Multiple Brain Abscesses Caused by Citrobacter Koseri in a 3-Month-Old Child
Aditya Rai1 and Ashwin Rai2,*
1Sri Lakshmi Narayan Institute of Medical Sciences (SLIMS), Puducherry, India
2Department of Neurosurgery, Jawaharlal Institute of Post-graduate Medical Education and Research (JIPMER), Puducherry, India
Received Date: 23/06/2024; Published Date: 08/10/2024
*Corresponding author: Ashwin Rai, Department of Neurosurgery, Jawaharlal Institute of Post-graduate Medical Education and Research (JIPMER), Puducherry, India
Abstract
Citrobacter koseri is a gram-negative, rod-shaped bacteria. It is a facultative anaerobe and is present in human and animal digestive tracts as a commensal organism. It may act as an opportunistic pathogen in immunocompromised individuals. However, rarely it can cause neurological infections particularly ventriculitis, meningitis or brain abscesses in neonates and infants. We describe a rare case of multiple brain abscesses in a 3-month-old child caused by an acute Citrobacter koseri infection. We have described the patient’s history, presenting signs and symptoms, evaluation of the pathology and its management leading to the convalescence of the infection and significant neurological improvement. The case report will go into detail regarding the specific neurological deficiencies associated with the infection and the brain abscesses along with the course of the management which included a full neurological workup with Computed Tomography (CT) imaging along with the surgical procedure and aggressive antimicrobial therapy with supportive measures.
Keywords: Multiple brain abscesses; Citrobacter koseri; Suspected teratoma; Neurosurgery; Case Report
Case Report
Citrobacter koseri is a commensal gram-negative, rod-shaped, facultative anaerobic bacterium which can be found in the digestive tracts of humans and animals. It is a rare infection and usually affects neonates or young infants. Neonates acquire the bacteria via vertical transmission from the mother at the time of delivery or horizontally as nosocomial infections. CNS infections are most common along with occasional cases or neonatal sepsis and bacteraemia. The strongest predilection for infection is in the first 2 months of life as most of the cases occur during this time [1]. Meningitis caused by Citrobacter koseri is particularly dangerous as it leads to brain abscesses in 75% of the cases, along with complications like ventriculitis, cerebral oedema, cerebritis, empyema, diffuse necrotising meningoencephalitis and cerebral infarction hydrocephalus [2]. The mortality rate for meningitis due to Citrobacter koseri is 30% and out of the survivors around 80% have some degree of intellectual disability [3]. The commonly seen signs and symptoms of Citrobacter meningitis and abscesses are raised fontanelle, rapidly increasing head circumference and wide cranial sutures [2]. Citrobacter koseri has a propensity to affect the meninges which is hypothesized to be because of a unique 32-kD outer membrane protein that provides tropism to the bacteria specific to the CNS [4].
Brain abscesses have 4 stages of development. Early cerebritis is occurs from the 1st to the 4th days. Late cerebritis is from the 4th to the 10th day. After that capsule formation starts occurring. Early capsule formation from day 11 to day 14 and late capsule formation occurs after 14 days [5]. Formation of the capsule reduces antibiotic uptake and action.
History and Examination
A 3-month-old male child, with normal development, presented to paediatric emergency with complaints of fever for 2 days which was high grade and intermittent. The child also had an episode of abnormal cyclic movements of his left upper limb lasting for 5 minutes which aborted spontaneously and there was no post ictal lethargy/sleepiness. The child had 2 episodes vomiting in the past 2 days in addition to poor feeding.
The child had one prior hospitalization in the past. On day 5 of life, the child was admitted to the general hospital for high grade fever, right focal seizure with uprolling of eyes. The blood culture grew MRSA and the child was treated successfully with antibiotics.
At arrival patient’s temperature was 100°F, had tachycardia of 142/minute, BP of 90/52 mmHg and respiratory rate of 45/minute. A physical evaluation revealed a poorly compliant and uncooperative child with no abnormal movements of the limbs. Central Nervous System (CNS) examination revealed spontaneous movements on right upper and lower limb with reduced movements in the left upper and lower limb indicating left hemiparesis. The Medical Research Council (MRC) score was 5/5 on the right side and 3/5 on the left side. Paediatric GCS examination showed that the eyes were opening to loud noises, the child was crying inappropriately and screaming, and all the limbs were moving spontaneously. This showed a paediatric GCS of E3V3M6. The anterior fontanelle was bulging, suggestive of increased intracranial pressure.
