Non-Operative Treatment of Pancreatic Hydatid Cyst in Children
Assia Mouad1,2,*, Loubna Aqqaoui1,2,3, Fadoua Boughaleb1,2, Houda Oubejja1,2,3,4,5 and Fouad Ettayebi1,2
1Paediatric Surgical Emergencies Department, Children’s Hospital of Rabat, Morocco
2Faculty of Medecine and Pharmacy, University Mohammed V, Rabat, Morocco
3Laboratory of Genetic and Biometry, Faculty of Science, University Ibn Tofail Kenitra, Morocco
4Laboratory of Epidemiology, Clinical Research and Biostatistics, Faculty of Medicine and Pharmacy, University Mohammed V, Rabat, Morocco
5SIM: Moroccan society of simulation in health care, Morocco
Received Date: 27/06/2024; Published Date: 09/10/2024
*Corresponding author: Assia Mouad, Paediatric Surgical Emergencies Department, Children's Hospital of Rabat, Ibn Sina University Hospital, Mohammed V Faculty of Medicine, Rabat, Morocco
Abstract
Pancreatic hydatid cysts are rare, accounting for less than 2% of cases, and diagnosis can be challenging due to overlapping imaging characteristics. Surgical intervention has historically been the mainstay of treatment, but non-surgical methods, including albendazole therapy, have emerged as effective alternatives.
We present the case of a pancreatic hydatid cyst in a patient who was medically treated.
Keywords: Non-operative treatment; Pancreas; Hydatic cyst; Children
Introduction
Pancreatic hydatid cysts are infrequent, constituting just 1% of all hydatid cysts and exceptionally rare in pediatric cases. The scarcity of occurrences in children might contribute to challenges in diagnosing this condition [1-2].
We present a case involving a 11-year-old child with a pancreatic hydatid cyst treated by nonsurgical treatment.
Case Report
An 11-year-old female admitted for abdominal pain. She lived in a rural area with exposure to dogs.
Clinically, the patient was non-icteric and the abdominal examination revealed tenderness in the epigastric area without a palpable mass.
She was managed with fluid resuscitation, and analgesics.
Abdominal ultrasound revealed a well-defined, round mass measuring 76x69 mm at the tail of the pancreas, suggestive of a hydatid cyst (Figure 1). Hydatid serology was positive (201 UI/ml), confirming a pancreatic hydatid cyst of the tail.
Conservative treatment included digestive rest with a basic diet, analgesics, and 12 mg/kg/day albendazole (after liver function tests before and after treatment).
Albendazole was administered for 3 months with therapeutic breaks of 15 days after each month. Follow-up included monthly evaluations for 4 months, then every 3 months for 1 year. Clinical exams showed no pain or jaundice, normal liver enzymes, negative hydatid serology, and ultrasounds demonstrated gradual reduction in cyst size to 38x33 mm with calcification on the last examination (Figure 2).

Figure 1: Abdominal ultrasound of the patient showing a hydatid cyst in the tail of the pancreas.
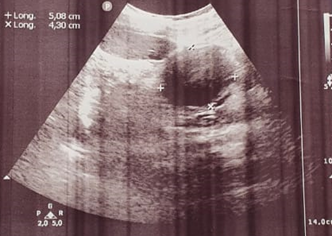
Figure 2: Abdominal ultrasound after 8 months follow-up showing the calcification of the cyst and the reduction of its size.
Discussion
Echinococcosis is a widespread parasitic disease found in regions surrounding the Mediterranean, Asia, South America, and Oceania [3,4].
Parasitic embryos typically traverse the liver after intestinal migration, with most becoming trapped there or moving on to the lungs or other body parts, making the liver and lungs the most commonly affected organs [5]. Pancreatic hydatid cysts are rare, accounting for less than 2% of cases [6,7]. Diagnosing these cysts before surgery is challenging due to their rarity and overlapping imaging characteristics. The resemblance of a hydatid cyst in the pancreatic head of the cyst tumor (which remains very rare in children) adds to the complexity of management. This study details our experience with a case involving a hydatid cyst in the pancreas.
The main symptoms found in the literature are abdominal pain, jaundice and the presence of an abdominal mass [8,9]. In our patient the pain was the main symptom.
