Paravertebral Extramedullary Hematopoiesis
Rabileh Madina*, Lanjerie Safae, Sidki Kenza, Insumbo Paulino, Wen-Yam Traoré, Saleheddine Tariq, Zamani Ouijdane, Edderai Meryem and El Fenni Jamal
Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Received Date: 08/08/2024; Published Date: 21/10/2024
*Corresponding author: Rabileh Madina, Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Abstract
Extramedullary Hematopoiesis (EMH) corresponds to the ectopic development of hematopoietic tissue outside the bone marrow this phenomenon is encountered in chronic hemolytic anemia myelofibrosis neoplasia with bone marrow invasion. The most common location involves the reticuloendothelial system and paravertebral involvement is rare. HEM lesions are rarely symptomatic but can manifest as bleeding which constitutes the main clinical manifestation and also certain complications such as spinal cord compression. The diagnosis is based on the clinical-biological context and essentially on magnetic resonance imaging which is the gold standard for the exploration of this rare entity. .Treatment combines, depending on the case, repeated transfusions, surgery, radiotherapy, corticosteroid therapy or hydroxyurea. In the absence of clinical signs, therapeutic abstention and radiological monitoring are recommended.
In our case we illustrate the exploration of paravertebral masses of fortuitous discovery as part of an assessment of a rhabdomyosarcoma of the right maxillary sinus.
Keywords: Anemia; Paravertebral Extramedullary Hematopoiesis (PVEMH)
Introduction
Extramedullary hematopoiesis or “medullary heterotopia” or also called “hematopoietic lipoma” is a classic entity complicating the evolution of numerous chronic hematological conditions (sickle cell disease, thalassemia, neoplasia, etc.). This is a phenomenon of compensation for bone marrow dysfunction in other hematopoietic organs. Extra-medullary para-vertebral hematopoiesis is secondary to a hematological pathology causing chronic anemia, the development of hematopoietic tissue then takes place outside the bone marrow and it is very rarely described in the literature, to date only a few cases have been reported in the literature [1].
We report the case of a 22-year-old patient followed for rhabdomyosarcoma of the right maxillary sinus in whom biological assessments revealed bicytopenia (anemia and thrombocytopenia), and during her evaluation assessment imaging revealed bilaterale dorsal paravertebral tissue masses. We describe this rare pathology as well as the radiological characteristics of this entity, notably CT and MRI.
Case Report
This is a 20-year-old patient followed in the oncology department for a locally advanced rhabdomyosarcoma of the right maxillary sinus, including initial CTAP scan showed an aggressive right maxillary tumor process with extension to the nasal cavity, orbit and endocranium (Figure 1a), treated with chemotherapy (6xVIDE protocol vincristine ifosphamide ectoposide doxorubicin) + radiotherapy .After 1 year of treatment, the clinical examination showed conjunctiva in a context of apyrexia and preservation of general condition and back pain .The biological assessment shows a normocytic normochrome regenerative anemia (Hb at 7g/dL) with schistocytes less than 1% in the blood smear; bacterial serology and autoimmunology prove negative. CTAP CT during evaluation showed a clear regression in size and volume of the large lytic mass centered on the right maxillary sinus and we noted the appearance of tissue masses of the bilateral paravertebral soft tissues next to D1 to D3 and from D9 to D10 regular contours, well limited, without calcifications, enhanced homogeneously after injection of contrast product, filling the costovertebral angles with doubt on an endocanal extension (Figure 1b, 1c, 1d) requiring comparison with spinal magnetic resonance imaging (MRI) . MRI spine examination demonstrated that the bilateral paravertebral bifocal segmental tissue masses have the same signal characteristics with the marrow of the adjacent vertebral body, isointense on T1 and T2 WI images, enhanced homogeneously after injection with bilateral foraminal and intracanal extramedullary extension associated with anterolateral epiduritis more marked at the level of D2 (Figure 2a, 2b, 2c, 2e). There were no adjacent bony lesions or pleuro-parenchymal abnormalities. There was no associated lymphadenopathy. The diagnosis of paravertebral extramedullary hematopoiesis (HEMPV) was made given the clinical-biological context and the radiological appearance. The attitude was therapeutic abstention associated with correction of hematological disorders. A CT scan after 4 months showed partial regression of the paravertebral masses with preservation of the general condition.
