Association of Superior Mesenteric Artery Syndrome and Lumbar Scoliosis
Assia Mouad1,3,*, Loubna Aqqaoui1,3,4, Rihab Sadqi2,3, Fadoua Boughaleb2,3, Houda Oubejja1,3,4,5,6 and Fouad Ettayebi1,3
1Paediatric Surgical Emergencies Department, Children’s Hospital of Rabat, Morocco
2Faculty of Medecine and Pharmacy, University Mohammed V, Rabat, Morocco
3Laboratory of Genetic and Biometry, Faculty of Science, University Ibn Tofail Kenitra, Morocco
4Laboratory of Epidemiology, Clinical Research and Biostatistics, Faculty of Medicine and Pharmacy, University Mohammed V, Rabat, Morocco
5SIM: Moroccan society of simulation in health care, Morocco
Received Date: 27/06/2024; Published Date: 09/10/2024
*Corresponding author: Assia Mouad, Paediatric Surgical Emergencies Department, Children's Hospital of Rabat, Ibn Sina University Hospital, Mohammed V Faculty of Medicine, Rabat, Morocco
Abstract
Superior Mesenteric Artery Syndrome (SMAS) occurs due to vascular compression of the third portion of the duodenum between the aorta and the superior mesenteric artery. Treatment involves conservative measures such as dietary modifications and gastric aspiration, a surgical intervention considered if symptoms persist. Surgical options include duodenal de-crossing or internal bypass procedures. In our department, the LADD technique is utilized to release duodenal compression without digestive anastomoses
We present the particular case of a patient with aorto-mesenteric syndrome associated with lumbar scoliosis.
Keywords: Superior mesenteric artery syndrome; Lumbar scoliosis; LADD procedure; Children
Introduction
The superior mesenteric artery syndrome, also known as Wilkie's syndrome or mesenteric artery syndrome, is characterized by obstruction in the upper part of the duodenum, specifically at its third portion.
This syndrome develops due to the local anatomical features of the duodenum, which is positioned between the aorta posteriorly and the superior mesenteric artery anteriorly. The superior mesenteric artery forms an acute angle with the aorta, typically between 45° and 60°. When this angle is less than 45°, the D3 portion of the duodenum becomes compressed between the aorta and the superior mesenteric artery, resulting in a presentation of high intestinal obstruction [1].
Case Report
Patient Y. O., a long thin body type14-year-old female, was admitted for bilious vomiting.
Clinical examination revealed signs of dehydration. And the abdominal examination showed a flat, soft abdomen without palpable masses.
The patient underwent the placement of a nasogastric tube and fluid resuscitation,
Additionally, a radiological assessment was carried out including:
• Abdominal X-ray, which revealed a duodenal air-fluid level and the incidental finding of lumbar scoliosis (Figure 1).

Figure 1: abdominal X-ray without contrast (AXR) of the patient showing a duodenal air-fluid level and a lumbar scoliosis.
- Abdominal CT scan revealed significant dilation of the duodenum involving D1 and D2, with D3 being pinched between the aorta and the superior mesenteric artery (Figure 3). The aortomesenteric angle was measured at 18°, and the aorta-superior mesenteric artery distance was measured at 4 mm (Figure 2).
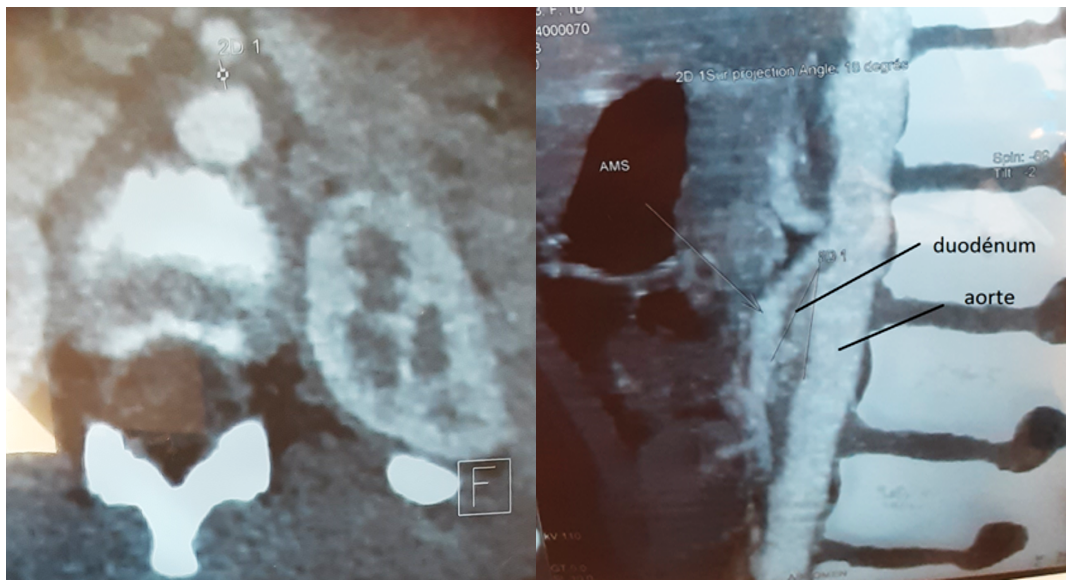
Figure 2: Abdominal CT scan showing an aortomesenteric angle measured at 18°, and an aorta-superior mesenteric artery distance measured at 4 mm.
