Uterine Inversion Due to Submucous Myoma in a Non-Puerperal Patient
Medemagh Malek*, Haifa Bergaoui, Chayma Cheikh Mohamed, Nadia Chalbi, Hanan Lazreg, Imen Ben Farhat, Toumi Dhekra, Raja Faleh
Department of Gynecology and Obstetrics, Fattouma Bourguiba University Hospital, Monastir, Tunisia
Received Date: 03/08/2024; Published Date: 22/10/2024
*Corresponding author: Malek Medemagh, Department of Gynecology and Obstetrics, Fattouma Bourguiba University Hospital, Monastir, Tunisia
Abstract
Uterine inversion is rare, especially in non-puerperal cases, and often caused by submucous fibroids. We present a case of a 38-year-old woman who experienced uterine inversion during a vaginal myomectomy. She had metrorrhagia, pelvic pain, and a sensation of heaviness, with a 10 cm intravaginal mass. Uterine inversion occurred during fibroid extraction, and the Johnson maneuver failed, requiring emergency laparotomy. Correction involved posterior colpotomy, plication of round ligaments, and ligation of uterine arteries. Recovery was uncomplicated. Non-puerperal uterine inversions are rare, linked to submucosal leiomyomas, and present with abnormal bleeding, pelvic discomfort, and a protruding mass. Surgical intervention varies from vaginal repositioning to laparotomy. Preventive surgery for large submucous leiomyomas is recommended to avoid such complications.
Keywords: Leiomyoma; Uterine Inversion; Submucusal Myoma
Introduction
Uterine inversion can be categorized into puerperal (obstetric) and nonpuerperal (gynecological) types. Nonpuerperal uterine inversion is considered rare and typically results from tumors located at the uterine fundus, which exert a traction force leading to the inversion [1].
Prolapsed fibroids are the most common trigger, with occasional reports linking uterine inversion to uterine neoplasms and endometrial polyps. The proposed contributing factors include: the sudden emptying of a uterus previously distended by a tumor, the thinning of the uterine walls due to an intrauterine tumor, and the dilation of the cervix.
Here, we detail the assessment and treatment of a multiparous woman in her 30s who arrived at our maternity unit with abnormal bleeding. During an emergency myomectomy, this led to a uterine inversion.
Case Report
This case involves a 38-year-old multiparous woman with no significant medical history, who was admitted to the emergency department of our maternity unit due to metrorrhagia that had been ongoing for several months, accompanied by pelvic pain and a sensation of heaviness. Upon clinical examination, the patient appeared pale, hemodynamically unstable, with discolored conjunctiva, and presented with a 10 cm intravaginal mass suggestive of a fibroid expelled through the cervix. A suprapubic ultrasound confirmed the diagnosis of an intracavitary fibroid expelled through the cervix, measuring more than 10 cm. The patient underwent a myomectomy via the vaginal route. During the fibroid extraction, an accidental uterine inversion occurred. An attempt to reintegrate the uterus using the Johnson manouvre was unsuccessful. Consequently, an emergency laparotomy was indicated, involving a posterior colpotomy and reduction of the inversion, followed by plication of the round ligaments and ligation of both uterine arteries (Figure 1). The postoperative course was uncomplicated.
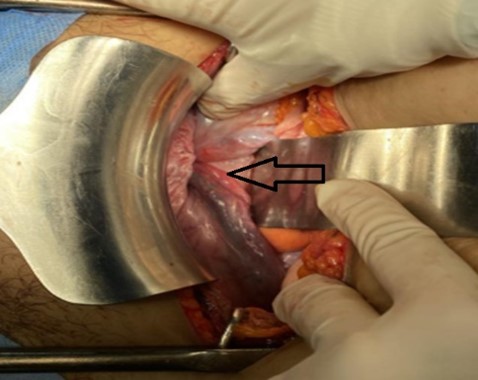
Figure 1: Operative image of uterine inversion : An arrow indicating site of uterine inversion with bilateral tubes and ovarian ligaments pulled in.
Discussion
Uterine inversions are classified into two categories: puerpéral and non-puerperal inversions [2].The incidence of spontaneous uterine inversion outside the postpartum period is exceptionally rare, comprising only 5% of all uterine inversion cases. This condition is typically linked to the presence of a polypoid mass in the uterine fundus, commonly a uterine leiomyoma or a uterine sarcoma [3].
