An Exceptional Case of Traumatic Arteriovenous Malformation in the Chin: Clinical Insights and Implications
Sejal KM1, Kavitha Prasad2, Harini Palinivelu3 and Avinash Baswaraju4,*
1MDS, Associate Professor, Department of Oral & Maxillofacial Surgery, Ramaiah University of Applied Sciences, Bangalore, India
2MDS, Professor and Head, Department of Oral & Maxillofacial Surgery, Ramaiah University of Applied Sciences, Bangalore, India
3MDS, Postgraduate, Department of Oral & Maxillofacial Surgery, Ramaiah University of Applied Sciences, Bangalore, India
4MDS, Postgraduate, Department of Oral & Maxillofacial Surgery, Ramaiah University of Applied Sciences, Bangalore, India
Received Date: 02/09/2024; Published Date: 29/10/2024
*Corresponding author: Avinash Baswaraju, MDS, Postgraduate, Department of Oral & Maxillofacial Surgery, Ramaiah University of Applied Sciences, Bangalore, India
Abstract
Background: Arteriovenous Malformations (AVMs) are lesions where an artery or vessels directly connect to a vein or vessels without passing through a capillary bed. In the head and neck, the primary reasons for intervening in AVMs are hemorrhage and disfigurement.
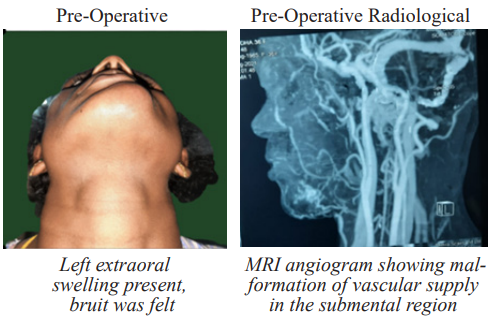
Observation: We present a rare case of a 32-year-old female who reported concerns of facial disfigurement due to a painless swelling. Clinical examination revealed a swelling on the lower left side of the face, which, upon palpation, produced a bruit. A CT angiogram identified feeder arteries, confirming the presence of an arteriovenous malformation in the chin region. The AVM was surgically managed at our institution.
Conclusion: The incidence of arteriovenous malformations (AVMs) in the head and neck region is relatively low. Hemodynamic complications may include venous obstruction, distal ischemia, and high-output cardiac failure. Therefore, early diagnosis and treatment are of utmost importance. In most cases, a thorough clinical evaluation and imaging that clearly delineates the lesion can guide a prudent decision for intervention.
Keywords: Arteriovenous malformation; Vascular malformation; Vascular lesion; Vascular tumor; Chin; AVM (Arteriovenous malformations); Vascular anomalies; Case Report
Introduction
Arteriovenous Malformations (AVMs) are high-flow lesions that rank among the most challenging abnormalities to diagnose and manage surgically. These lesions are particularly rare in the head and neck region. Characterized by a progressive and gradual onset, AVMs can develop in any anatomical area of the body. Within the oral cavity, AVMs are most found on the anterior two-thirds of the tongue, palate, gingiva, and buccal mucosa, reflecting their potential to occur in diverse locations.
The first recorded reference to an AVM is symbolically linked to the image of snakes covering the head of the Greek god Gorgon. AVMs can manifest throughout life and are prone to sudden, dramatic growth spurts triggered by environmental factors. Histologically, AVMs consist of thick-walled, dysmorphic arteries with abnormal venous connections. They have a frequency of approximately 1%, with an estimated incidence of 1-2 per 10,000 births.
Various factors, including trauma, ischemic events secondary to thrombosis, ectasia, hormonal changes, and puberty, can lead to the proliferation of AVMs. Traumatic AVMs typically involve a single vessel, while congenital forms often affect multiple vessels. In previously stable AVMs, infection, trauma, or hormonal changes can precipitate rapid enlargement and bleeding.
Diagnosis of these abnormalities can be achieved through plain radiography, computed tomography (CT) scans, Magnetic Resonance Imaging (MRI), or angiography. The most traditional approach to treating AVMs is surgical excision. While surgery remains the gold standard, it is now often combined with the use of sclerosing agents and embolization techniques.
The following case report details the successful surgical excision of a rare arteriovenous malformation of the chin.