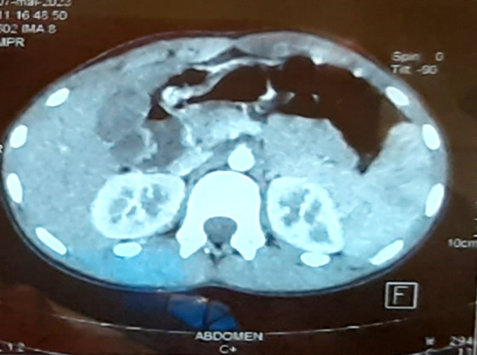
Figure 3: Abdominal CT scan showing D3 being pinched between the aorta and the superior mesenteric artery.
Based on these assessments, the diagnosis of superior mesenteric artery syndrome associated with lumbar scoliosis was established.
Initially, a medical management was pursued, including parenteral nutrition with adequate rehydration and correction of electrolyte imbalances. However, due to the lack of improvement in the patient's condition, surgical intervention was decided (Ladd procedure):
Following a midline laparotomy, the entire colonic frame was released. After releasing the ligament of Treitz, a dilated duodenum upstream of D3, which was pinched between the aorta and the superior mesenteric artery, was identified. The entire duodenum and jejunum were freed, and the digestive tract was repositioned into a complete mesentery (Figure 4), allowing direct continuation of the duodenum with the first loop of the jejunum. Mesenteric defects were closed, and a precautionary appendectomy was performed before closure layer by layer.
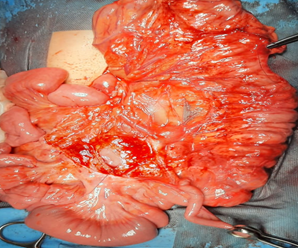
Figure 4: The digestive tract positioned as a complete common mesentery.
Postoperative recovery was uneventful, with good progress, clean wound, improvement in the patient's general condition, and resolution of vomiting.
During the monthly follow-ups, good wound healing was noted with no gastrointestinal disturbances or vomiting, and there was a gradual weight gain.
At the fourth-month follow-up, a complete spine X-ray was requested to measure the Cobb angle, which was 16° (Figure 5). The patient was advised on hygiene and diet measures and started physical therapy sessions.

Figure 5: X-ray showing lumbar scoliosis with 16° Cobb angle.
Discussion
Superior Mesenteric Artery Syndrome (SMAS) is a rare condition first reported by Rokitanski in 1861. In 1927, Wilkie described the pathophysiology and therapeutic options of this syndrome, which was later named Wilkie's syndrome [2].
This syndrome can be caused by various factors such as weight loss, spinal deformities (hyperlordosis), spinal trauma or surgeries, a short ligament of Treitz, or a low origin of the superior mesenteric artery [3].
The duodenum crosses with the aorta at the level of L3 and is held in place between the aorta and the superior mesenteric artery by the ligament of Treitz, originating from the diaphragm. These three elements (duodenum, aorta, and superior mesenteric artery) are surrounded by adipose and lymphatic tissue.
Superior mesenteric artery syndrome is caused by vascular compression of the third portion of the duodenum, resulting from the closure of the angle formed by the aorta and the superior mesenteric artery, hence the term "pinch syndrome" to describe this condition.
Several factors can lead to this syndrome, such as rapid weight loss (associated with mental anorexia, extensive burns, or malabsorption syndrome) that decreases the protective adipose mass around the duodenum, formation of a retroperitoneal hematoma, uterine pregnancy, or surgical correction of spinal deformity by plaster or surgery. Correction of kyphosis is the determining factor that causes closure of the aortomesenteric angle [1].
The syndrome mainly affects young children and adolescents, especially females [4,5].
Clinically, it can manifest either acutely with a picture of duodenal obstruction or chronically in the form of epigastric abdominal pain and vomiting. The most common clinical form is cachexia, characterized by rapid weight loss.
The diagnosis is confirmed if the distance between the aorta and the superior mesenteric artery, evaluated during arterial phase, is less than or equal to 8 mm at the level of CT scan slices passing through the third portion of the duodenum. This criterion has a sensitivity and specificity close to 100%. It is also associated with an aortomesenteric angle of less than 45° [6].
