Complex Gastrocolic Fistula in a Young Woman with Crohn’s Disease: A Case Report and Review of Diagnostic and Therapeutic Challenges
Muhammad Subhan¹,*, Ruqiya Bibi², Syed Muhammad Zaid Alvi³, Muhammad Omaise Zafar⁴, Muhammad Hamza⁵, Naiha Talha⁶ and Bibi Sarah Yousofzai⁷
1Department of Gastroenterology, Allama Iqbal Medical College Lahore/Jinnah Hospital Lahore, Pakistan
2Department of Medicine, Allama Iqbal Medical College Lahore/Jinnah Hospital Lahore, Pakistan
3Ziauddin Medical College, Pakistan
4Dow Medical College, Karachi, pakistan
5Department of General Surgery, Allama Iqbal Medical College Lahore/Jinnah Hospital Lahore, Pakistan
6Department of Internal Medicine, Allama Iqbal Medical College Lahore, Pakistan
7Department of Gynecology and Obstetrics, Be Team International Cure Hospital, Kabul, Afghanistan
Received Date: 24/07/2024; Published Date: 10/08/2024
*Corresponding author: Muhammad Subhan, Department of Gastroenterology, Allama Iqbal Medical College Lahore/Jinnah Hospital Lahore, Pakistan
Abstract
A gastrocolic fistula, an abnormal connection between the stomach and colon, can arise from conditions such as malignancies, Crohn's disease, peptic ulcer disease, or surgical complications. This case report discusses a 29-year-old woman with Crohn's disease who presented with epigastric and paraumbilical pain, foul-smelling vomitus, black stools, and significant weight loss. Physical examination revealed tenderness and signs of inflammation, while endoscopy confirmed the presence of a gastrocolic fistula. Initial treatment with corticosteroids and Infliximab was ineffective, necessitating surgical intervention, nutritional support, and medications to minimize fistula output. This case underscores the importance of early diagnosis, multidisciplinary management, and the potential need for surgery in treating gastrocolic fistulas. Further research is essential for developing standardized diagnostic and treatment protocols to improve patient outcomes.
Keywords: Gastrocolic fistula; Crohn's disease; Abdominal pain; Endoscopic examination; Collaborative healthcare
Introduction
A gastrocolic fistula represents an atypical conduit between the stomach and colon, permitting the direct transfer of stomach contents into the colon, resulting in various gastrointestinal complaints [1]. Such fistulas typically develop as complications of conditions like cancer, Crohn's Disease (CD), Peptic Ulcer Disease (PUD), or complications of any gastrointestinal surgical procedure [2-4]. Its incidence is challenging due to its infrequency and diverse origins [3]. Presently, cancers, especially those of the stomach and colon, along with CD, are the primary causes [2-4]. While there is no distinct preference for either gender, it is more commonly reported in older people and younger women, mirroring the age distribution of its root causes [5]. Without treatment, a gastrocolic fistula can lead to critical complications such as malnutrition, infection, and mortality [5]. Prompt detection and a collaborative treatment approach are essential for effective therapy and better patient outcomes [4,5]. The pathogenesis of a gastrocolic fistula involves an inflammatory process that causes ulceration in the walls of the stomach and colon, culminating in the creation of a fistula [6]. Genetic predisposition plays a significant role in inflammatory bowel diseases (IBD) like CD, where genetic factors contribute to the likelihood of developing the disease [7]. Specific genetic mutations, such as those in the NOD2/CARD15 gene, are implicated in CD, potentially affecting the risk of fistula development [7]. CD can impact any segment of the gastrointestinal tract and is marked by persistent inflammation, leading to various gastrointestinal symptoms and complications [8]. It is more prevalent among individuals of Northern European descent and usually manifests as a chronic, recurring condition, often appearing in teenagers and young adults [8]. Symptoms differ based on the affected area and include abdominal pain, diarrhea, fever, and weight loss, significantly affecting life quality [8,9]. The disease is characterized by inflammation that penetrates the entire thickness of the intestinal wall, resulting in severe complications such as fistulas, abscesses, constrictions, and perianal disease [8,9]. Diagnosing CD demands a high level of clinical suspicion due to symptom overlap with other conditions, typically necessitating endoscopic procedures to identify characteristic ulcerations and corroborative imaging tests [10]. Treatment encompasses corticosteroids, immunomodulators, antibiotics, biological therapies, and occasionally surgical procedures for severe cases or complications [10]. Timely diagnosis and proper management can substantially decrease the morbidity and mortality associated with CD, aiming to sustain remission, alleviate symptoms, and enhance patients' overall quality of life [10].
