Mixed Venous and Lymphatic Malformation: Rare Association
Fajri Zineb*, Hanane Baybay, Meryem Soughi, Zakia Douhi, Sara Elloudi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II of Fez, Morocco
Received Date: 04/08/2024; Published Date: 25/10/2024
*Corresponding author: Fajri zineb, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Abstract
Venous and lymphatic malformations are congenital malformations with slow flow, which can be isolated or associated with other malformations. The combination of lymphatic and venous malformations in the same individual remains rare.
We report the case of a patient A 38-year-old woman with no significant past medical history who presented with a venous and lymphatic malformation, diagnosed by ultrasound, Doppler and Magnetic resonance imaging, the patient was treated with sclerotherapy combined with bleomycin and aetoxisclerol, with a successful evolution.
Keywords: Mixed venous; Lymphatic malformation
Introduction
Venous and lymphatic malformations are congenital malformations with slow flow, which can be isolated or associated with other malformations. The combination of lymphatic and venous malformations in the same individual remains rare. Their diagnosis is based on clinical suspicion combined with imaging. Their management is multidisciplinary approach.
Case Report
A 38-year-old woman with no significant past medical history presented to the Department of Dermatology with fluid lesions in the right iliac fossa, associated with an augmentation of the volume of the right leg and recurrent pain and swelling in the leg, which had developed since adolescence and had been treated as venous insufficiency. Dermatological examination revealed multiple white or buff-colored vesicles of variable size, ranging from 1 to 3 mm2, located in the hypogastric region, 1 to 3 mm2, located in the hypogastric region, the presence of multiple bluish compressible swellings on the lateral part of the leg, distributed along the venous territory, echo-doppler was performed, which showed a slow monophasic flow and hypoechoic compressible lesions, an Magnetic resonance imaging was performed to evaluate the extension of the venous malformation. The diagnosis of venous malformation associated with microcystic lymphatic malformation was maintained. The patient was treated with sclerotherapy combined with bleomycin and aetoxisclerol, with a successful evolution.
Discussion
Vascular malformations are congenital dysmorphic vessels that are present at birth but may not become clinically apparent until later in life. They may worsen in severity with age and persist if untreated [1]. The updated International Society for the Study of Vascular Anomalies classification divides vascular malformations into four types: simple, combined, major named vessel(s), and associated with other anomalies [2]. Vascular malformations can also be subdivided according to flow rate: slow flow lesions contain capillaries, veins and/or lymphatics, and fast flow lesions have an arterial component. Venous malformations (VMs) are the most frequent type, accounting for two thirds of all cutaneous vascular malformations [3]. VMs are soft, compressible, non-pulsatile and bluish in color. They may become distended with exercise. They can be focal, multifocal, or diffuse; although they can occur anywhere in the body, focal genital involvement is rare.
History and physical examination are usually sufficient for diagnosis. Doppler ultrasound is the preferred first-line imaging modality for venous malformations involving superficial soft tissues and may be used to identify the anatomy of the feeding vessels. On ultrasound, venous malformations are hypoechoic, compressible lesions in approximately 80% of cases, although in up to 20% of cases venous malformations are isoechoic or hyperechoic.
Phleboliths appearing as hyperechoic masses with posterior shadowing may be seen and are pathognomonic for venous malformations.1 The distinction between venous and lymphatic malformations can be difficult, even in experienced hands, as the pathognomonic signs non-compressible, cysts with thick septa and fluid levels) are not always present or may be complicated by intracystic haemorrhage. Doppler sonography is used to confirm the venous malformation, which has a slow monophasic flow. In approximately
For lymphatic malformations (LMs) are congenital non-proliferative malformations of the lymphatic drainage pathways that result in enlarged vascular and cystic spaces. They can be simple or complex, the complex including elements of other types of vasculatures, particularly venous, as in our case. LM are most usually diagnosed at birth, affecting one in 2000 to 4000 individuals, and result from errors in embryonic development [4]. Lesions most commonly occur in areas of rich lymphatic circulation, including head and neck, axilla, mediastinum, groin, and retroperitonea.