When the reduction in the angle between the aorta and the superior mesenteric artery reaches less than 20 degrees, duodenal compression occurs, leading to obstruction of food passage and resulting in high intestinal obstruction [5].
Several anatomical anomalies can predispose to this condition, such as a hypertrophied or abnormally short ligament of Treitz, which draws the third portion of the duodenum to the left and the apex of the duodenojejunal angle, resulting in compression of the digestive segment by the superior mesenteric artery [2].
Other factors can also play a role, such as severe malnutrition or rapid weight loss, reducing the thickness of adipose tissue in the aortomesenteric space, as can occur in cases of anorexia nervosa or rapid growth without weight gain. Additionally, mesenteric lymphadenopathy, trauma, recent spinal surgery, hyperlordosis, or cerebral palsy have also been suggested as possible factors. Recently, a potential role of genetic factors has been suggested following the description of a mesenteric clamp syndrome in members of the same family [7].
Surgical correction of scoliosis or hyperlordosis has also been reported as predisposing factors for the occurrence of this condition [8].
However, in our particular case, superior mesenteric artery syndrome manifested in our patient without any correction of scoliosis. In fact, the discovery of scoliosis was incidental in our patient during the performance of an abdominal X-ray without contrast as part of the etiological diagnosis of her occlusive syndrome.
In the acute phase, treatment consists of gastric aspiration and correction of electrolyte disturbances. Dietary measures are also essential and include having small, frequent meals, lying on the left side or in a prone position after meals, and possibly parenteral supplementation in cases of malnutrition. These approaches may be sufficient to manage food intolerance and prevent recurrence. If no improvement is observed after three weeks, surgical intervention may be considered. In children, a duodenal de-crossing procedure (Strong's procedure) involves sectioning the ligament of Treitz to lower D4, or an internal bypass such as a duodenojejunostomy may be performed [5,9,10].
In our department, surgical treatment is performed using the LADD technique, which involves freeing the duodenum along with the entire small intestine and right colon and positioning the digestive tract in a complete common mesentery with the small intestine on the right and the colon on the left, thereby releasing the duodenum from its superior mesenteric artery compression.
In our department, we utilize the LADD technique, which involves freeing the duodenum along with the entire small intestine and right colon, and then positioning the digestive tract in a complete common mesentery with the small intestine on the right and the colon on the left. This approach allows for the release of the duodenum from its superior mesenteric artery compression without the need for digestive anastomoses and the associated risk of suture dehiscence.
Conclusion
Superior mesenteric artery syndrome is a rare entity; however, it should be considered in the setting of high intestinal obstruction. Diagnosis is confirmed through abdominal CT scan with contrast injection and ingestion. Early medical treatment is generally sufficient in most cases, while surgery is only considered in cases of initial medical treatment failure
Conflict of interests: The authors have no conflict of interests to declare.
References
- Zadegan F, Lenoir T, Drain O, Dauzac C, Leroux R, Morel E, et al. Superior mesenteric artery syndrome following correction of spinal deformity: case report and review of the literature, 2007; 92110.
- Bonnet JP, Louis D, Foray P. La pince aortomeésenteérique supeérieure primitive. Arch Pediatr, 1995; 2: 333–338.
- Eddeghai S, Krati K, Louzi A. Le syndrome de la pince aorto- meésenteérique : une cause rare de vomissement chronique. Hegel, 2014; 4: 86–91.
- Kalouche I, Leturgie C, Tronc F, Bokobza B, Michot F, Pons P. Le syndrome de la pince meésenteérique. AÀ propos d’une observation et revue de la litteérature. Ann Chir, 1991; 45: 609-662.
- Loeb T, Loubert G, Morsly R, Gabillet JM, Pasteyer J. Syndrome de l’arteère meésenteérique supeérieure. Ann Fr Anesth Reanim, 1999; 18: 1000-1004.
- Nacef K, et al. Service de chirurgie geéneérale, hôpital Taher-Sfar de Mahdia, Tunisie
Le syndrome de la pince aorto-meésenteérique : description du signe de Sœur Marie-Joseèphe Journal d'imagerie diagnostique et interventionnelle, 2018; 1–2. - Ortiz C, Cleveland RH, Blickman JG, Jamarillo D, Kim SH. Familial superior mesenteric artery syndrome. Pediatr Radiol, 1990; 20: 588-589.
- Jellouli O, et al. Syndrome de la pince mésentérique, Feuillets de radiologie, 2015; 55: 386-387.
- Kadji M, Naouri A, Bernard P. Syndrome de la pince aortomeésen- teérique : aà propos d’un cas. Ann Chir, 2006; 131: 389-392.
- Kim IY, Cho NC, Kim DS, Rhoe BS. Laparoscopic duodenojejuno- stomy for management of superior mesenteric artery syndrome: two cases report and a review of the literature. Yonsei Med J, 2003; 44: 526-529.