The diagnostic assessment of a gastrocolic fistula involves a blend of endoscopic and imaging evaluations [7,8]. Gastroscopy and colonoscopy are crucial for visualizing the fistula and acquiring tissue samples for biopsy [8,9]. Imaging techniques, such as Computerized Tomography (CT) scans, offer detailed anatomical insights and assist in determining the fistula's extent [8,9]. Histopathological analysis is vital for identifying the root cause, especially distinguishing between benign inflammatory conditions and malignancies [9]. Managing a gastrocolic fistula depends on the underlying cause and the patient's general health [9,10]. Surgical intervention is often necessary, particularly in cases of malignancy or when conservative treatment is unsuccessful [9,10]. The surgical approach involves removing the affected sections of the stomach and colon and repairing the fistula [10]. Medical management, including nutritional support and addressing underlying conditions like CD, is also crucial [10]. Pharmacological therapy includes corticosteroids, antibiotics, immunosuppressants, IBD biologics, and cancer chemotherapy [10].
Case Presentation
A 29-year-old woman with a history of CD came forward with a two-year history of sporadic pain in the epigastric and paraumbilical regions, initially accompanied by occasional blood-tinged vomiting. In the last two weeks, her vomiting became odorous, dark, and contained undigested food. She also reported multiple episodes of black, sticky stools for the past two months, which worsened following recent childbirth, and a significant weight loss of roughly 12 kg. Physical examination showed her to be emaciated, frail, and pallid, with slight sensitivity in the epigastric and left upper quadrant areas. No signs of jaundice, nail deformities, koilonychia, swollen lymph nodes, or swelling were present. The rest of the systemic examination was unremarkable. Laboratory tests indicated a white blood cell count of 11.4K cells/µL, hemoglobin levels of 9.6 g/dL, and platelet count of 457K cells/µL. All other serological tests were normal, except for a slight drop in sodium levels (Na 133 mmol/L).
Endoscopic examination revealed a normal esophagus, a functioning lower esophageal sphincter at 38 cm, and inflamed, fragile mucosa in the stomach's lower region with a sizable opening, dead tissue, and fecal discharge. Figure 1 shows an endoscopic image of the colonic mucosa where tarry fecal matter can be seen.

Figure 1: Endoscopic view of colonic mucosa showing fecal matter.
The scope could pass deeply into the opening, leading to the colon. The pylorus was normally open, and the duodenum's lining appeared healthy in the first two sections. Biopsy samples from the lesion suggested an underlying inflammatory condition, likely CD. An abdominal X-ray showed a small shadow in the stomach area and gases in the intestines. Figure 2 shows the presence of gases in the transverse colon leaking from the stomach due to the gastrocolic fistula.

Figure 2: Air fluid level in the Gut due to the presence of a gastrocolic fistula.
Further imaging, including a CT scan of the abdomen and pelvis, indicated thickening of the mucosa in the ascending, transverse, and descending colon, eroded mucosa in the transverse colon communicating with the stomach lining, and the presence of gas within the walls of the stomach or colon due to the fistula. Figure 3 shows the gut wall thickening with mucosal enhancement, mesenteric fat strandings, and bilateral kidneys, which also show kidney stones.

Figure 3: Gut Wall Thickening with Mucosal Enhancement, Mesenteric Fat Strandings, and Bilateral Kidney Stones.
Figure 4 shows histological examination features of CD, such as distorted crypt architecture, inflammatory expansion of the lamina propria with basal lymphoplasmacytosis, and inflammation across the entire wall thickness with lymphoid clusters.