Advancements in the molecular biology and the discovery of somatic mutations that may be responsible for both venous and lymphatic malformations. These vascular malformations are congenital and are due to sporadic somatic mutations in 2 genes. To date, 60% of venous malformations have an activating mutation in the TEK (TIE2) gene, which encodes the TIE2 receptor tyrosine kinase on endothelial cells, and 20% of venous malformations have a mutation in the PIK3CA gene, which results in excessive activation of phosphoinositol 3-kinase (PI3K). These two mutations induce excessive activation of intracellular signaling cascades and in particular the PI3K/AKT/mammalian target of rapamycin (mTOR) pathway), leading to uncontrolled endothelial cell proliferation and disruption of pericyte coverage. These mutations lead to hyperactivation of the PI3K pathway, resulting in abnormal tissue growth, including epithelial and mesenchymal cells. The resulting proliferative syndromes often include slow-flow vascular malformations: lymphatic and venous and vascular malformations, which explains the efficacy of treatment with specific therapies, in particular sirolimus [5].
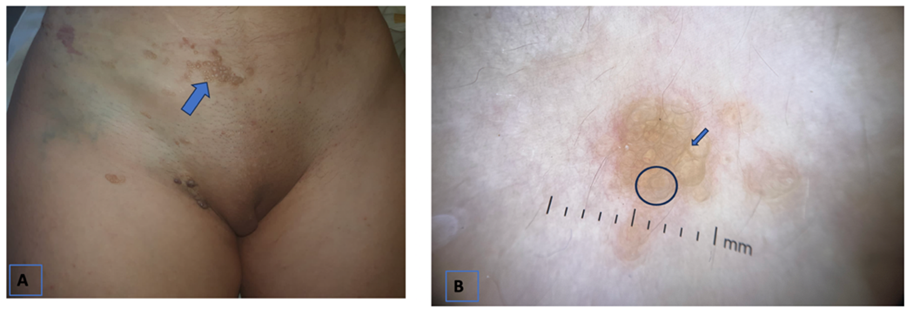
Figure 1: (A)The Clinical manifestation multiple white or buff-colored vesicles of variable size, ranging from 1 to 3 mm2. (B) Dermoscopy revealing yellow lacunae surrounded by pale septa.

Figure 2: (A)The clinical manifestation multiple Bluish distension along the vvenous line. (B) Echodoppler image: lagune veineuse compressible.
Conclusion
Congenital vascular malformations are a heterogeneous group of lesions likely to cause significant morbidity in patients. They remain a constant diagnostic challenge, based on a radio-clinical comparison in which the dermatologist plays a very important role, guiding the radiologist based on distinctive clinical criteria to choose the right examination and look for distinctive radiological criteria. Echo-Doppler is the first-line examination for confirming certain clinical criteria.
IRM is the examination of choice, enabling visualization of the entire malformation. Their management requires a multidisciplinary approach dermatologist, pediatricians, radiologists, geneticists, surgeons.
References
- Colletti G, Ierardi AM. Understanding venous malformations of the head and neck: A comprehensive insight. Med Oncol, 2017. http://dx.doi.org/10.1007/s12032-017-0896-3.
- Gemmete JJ, Pandey AS, Kasten SJ, et al. Endovascular methods for the treatment of vascular anomalies. Neuroimaging Clin N Am, 2013; 23: 703-728.
- Seront E, Vikkula M, Boon LM. Venous malformations of the head and neck. Otolaryngol Clin North Am, 2018; 51: 173-184.
- Neil M Kalwani, Stanley G Rockson.Management of lymphatic vascular malformations: A systematic review of the literature. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 2021; 9(4): 1077-1082. doi: 10.1016/j.jvsv.2021.01.013
- Sirolimus Harbers VEM, Rongen GAPJM, van der Vleuten CJM, Ver- hoeven BH, de Laat PCJ, van der Horst CMAM, et al. Patients with Congenital Low- Flow Vascular Malformation Treated with Low Dose Sirolimus. Adv Ther, 2021; 38(6): 3465–3482. https://doi.org/10.1007/ s12325-021-01758-y.