Case Report
A 36-year-old female named Kumudha Kamalesan presented to the Department of Oral and Maxillofacial Surgery at M.S. Ramaiah Dental Hospital, Bangalore, with a complaint of a slow-growing, painless swelling in the left chin region, persisting for the past 10 years. The patient reported a history of trauma 10 years ago, following which a small lesion appeared on the extraoral left chin region three years later, gradually increasing in size.
Extraoral examination revealed a well-defined swelling on the left side of the chin, with no discoloration of the surrounding skin. The swelling extended from the midline to the left corner of the mouth anteroposteriorly and from the lower margin of the lower lip on the left side to the lower border of the chin, measuring approximately 4 x 3 cm. On palpation, the swelling was non-tender, soft in consistency, and exhibited a positive bruit without any local rise in temperature or changes in skin texture [1-5].
Intraoral examination showed obliteration of the vestibule on the left side in the premolar region. Palpation revealed a painless, pulsatile swelling, and a diascopy test demonstrated blanching. The associated teeth were tested for vitality and yielded positive results.
A CT angiogram revealed dilated feeding arteries involving the submental artery and the left facial artery. Based on the clinical examination and chair-side investigations, a provisional diagnosis of acquired arteriovenous Malformations (AVM) was made, with a differential diagnosis of acquired AVMs considered. However, given the detailed history of onset following trauma and the involvement of the left chin region, a clinical diagnosis of acquired AVM was favored.
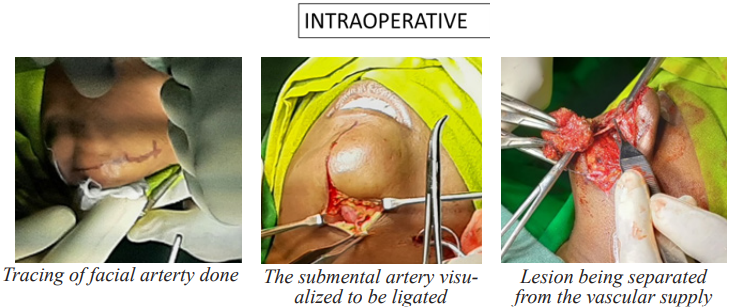
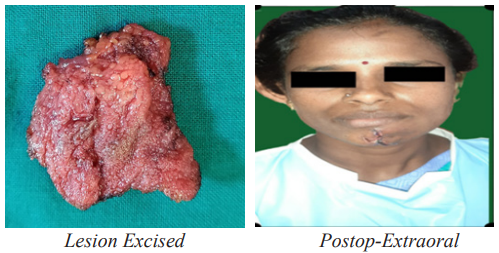
The patient was informed about the diagnosis, treatment options, and the risks associated with performing a biopsy and the surgical procedure. While histopathology is crucial for a definitive diagnosis, it carries a high risk of bleeding during the biopsy. Following a comprehensive systemic examination, the patient underwent surgery, where complete excision of the lesion was performed after ligation of the feeder vessels. The excised specimen was then sent for histopathological examination.
Ligation of the artery and excision of the lesion were performed under general anesthesia. Surface markings were made to trace the course of the facial artery on the left side. An extraoral incision was placed, and the skin and subcutaneous tissue were dissected to expose the facial artery, which was then ligated using stitch ligation. Subsequently, another extraoral incision was made along the midline of the mandible, 2 mm below the lower lip, extending to the left side along the inferior border of the mandible, where the submental artery was identified and ligated [6-9].
After securing the feeder vessels, the lesion was delineated and excised. A 10 ml drain was placed for fluid collection, and the closure was performed using 5-0 Prolene and 3-0 Vicryl sutures. An extraoral pressure dressing was then applied.
The patient was discharged once hemodynamically stable and was scheduled for follow-up to monitor the healing progress. The patient was satisfied with the aesthetic outcome and reported no recurrence during an 18-month follow-up period.
Discussion
The term "vascular anomaly" encompasses a broad spectrum of congenital malformations and tumors of vascular origin, ranging from minor birthmarks to life-threatening and severely disfiguring conditions. Vascular abnormalities include a diverse group of vessel disorders that can affect any part of the vascular system, including the lymphatic vessels, capillaries, veins, and arteries. Each type of abnormality possesses distinct anatomy, pathophysiology, clinical behavior, and requires a specific therapeutic approach [10-13].
Arteriovenous Malformations (AVMs) are high-flow lesions formed by abnormal connections between arteries and veins, bypassing the capillary bed and creating a shunt. Unlike hemangiomas, AVMs exhibit ectasia of abnormal blood vessels lined by flat endothelial cells, rather than endothelial cell proliferation. AVMs result from errors in blood vessel formation during embryogenesis.