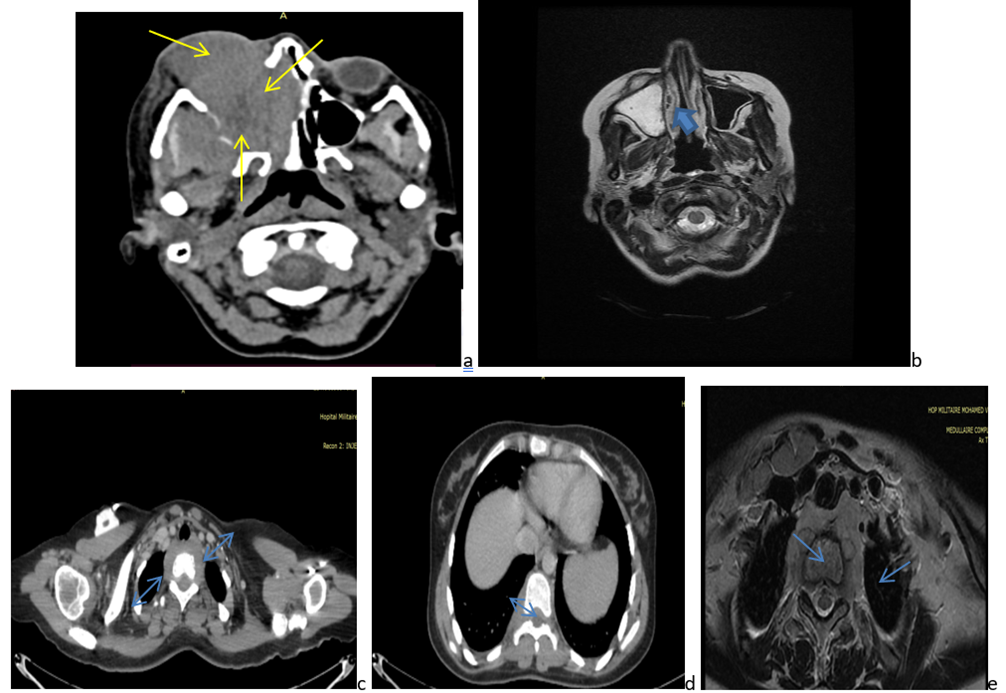
Figure 1: (a) cervical CT axial view with contrast iv injection showed large lytic mass centered on the right maxillary sinus with extension to the nasal cavity, orbit( yellow arrow). (b) cervical MRI axial view T2 : note the regression of the large lytic masse (arrow head). (c,d ): Thoracic abdominal CT in axial section after injection of contrast product: Bilateral paravertebral tissue masses , soft tissues next to D1 to D3 (c) and from D9 to D10 (d) regular contours, well limited , without calcifications, without adjacent vertebral bone lesion, enhanced homogeneously (full arrow). (e) MRI of the cervico-thoracic spine axial view, showed bilateral paravertebral tissue masses have the same signal characteristics with the marrow of the adjacent vertebral body, isointense T2 WI images, with bilateral foraminal and intracanal extramedullary extension (blue arrow).
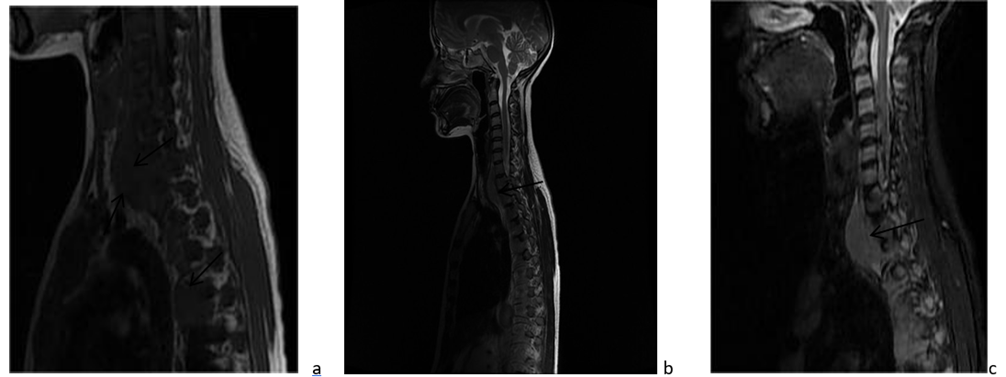
Figure 2: (a) MRI spine sagital view showing bilateral paravertebral bifocal segmental soft tissue masses, isointense on T1 and (b) T2 WI images, (c) Enhanced homogeneously after injection, with bilateral foraminal and intracanal extension, without adjacent vertebral bone.
