Solitary Extramedullary Plasmacytoma of the Orbit: A Case Report and Literature Review
Sidki Kenza*, Madina Rabileh, Essaber Hatim, Omor Youssef And Latib Rchida
Department of Medicine, Mohamed V University Rabat, Morocco
Received Date: 18/08/2024; Published Date: 24/10/2024
*Corresponding author: Sidki Kenza, Department of Medicine, Mohamed V University Rabat, Morocco
Keywords: Plasma tumors; Radiotherapy; Atypical; Location
Introduction
Malignant plasma cell tumors result from the proliferation and accumulation of neoplastic monoclonal plasma cells. They can be either multicentric, such as multiple myeloma, or solitary, and can occur in bone or extramedullary sites. The latter type constitutes a minority (3%) with a much better prognosis. Orbital involvement is an extremely rare site [1], with a male predominance (3:1 ratio) and an onset age between the 6th and 7th decades of life. The main symptom reported in the literature is exophthalmos, with or without diplopia.
Case Report
We report the case of a 61-year-old woman who has been presenting with a rapidly progressing swelling for several months, rendering the eyeball invisible. MRI revealed a preseptal lesion with conjunctivo-palpebral development responsible for enophthalmos.
The patient underwent complete tumor resection due to the rather large volume of the mass, with clear resection margins.
Histopathological examination revealed a diffuse infiltrate composed of plasma cells.
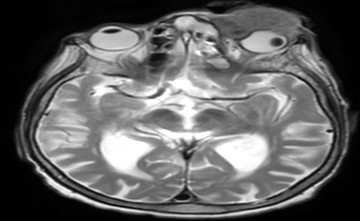
Figure 1: T2 axial showing orbital plasmacytoma.

Figure 2: T2 Sagital Showing Orbital Plasmocytoma.

Figure 3: Surgical resection of orbital plasmacytom.

Figure 4: Histological evidence of orbital plasmacytoma.
Discussion
Several criteria are necessary to diagnose solitary plasmacytoma: absence of anemia, normal serum calcium and phosphate levels, normal renal function, normal bone marrow cytology in at least two different sites, and absence of other lesions on skeletal radiographs or MRI.
The treatment of solitary plasmacytoma primarily relies on radiotherapy (RT); they are radiosensitive and radio-curable tumors. In our series, all patients were treated with radiotherapy, resulting in good local control (87%).
Some studies suggest a minimum dose of 40 Gy to achieve good local control, with higher doses (>40 Gy) associated with a 94% local control rate compared to 69% with lower doses. Others propose doses of 40-50 Gy for small tumors and higher doses for larger tumors [2].
Nevertheless, some authors have not found any dose effect beyond 35 Gy for small tumors and recommend reserving high doses or combined treatment for bulky tumors.
Surgery's role in solitary plasmacytoma is limited, primarily performed for diagnostic purposes and should not be extensive or mutilating [3].
It may be justified for decompressive laminectomy in spinal locations without prior histological evidence or for orthopedic repair in cases of fracture or impending fracture, allowing comfortable radiotherapy administration. In our series, three patients underwent laminectomy surgery.
The role of chemotherapy remains controversial. One prospective study reported benefits with combined chemotherapy and RT compared to RT alone, improving remission and survival duration.
Predictive factors for local recurrence include insufficient radiotherapy doses, the site of solitary bone plasmacytoma, with spinal or pelvic lesions being more challenging to treat than peripheral lesions, and tumor size.
The progression to multifocal lesions is rare and debated, occurring in 2 to 15% of cases in the literature.
These are new bone locations distant from the initial lesion, representing multicentric plasmacytoma rather than myelomatous dissemination. However, distinguishing this from multiple myeloma is not always straightforward, especially since a simple bone marrow biopsy does not definitively exclude dissemination [3].
The prognosis of solitary bone plasmacytoma is dominated by the risk of developing multiple myeloma.
Conclusion
Radiotherapy is an effective treatment for solitary bone plasmacytoma, providing local control in 90% of cases. The prognosis is affected by progression to multiple myeloma, which justifies rigorous monitoring after treatment and suggests a need for consideration of the exact role of chemotherapy [4].
References
- Overweight & Obesity Statistics. National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 2021.
- Furbetta N, Cervelli R, Furbetta F. Laparoscopic adjustable gastric banding, the past, the present and the future. Ann Transl Med, 2020; 8(Suppl 1): S4. doi: 10.21037/atm.2019.09.17.
- Yun GY, Kim WS, Kim HJ, Kang SH, Moon HS, Sung JK, et al. Asymptomatic gastric band erosion detected during routine gastroduodenoscopy. Clin Endosc, 2016; 49(3): 294-297. doi: 10.5946/ce.2016.001.
- Seeras K, Acho RJ, Prakash S. Laparoscopic gastric band placement. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Tabibian N, Swehli E, Boyd A, Umbreen A, Tabibian JH. Abdominal adhesions: A practical review of an often-overlooked entity. Ann Med Surg (Lond), 2017; 15: 9-13. doi: 10.1016/j.amsu.2017.01.021.
- Herndon LK, Stead TG, Ganti L, Jasper T, Lebowitz D. Laparoscopic adjustable gastric band slippage presenting as chest pain. Cureus, 2019; 11(7): e5069. doi: 10.7759/cureus.5069.
- Ma IT, Madura JA. Gastrointestinal complications after bariatric surgery. Gastroenterol Hepatol (N Y), 2015; 11(8): 526-535.
- Management of long-term complications of gastric banding and gastric balloon. Bariatric Times, 2024.
- Furbetta N, Gragnani F, Cervelli R, et al. Technical details and result of a minimally invasive management of gastric band erosions: a series of 47 patients. Obes Surg, 2019; 29: 3754–3761. doi: 10.1007/s11695-019-04170-2.
- Prevention and management of complications after bariatric surgery. BC Med J, 2021; 63(3): 170-178.