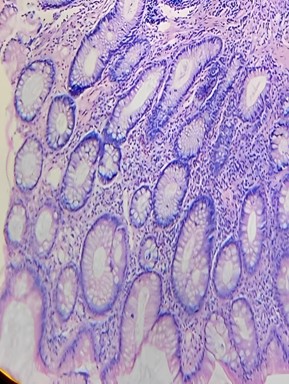
Figure 4: Histological Features of Crohn's Disease: Distorted Crypt Architecture, Inflammatory Expansion of the Lamina Propria, and Transmural Inflammation with Lymphoid Clusters.
The case was reviewed in a multidisciplinary team (MDT) meeting where the patient actively participated in the discussion, voicing her questions and concerns. First-line medical management was planned to cope with acute flare of CD and to heal gastrocolic fistula. The team clarified the reasoning behind the chosen management strategy and the potential risks and benefits. The patient's comprehension and consent were essential in finalizing the plan. She received medical treatment for CD, including high-dose steroids of 40 mg per day, which is gradually reduced for 4–8 weeks in an acute flare, then shifted to Infliximab as an intravenous infusion with the initial dose of usually 5 mg/kg. Additional doses were given 2 and 6 weeks after the first infusion, followed by maintenance doses every eight weeks. However, symptoms persisted with malnutrition despite medical therapy. A Follow-up CT scan also showed the persistence of the fistula. The case was re-discussed in MDT, and a final plan was made for fistulotomy with nutritional support, prokinetics, and octreotide to minimize output.
Discussion
Gastrocolic fistulas are rare but serious complications arising from various conditions, including CD, tuberculosis (TB), PUD, Colorectal Carcinoma (CRC), and stomach cancer [1-4]. This case report highlights the complexity and challenges associated with diagnosing and managing gastrocolic fistulas, particularly in patients with CD [2]. Persistent and full-thickness inflammation in CD can lead to fistula formation, with genetic predispositions such as NOD2/CARD15 mutations increasing susceptibility [2]. Gastrointestinal TB can cause fistulas through caseating granulomas, especially in high-incidence areas [3]. Malignancies like CRC and stomach cancer can also precipitate gastrocolic fistulas through invasive tumor growth [4,5].
Diagnosing gastrocolic fistulas requires a high index of suspicion, particularly in CD patients [5]. Endoscopic examination is crucial for visualizing the fistula and obtaining biopsy samples, while imaging studies like CT scans provide detailed anatomical insights [6]. Histopathological examination distinguishes between benign inflammatory conditions and malignancies [6,7]. In this case, endoscopy confirmed a gastrocolic fistula, revealing inflamed mucosa and fecal discharge [7]. Initial medical management with corticosteroids and Infliximab was attempted but proved ineffective, necessitating surgical intervention. Surgical management included fistulotomy, nutritional support, and medications like prokinetics and octreotide to minimize fistula output. The prognosis of gastrocolic fistulas varies based on the underlying cause and timeliness of diagnosis and treatment. Early detection and a coordinated multidisciplinary approach are crucial for optimizing outcomes. This case underscores the potential need for surgery in refractory cases and the importance of individualized treatment plans. Nutritional support and careful monitoring are essential for post-operative care to ensure recovery and prevent complications.
Several similar clinical studies have reported on the challenges and management of gastrocolic fistulas. For instance, a case report by Aslam et al. described a 77-year-old male with a gastrocolic fistula secondary to a transverse colonic tumor [11]. The patient presented with feculent vomiting and weight loss, and the diagnosis was confirmed via CT scan and endoscopy [11]. Surgical intervention, including an extended right hemicolectomy and distal gastrectomy, was performed as a palliative measure [11]. Another case report by Gourishankar et al. detailed an adolescent patient who developed a gastrocolic fistula as a complication of percutaneous endoscopic gastrostomy (PEG) [12]. The patient required corrective surgery after imaging confirmed the fistula [12]. These cases, like the present one, emphasize the importance of timely diagnosis and the potential need for surgical intervention. Future research should focus on developing standardized diagnostic and treatment protocols, advancing minimally invasive surgical techniques, and exploring targeted medical therapies. Genetic studies could provide insights into predispositions and facilitate personalized medicine approaches in conditions like CD and gastric cancer. Ongoing clinical research and case reporting are vital for understanding and managing this complex condition.
