Ulcers, 2013; 2013: 413604. doi:10.1155/2013/413604.
- Heatley F, Saghdaoui LB, Salim S, Onida S, Davies AH. Primary care survey of venous leg ulceration management and referral pre-EVRA trial. Br J Community Nurs, 2020; 25: S6-S10. doi: 10.12968/bjcn.2020.25.Sup12.S6.
- Adderley UJ, Thompson C. Community nurses' judgement for the management of venous leg ulceration: a judgement analysis. Int J Nurs Stud, 2015; 52: 345-354. doi:10.1016/j.ijnurstu.2014.09.004.
- Heatley F, Saghdaoui LB, Salim S, Onida S, Gohel MS, Davies AH. UK primary care survey of venous leg ulceration management and referral - Post-EVRA trial. Phlebology, 2021; 36: 48-53. doi: 10.1177/0268355520944102.
- Guest JF, Fuller GW, Vowden Venous leg ulcer management in clinical practice in the UK: costs and outcomes. Int Wound J, 2018; 15: 29-37. doi:10.1111/iwj.12814.
- Grennan Diabetic Foot Ulcers. JAMA, 2019; 321: 114. doi:10.1001/jama.2018.18323.
- Slomski Intensive Glycemic Treatment Reduces Diabetic Foot Ulcers. JAMA, 2022; 327: 1118. doi: 10.1001/jama.2022.3754.
- Aumiller WD, Dollahite Pathogenesis and management of diabetic foot ulcers. JAAPA, 2015; 28: 28-34. doi: 10.1097/01.JAA.0000464276.44117.b1.
- McDermott K, Fang M, Boulton AJM, Selvin E, Hicks CW. Etiology, Epidemiology, and Disparities in the Burden of Diabetic Foot Ulcers. Diabetes Care, 2023; 46: 209-221. doi:10.2337/dci22-0043.
- Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot Lancet, 2005; 366: 1719-1724. doi:10.1016/S01406736(05)67698-2.
- Eneroth M, Apelqvist J, Stenstrom A. Clinical characteristics and outcome in 223 diabetic patients with deep foot infections. Foot Ankle Int, 1997; 18: 716-722. doi:10.1177/107110079701801107.
- Jeffcoate WJ, Harding KG. Diabetic foot ulcers. Lancet, 2003; 361: 1545-1551. doi:10.1016/S0140-6736(03)13169-8.
- Gwilym BL, Mazumdar E, Naik G, Tolley T, Harding K, Bosanquet DC. Initial Reduction in Ulcer Size as a Prognostic Indicator for Complete Wound Healing: A Systematic Review of Diabetic Foot and Venous Leg Ulcers. Adv Wound Care (New Rochelle), 2022. doi:10.1089/wound.2021.0203.
- Ertugrul B, Uckay I, Schoni M, Peter-Riesch B, Lipsky BA. Management of diabetic foot infections in the light of recent literature and new international guidelines. Expert Rev Anti Infect Ther, 2020; 18: 293-305. doi: 10.1080/14787210.2020.1730177.
- Parker CN, Van Netten JJ, Parker TJ, Jia L, Corcoran H, Garrett M, et al. Differences between national and international guidelines for the management of diabetic foot Diabetes Metab Res Rev, 2019; 35: e3101. doi: 10.1002/dmrr.3101.
- Charles Using compression bandages in the treatment of venous leg ulceration. Prof Nurse, 2001; 17: 123-125.
- Onida S, Heatley F, Peerbux S, Bolton L, Lane T, Epstein D, et Study protocol for a multicenter, randomised controlled trial to compare the use of the decellularised dermis allograft in addition to standard care versus standard care alone for the treatment of venous leg ulceration: DAVE trial. BMJ Open, 2021; 11: e041748. doi:10.1136/bmjopen-2020-041748.
- Salim S, Heatley F, Bolton L, Khatri A, Onida S, Davies The management of venous leg ulceration post the EVRA (early venous reflux ablation) ulcer trial: Management of venous ulceration post EVRA. Phlebology, 2021; 36: 203-208. doi:10.1177/0268355520966893.
- FU ZH, WU JD, MEARNS AB, WU D. Under the Skin – A Manual of Fu’s Subcutaneous Needling (FSN) Acupuncture; people's health publishing house: Beijing, China, 2020.
- Fu Foundation of Fu’s Subcutaneous Needling; people's health publishing house: Beijing, China, 2017.
- Liu T, Wen X, Kuang W, Wang X, Jiang Y, Qiu X, et al. Therapeutic effect of Fu's subcutaneous needling for hemiplegic shoulder pain among stroke survivors: Study protocol for a randomized controlled trial. Medicine (Baltimore), 2019; 98: e15507. doi:10.1097/MD.0000000000015507.
- Fu ZH, Wang JH, Sun JH, Chen XY, Xu Fu's subcutaneous needling: possible clinical evidence of the subcutaneous connective tissue in acupuncture. J Altern Complement Med, 2007; 13: 47-51. doi: 10.1089/acm.2006.6125.
- Qi F, Huang H, Cai Y, Fu Z. Adjacent Fu's subcutaneous needling as an adjunctive healing strategy for diabetic foot ulcers: Two case Medicine (Baltimore), 2022; 101: e32271. doi: 10.1097/MD.0000000000032271.
- Liu YC, Margolis DJ, Isseroff RR. Does inflammation have a role in the pathogenesis of venous ulcers? A critical review of the evidence. J Invest Dermatol, 2011; 131: 818-827, doi:10.1038/jid.2010.428.
- Chamanga ET. Understanding venous leg ulcers. Br J Community Nurs, 2018; 23: S6-S15, doi: 10.12968/bjcn.2018.23.Sup9.S6.
- Ambrozy E, Waczulikova I, Willfort A, Bohler K, Cauza K, Ehringer H, et al. Healing process of venous ulcers: the role of microcirculation. Int Wound J, 2013; 10: 57-64. doi:10.1111/j.1742- 2012.00943.x.
- Oliver TI, Mutluoglu Diabetic Foot Ulcer. In StatPearls; Treasure Island (FL), 2022.
- Armstrong DG, Boulton AJM, Bus Diabetic Foot Ulcers and Their Recurrence. N Engl J Med, 2017; 376: 2367-2375. doi:10.1056/NEJMra1615439.
- Krstic RV. Human Microscopic Anatomy: An Atlas for Students of Medicine and Biology. Springer, 2004.
- Langevin HM, Churchill DL, Fox JR, Badger GJ, Garra BS, Krag MH. Biomechanical response to acupuncture needling in humans. J Appl Physiol (1985), 2001; 91: 2471-2478, doi: 10.1152/jappl.2001.91.6.2471.
- Langevin HM, Churchill DL, Cipolla MJ. Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB J, 2001; 15: 2275- 2282, doi: 10.1096/fj.01-0015hyp.