Rapid growth of AVMs can be triggered by factors such as trauma, puberty, pregnancy, or hormonal changes. This growth is due to local hemodynamic changes in blood pressure and flow, vessel dilation, and collateral vessel formation, rather than cellular proliferation.
AVMs are chronic, progressive, and potentially fatal, often leading to massive blood loss. They frequently recur after inadequate resection. Extracranial AVMs typically manifest in the cheek, lips, neck, scalp, ear, tongue, and mandible. In patients over 40 years of age, newly developed lesions in previously unaffected areas are often associated with a history of trauma. At this advanced stage, AVMs present with severe symptoms such as bleeding, pain, tissue loss, and ulcer formation. Our patient, a 36-year-old woman, had a history of trauma at the time of presentation.
Clinically, early AVM lesions may present with an overlying vascular blush in the skin. The underlying tissue is typically thicker, non-fluctuant, and non-compressible but pulsatile. When mucosa is involved, it is often thickened and vascular. More advanced lesions may show clearly dilated vessels on the surface and beneath, as well as pulsation. AVMs can infiltrate the skin, leading to ulcerations and bleeding. These characteristics partially aligned with our findings of a painless, pulsatile lesion with swollen vessels [14-17].
Radiographic imaging is essential in the diagnosis and operative planning of arteriovenous malformations (AVMs), utilizing techniques such as ultrasound with color Doppler, contrast-enhanced CT scans, and magnetic resonance imaging (MRI) with angiography. While ultrasound effectively demonstrates high-flow lesions, it may not accurately determine the full extent of the lesion, particularly with deeper involvement. MRI, however, is particularly valuable for assessing the involvement of adjacent soft tissues, with the lesion typically appearing as voids in both T1-weighted and T2-weighted sequences.
The management of AVMs centers on the obliteration of the nidus, the network believed to be responsible for recruiting new blood vessels that contribute to the lesion’s growth. Intra-arterial embolization, which involves occluding the feeder blood vessels, reduces blood flow to the lesion and may induce tumor necrosis. This procedure can be performed as an emergency intervention in cases of massive bleeding or preoperatively to prevent hemorrhage during surgical resection. However, embolization alone is not considered a definitive treatment, as it can lead to ulceration, necrosis, and ischemic changes in the lesion. Therefore, surgical resection is often necessary as an adjunct treatment, especially in high-flow lesions where the lesion may increase in size and cause ischemic pain, ulceration, or bleeding.
In this case, embolization was avoided due to the lesion’s accessibility, while ligation of the feeder artery was feasible. The decision to proceed with complete resection of the lesion after ligating the feeder arteries was influenced by the lesion’s size (4x3 cm), its superficial location, and the absence of neurological deficits. Patient compliance and financial considerations were also taken into account in formulating the treatment plan [18,19].
Although involvement of the oral cavity is common, it often requires innovative management strategies. Depending on their size and location, "problematic" hemangiomas or vascular malformations can significantly impact both function and aesthetics. Bleeding, pain, and disability are also frequent concerns. Therefore, a thorough understanding of the natural history of vascular anomalies is crucial for those who diagnose and treat these conditions.
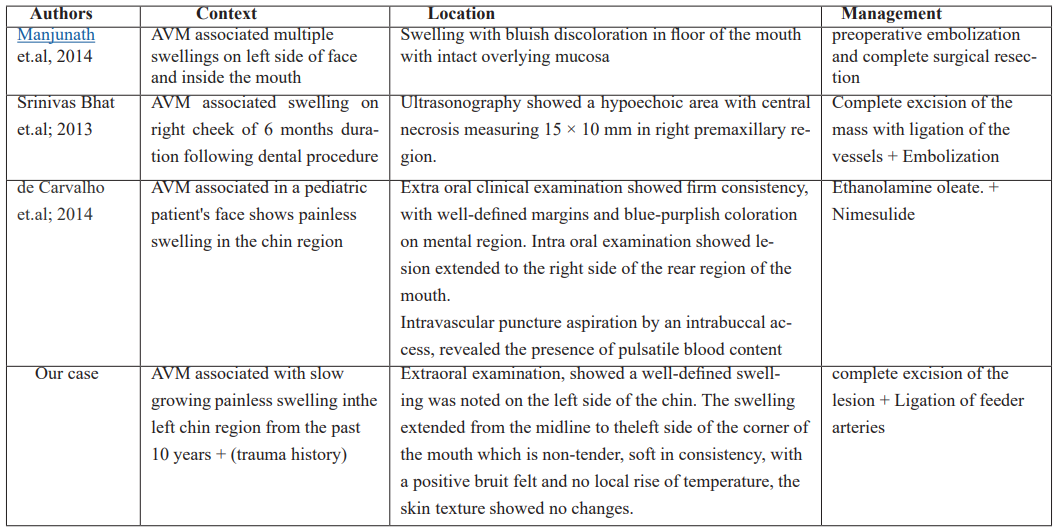
We found few case reports of AVMs which are associated with Head and Neck regions.