There are relatively few published cases of uterine inversion in the gynecological setting. However, when it does occur, it presents a diagnostic and management challenge due to its rarity and complexity. Fifty-six cases have been documented in the literature between 1976 and 2014. In the majority of these cases, it involved postmenopausal women or women over the age of 45 [4].
Non-puerperal uterine inversions are predominantly caused by benign submucosal uterine leiomyomas, but can also result from conditions such as rhabdomyosarcoma, leiomyosarcoma, or endometrial polyps. Typical symptoms of non-puerperal uterine inversion include anemia from abnormal vaginal bleeding, vaginal discharge, lower abdominal or pelvic discomfort, a protruding vaginal mass, and, occasionally, urethral obstruction [5].
Several factors are implicated in the pathophysiology of non-puerperal uterine inversion: the presence of a uterine tumor preferably located on the uterine fundus; situated on a thin uterine wall; with a small tumor pedicle; rapid tumor growth; and cervical dilation due to distension of the uterine cavity [6].
This scenario applied to our patient, who had a tumor developing on the fundus of the uterus. According to the severity, uterine inversion is classified into four degrees: first degree: the uterine fundus is depressed into a "bottle cap" or cup-like shape; second degree: the inverted uterus extends through the external cervical orifice; third degree: the uterine body becomes intravaginal and may completely exteriorize; fourth degree or total inversion: the vaginal walls are also involved in the inversion [7,8].
Surgery for uterine inversion can be quite challenging, and various surgical approaches have been documented in the literature. In some instances, a vaginal myomectomy is first carried out, followed by abdominal repositioning of the inverted uterus or, in some cases, a hysterectomy [9].
Conclusion
Non-puerperal uterine inversion, though rare, can be life-threatening. It is most commonly associated with intrauterine tumors, particularly leiomyomas. Repositioning can be performed either vaginally or via laparotomy. So every patient with a large submucous leiomyoma should be operated to prevent this complication.
Ethics statements
Patient consent for publication: Consent obtained directly from patient(s).
- ContributorsThe following authors were responsible for drafting of the text, sourcing and editing of clinical images, investigation results, MM, HB, CC, NC, HL, and I F. The following authors gave final approval of the manuscript: DT and RF.
- FundingThe authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
References
- Dadgar S, Pourhosseini SA. Non Puerperal Uterine Inversion Due to Submucous Myoma: A Case Report. J Family Reprod Health, 2018; 12(3): 169-172.
- Moshayedi F, Seidaei HS, Salehi AM. A Case Report of Non-puerperal Uterine Inversion due to Submucosa Leiomyoma in a Young Virgin Woman. Case Rep Surg, 2022; 2022: 5240830. doi: 10.1155/2022/5240830.
- Lupovitch A, England ER, Chen R. Non-puerperal uterine inversion in association with uterine sarcoma: Case report in a 26-year-old and review of the literature. Gynecol Oncol, 2005; 97: 938–941.
- Benjelloun AT, Makayssi A, Ennachit S, Elkarroumi M. Inversion utérine non puerpérale chronique: à propos d’un cas [Chronic non-puerperal uterine inversion: about a case]. Pan Afr Med J, 2018; 31: 231. doi: 10.11604/pamj.2018.31.231.16668.
- de Vries M, Perquin DAM. Non-puerperal uterine inversion due to submucous myoma in a young woman: a case report. Journal of Medical Case Reports,2010; 4(1): 1–3. doi: 10.1186/1752-1947-4-21.
- Abid S, Dhaou GB, Abdelmoula G, Smida AB, Abdesslem MRB, Mrad O, et al. Complete non-puerperal uterine inversion caused by uterine hemangioma: about a case report. Pan Afr Med J, 2022; 42: 156. doi: 10.11604/pamj.2022.42.156.35583.
- Pauleta JR, Rodrigues R, Melo MA, Graça LM. Ultrasonographic diagnosis of incomplete uterine inversion. Ultrasound Obstet Gynecol,2010; 36: 260–261.
- Wang W, Wang J. Uterine Inversion Secondary to Endometrial Carcinoma. J Med Cases, 2023; 14(1): 7-12. doi: 10.14740/jmc4023.
- Alsahabi J, Alsomairi A, Elmuzaini F. Non-puerperal uterine inversion due to submucosal fibroid in a nulliparous woman: A case report. Int J Case Rep Images, 2019; 10: 101008Z01JA2019.