Most documented cases of pancreatic hydatid cysts in English literature have typically resulted in surgical intervention. Cystectomy stands out as the most frequently reported operative procedure. In most instances, surgery was initially planned without a preoperative diagnosis of a hydatid cyst. However, during the surgical procedure, the laminated membrane was observed, and after puncturing the fluid and administering various scolicidal agents like cetrimide, hypertonic saline, H2O2, ethanol, or formaldehyde, the cyst was unroofed and removed. Some cases also involved omentoplasty. Additionally, in situations where the hydatid cyst was connected to the main pancreatic ducts or was of significant size, procedures such as distal pancreatectomy with or without splenectomy were performed. For hydatid cysts located in the pancreatic head, reported procedures included pancreaticoduodenectomy or cyst excision followed by Roux-en-Y reconstruction [10].
Certain authors have asserted that there was no risk of spillage, hence they opted against the use of scolicidal agents [11]. Another documented procedure involves central pancreatectomy, a method utilized for various pancreatic lesions, including cases of pancreatic hydatid cysts [12].
The conventional approach for treating hydatid cysts has involved surgical resection. Over the past decade, non-surgical methods for addressing hydatid disease have emerged, notably the introduction of albendazole into treatment protocols. This medication is now considered a primary treatment or used alongside surgery for managing hydatid cysts.
In our case, we have chosen the nonsurgical approach that gives comparable results to surgery without patients having to undergo the risks of surgery
Extending the duration of treatment improves the probability of cure, but there is a risk of an increase in undesirable effects such as cytolysis, which is not very severe with this therapy [12].
Conclusion
Non-operative medical treatment of pancreatic hydatid cyst in children offers an effective therapeutic alternative, less invasive than surgical approach with few side effects.
Conflict of interests: The authors have no conflict of interests to declare.
References
- Wani RA, Malik A, Chowdri N, et al. Primary extrahepatic abdominal hydatidosis. Int J Surg, 2005; 3(2): 125-127.
- Abi F, El Fares F, Khaiz D, et al. Les localisations inhabituelles du kyste hydatique : a propos de 40 cas. J Chir (Paris), 1989; 126(5): 307-312.
- Brown RA, Millar AJ, Steiner Z, Krige JE, Burkimsher D, Cywes S. Hydatid cyst of the pancreas. A case report in a child. Eu J Pediatr Surg, 1995; 5: 121-123.
- Safioleas M, Misiakos E, Manti C, Katsikas D, Skalkeas G. Diagnostic evaluation and surgical management of hydatid disease of the liver. World J Surg, 1994; 18: 859-865.
- Safioleas M, Misiakos EP, Dosios T, Manti C, Lambrou P, Skalkeas G. Surgical treatment for lung hydatid disease. World J Surg, 1999; 23: 1181-1185.
- Hamamci EO, Besim H, Korkmaz A. Unusual locations of the hydatid disease and surgical approach. ANZ J Surg, 2004; 74: 356-360.
- Ozmen MM, Moran M, Karakahya M, Coskun F. Recurrent acute pancreatitis due to a hydatid cyst of the pancreatic head: a case report and review of the literature. JOP. J Pancreas (Online), 2005; 6: 354-358.
- Yattoo GN, Khuroo MS, Zargar SA, Bhat FA, Sofi BA. Percutaneous drainage of the pancreatic cyst. Case Report: Percutaneous drainage of pancreatic head cyst with obstructive jaundice. J Gastroenterol and Hepatol, 1999; 14: 931-934.
- Krige JEJ, Mirza K, Bornman PC. Primary hydatid cysts of the pancreas. SAJD 2005; 43:37-40. /Diego T, Gonzalo C, Carlos ST, Gaston M, Fabian C, Paul EL, et al. Primary hydatid of the pancreas. Rev Fac Cien Med Univ Nac Cordoba, 2017; 74: 33-36.
- Pancreatic Hydatid Cyst: A Clinicopathologic Review. Bita Geramizadeh. JOP. J Pancreas (Online), 2018; 19(4): 171-177.
- Varshney M, Shahid M, Maheshuari V, Siddiqui MA, Alam K, Mubeen A, et al. Hydatid cyst in tail of pancreas. BMJ Case Reports, 2011.
- Adham M, Guinippero A, Hervierru V, Courbiere M, Partensky C. Central pancreatectomy (Single center experience of 50 cases). Arch Surg, 2008; 143:175-180.