Conclusion
The identification and management of arteriovenous malformations (AVMs) require a thorough medical history and accurate clinical diagnosis. While various novel and less invasive treatment options have emerged, surgical excision remains the most effective approach. This method ensures lower recurrence rates and demands less long-term patient compliance.
Informed Consent obtained from the patient.
Funding:Self-supported
Conflict of Interests:None
References
- Righi PD, et Arteriovenous malformation of the base of tongue: Case report and literature review, Microsurgery, 1996; 17(12): pp. 706–709.
- Sham ME, Sultana N. Vascular anomalies in maxillofacial region— Review’, Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology, 2012; 24(3): 137–146.
- Martines F, Immordino V. Arteriovenous malformation of the base of tongue in pregnancy: case report’, Acta Otorhinolaryngologica Italica, 2009; 29(5): 274– 278.
- Christison-Lagay ER, Fishman Vascular anomalies Surg Clin North Am, 2006; 86(2): 393–425.
- Stapf C, Mohr JP, Pile-Spellman J, Solomon RA, Sacco RL, Connolly ES Epidemiology and natural history of arteriovenous malformations. Neurosurg Focus, 2001; 11(5): e1.
- Waner M, Suen Management of congenital vascular lesions of the head and neck. Oncology (Williston Park), 1995; 9(10): 989-994, 997; discussion 998 passim.
- Higuera S, Gordley K, Metry DW, Stal S. Management of hemangiomas and pediatric vascular J Craniofac Surg, 2006; 17(4): 783-789.
- Bhat VS, Aroor R, Bhandary SK, Shetty Traumatic arteriovenous malformation of cheek: A case report and review of literature. Otorhinolaryngol Clin Int J, 2014; 1: 23–27.
- Kumar A, et Arteriovenous Malformation of Face’, Contemporary Clinical Dentistry, 2017; 8(3): pp. 482–484.
- Bhandari PS, Sadhotra LP, Bhargava P, Bath AS, Mukherjee MK, Maurya Management strategy for facial arteriovenous malformations. Indian J Plast Surg, 2008; 41(2): 183-189.
- Manjunath SM, et al. Arteriovenous Malformation of the Oral Cavity’, Case Reports in Dentistry, 2014; pp. 1–5.
- Kumar A, et Arteriovenous Malformation of Face’, Contemporary Clinical Dentistry, 2017; 8(3): pp. 482–484.
- Bhandari PS, Sadhotra LP, Bhargava P, Bath AS, Mukherjee MK, Maurya Management strategy for facial arteriovenous malformations. Indian J Plast Surg, 2008; 41(2): 183-189.
- Manjunath SM, et al. Arteriovenous Malformation of the Oral Cavity’, Case Reports in Dentistry, 2014; pp. 1–5.
- Shailaja SR, Manika Manjula M, Kumar LV. Arteriovenous malformation of the mandible and parotid gland. Dentomaxillofac Radiol, 2012; 41: 609–614.
- Cox Joshua A, et al. “Vascular malformations: a review.” Seminars in plastic surgery, 2014; 28(2): 58-63.
- Lee BB, Do YS, Yakes W, Kim DI, Mattassi R, Hyon WS. Management of arteriovenous malformations: a multidisciplinary J Vasc Surg, 2004; 39(3): 590–600.
- Visser A, FitzJohn T, Tan ST. Surgical management of arteriovenous malformation. J Plast Reconstr Aesthet Surg, 2011; 64(3): 283–291.
- Kohout MP, Hansen M, Pribaz JJ, Mulliken JB. Arteriovenous malformations of the head and neck: Natural history and management. Plast Reconstr Surg, 1998; 102: 64354.