In conclusion, though rare, gastrocolic fistulas pose significant diagnostic and therapeutic challenges. Early diagnosis, multidisciplinary management, and potential surgical intervention are essential for treating gastrocolic fistulas effectively. Continued research and case reporting are critical to developing effective management strategies and improving patient outcomes.
Conclusion
This case of a young woman with a gastrocolic fistula secondary to CD highlights the intricate diagnostic and therapeutic challenges of this rare condition. Extensive diagnostic investigations, including gastroscopy, colonoscopy, and CT imaging, confirmed the fistula and underlying inflammatory disease. The case emphasizes the need to consider gastrocolic fistula in patients presenting with chronic gastrointestinal symptoms and significant weight loss, necessitating a multidisciplinary approach to treatment. Surgical repair combined with medical management for CD is critical. Future research should unravel the pathophysiological mechanisms, enhance diagnostic precision, and establish standardized treatment protocols. Advances in minimally invasive surgery and targeted treatments offer hope for improved outcomes.
Further genetic and molecular studies could lead to personalized treatment strategies. Although rare, gastrocolic fistulas require prompt diagnosis and collaborative care. Continued clinical research and case documentation are vital for a deeper understanding and better managing this complex condition.
References
- Zhou B, Li W. A case of gastrocolic fistula secondary to adenocarcinoma of the colon. Int J Surg Case Rep, 2015; 15: 46-49. doi: 10.1016/j.ijscr.2015.08.023.
- Azouz SB, Hassine H, Debbabi H, Yacoub H, Cherif D, Elkhouni B, et al. Gastrojejunocolic fistula: a rare complication of peptic ulcer surgery. J Surg Case Rep, 2023; 2023(7): rjad125. doi: 10.1093/jscr/rjad125.
- Badiani S, Kashkooli S, Tang M, Strugnell N. A shortcut to Gut: gastrocolic fistula secondary to gastrointestinal tuberculosis (TB). ANZ J Surg, 2023; 93(1-2): 407-409. doi: 10.1111/ans.17855.
- Aydin U, Yazici P, Ozütemiz O, Güler A. Outcomes in the management of gastrocolic fistulas: a single surgical unit's experience. Turk J Gastroenterol, 2008; 19(3): 152-157.
- Mansour S, Marjiyeh-Awwad R, Khuri S. Gastrocolic Fistula: An Extraordinary Gastrointestinal Fistula. Gastroenterology Res, 2022; 15(6): 308-313. doi: 10.14740/gr1576.
- Wu S, Zhuang H, Zhao JY, Wang YF. Gastrocolic fistula in Crohn's disease detected by oral agent contrast-enhanced ultrasound: A case report of a novel ultrasound modality. World J Gastroenterol, 2020; 26(17): 2119-2125. doi: 10.3748/wjg.v26.i17.2119.
- Aktan I, La Ragione RM, Woodward MJ, Ando H, Abe H, Sugimoto N, et al. Gastrointestinal infections. Microbiology, 2007; 153: 464-473.
- Menni A, Tzikos G, Rafailidis V, Krokou D, Karlafti E, Michalopoulos A, et al. Gastrocolic fistula in Crohn's disease: A case report and review of the literature. Radiol Case Rep, 2022; 17(12): 4756-4760. doi: 10.1016/j.radcr.2022.09.009.
- Torres J, Mehandru S, Colombel JF, Peyrin-Biroulet L. Crohn's disease. Lancet, 2017; 389(10080): 1741-1755. doi: 10.1016/S0140-6736(16)31711-1.
- Veauthier B, Hornecker JR. Crohn's Disease: Diagnosis and Management. Fam Physician, 2018; 98(11): 661-669.
- Aslam F, El-Saiety N, Samee A. Gastrocolic fistula, a rare complication. BJR Case Rep, 2018; 4(4): 20170121. doi: 10.1259/bjrcr.20170121.
- Gourishankar A. Indolent complication after percutaneous endoscopic gastrostomy: a case report of gastric fistula. World J Pediatr Surg, 2020; 3(3): e000202. doi: 10.1136/wjps-2020-000202.