Discussion
Extramedullary Haematopoiesis (EMH) develops as a compensatory response to inadequate blood cell production, leading to the proliferation of hematopoietic cells outside the bone marrow when the body requires more blood cells than are being produced [2,3]. Extramedullary hematopoiesis preferentially develops in sites involved in hematopoiesis during fetal life that cease to produce erythrocytes at birth but retain this capacity in cases of ineffective erythropoiesis, such as the liver, spleen, and lymph nodes [4,5]. Rare localisations such as the kidneys, adrenal glands, peritoneum, and the pre-sacral region should also be investigated. Other rare sites can be affected, particularly the paraspinal tissue, with a predominance in the paravertebral compartments, as described in our case.The pathophysiology of paravertebral extramedullary hematopoiesis is not yet well understood. It is thought to involve either a transformation of embryonic osteogenic tissue into hematopoietic tissue in cases of chronic anemia, or an extension of hematopoietic tissue through the proximal costal tubercles or adjacent vertebral bodies. Most often, these paravertebral masses are asymptomatic, but they can sometimes lead to serious neurological lesions due to their proximity to the spinal canal. Chest CT usually shows a tissue mass paravertebral lobulated, uni- or bilateral, well limited, seat subpleural, without bone lysis, and containing adipose tissue, alone does not exclude the differential diagnoses suggested by such image from other costovertebral angle masses, such as neurogenic tumours, lymphoma, metastasis, paravertebral abscess. Magnetic resonance imaging in this case is the reference examination and makes it possible to confirm the diagnosis and clarify the epidural and meningeal lesion extension. On MRI, the EMH foci have a variable presentation, particularly depending on the active nature or not of the lesion. These are most often heterogeneous or homogeneous bilateral para-vertebral masses, well defined, of variable size, with a more or less significant fatty component, without calcification within them and without adjacent vertebral bone lesion [1,6-8). When contrast material is injected, enhancement is often moderate. There is no associated lymphadenopathy, unlike lymphoma which remains a differential diagnosis to be ruled out. EMH should be considered in the differential diagnosis in a patient with chronic severe anaemia and a paraspinal mass.In cases of incidental findings of lesions without significant clinical signs, it is recommended to opt for therapeutic abstention along with imaging surveillance. However, there is currently no standardized and validated protocol for this surveillance [4]. Typically, para-spinal masses tend to regress with the correction of hematopoietic disorders. Therefore, it is crucial to be able to suggest the diagnosis in the context of hematopoietic dysfunction, especially when typical imaging results are present.
Conclusion
Extra-medullary para-vertebral hematopoiesis corresponds to the ectopic development of hematopoietic tissue outside the bone marrow should be considered in any patient presenting with a paravertebral mass in a context of hemoglobinopathy. The clinical examination,simple radiological and isotopic explorations and not invasive procedures help confirm the diagnosis.
References
- Delavaud C, Lincot J, Debray M, Schouman-Claeys E, Dallaudiere B. An incidental posterior mediastinal mass. Diagn Interv Imaging, 2014; 95: 121-122.
- BerKmen YR, Zalta BA. Extramedullary Hematopoiesis. Radiology, 2007; 245: 905-908.
- Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK. Typical and atypical presentations of extramedullary hemopoiesis. AJR, 2002; 179: 1239–1243.
- Laamrani F, Dafiri R. [Large hilum in a child with sickle cell anemia. Extramedullary hematopoiesis]. Arch Pediatr, 2015; 22: 88-89, 104-105.
- Psichoglou H, Malagarl K, Spanomichos G. Mediastinal extramedullary hematopoiesis in hemolytic anemia. JBR-BTR, 2004; 87: 150-151.
- Maazoun F, Gellen Dautremer J, Boutekadjirt A, Pissard S, Habibi A, Bachir D, et al. [Symptomatic extramedullary haematopoiesis in β-thalassemia: A retrospective single centre study]. Rev Med Interne, 2016; 37: 5-12.
- Ogier M, Kerjouan M, Libessart T, Merzoug A, Leroyer C, Desrues B, et al. [Posterior mediastinal mass]. Rev Mal Respir, 2015; 32: 959-962.
- Chourmouzi D, Pistevou-Gompaki K, Plataniotis G, Skaragas G, Papadopoulos L, Drevelegas A. MRI findings of extramedullary haemopoiesis. Eur Radiol, 2001; 11: 1803–1806.