Evaluation and Treatment
The child was admitted on the basis of the above-mentioned signs and symptoms. Appropriate investigations were ordered. Total blood count revealed mild normocytic anemia with a WBC count in the normal range. Differential leucocyte count showed no abnormalities. Platelet count was slightly increased. Procalcitonin levels were within normal range. CT scan was done soon after which confirmed the diagnosis. The CT showed multiple brain abscesses in the right frontotemporal region with a midline shift and mass effect.
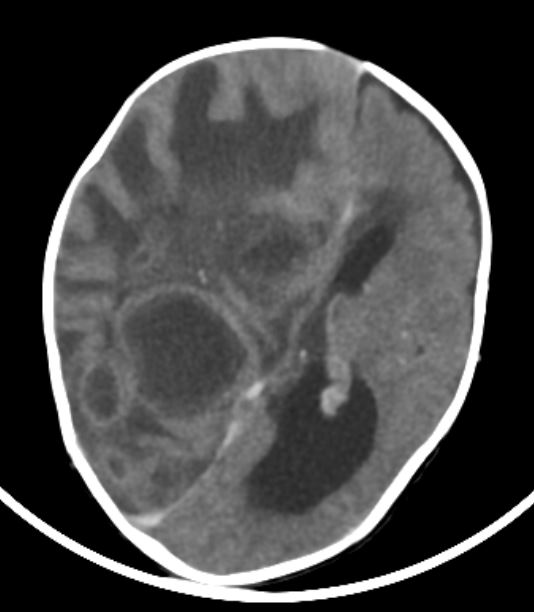
Figure 1: Pre-Operative CT brain at the level of lateral ventricle, showing multiple deep seated abscesses of varying sizes in right fronto-parietal region, the largest measuring 3x4 cm with multiple smaller satellite abscesses. Diffuse white matter edema with mass effect also seen.
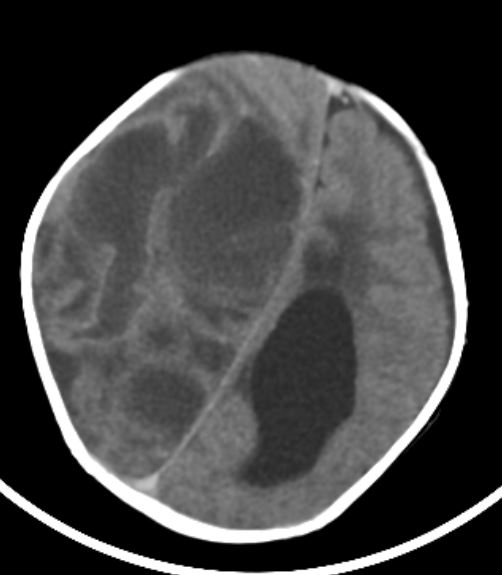
Figure 2: Pre-Operative CT brain at high parietal section, showing the extension of the abscess and white matter edema in the higher cuts. Bulging anterior fontanelle also seen.
In view of fronto parietal abscesses with mass effect (Figures 1, 2), patient underwent right fronto parietal craniotomy with drainage of abscess and excision of abscess capsule. 30-40 mL of yellowish-green pus was drained from the abscess and sent for investigations. The excised abscess capsule was sent for histopathological examination. Abscess cavity was thoroughly washed with gentamicin saline. After abscess evacuation, the brain edema reduced significantly and dura was closed in a lax fashion and bone flap was replaced back.

Figure 3: Post-operative CT at the level of lateral ventricle showing adequate drainage of abscess and reduced white matter edema and mass effect. A deep-seated residual abscess is also seen.
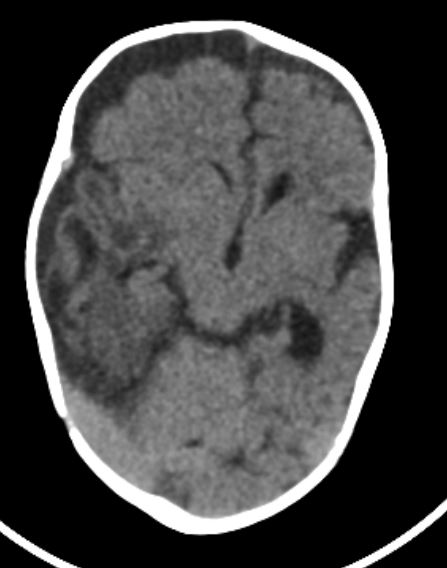
Figure 4: Post-operative CT at midbrain level showing reduction in white matter edema and mass effect.
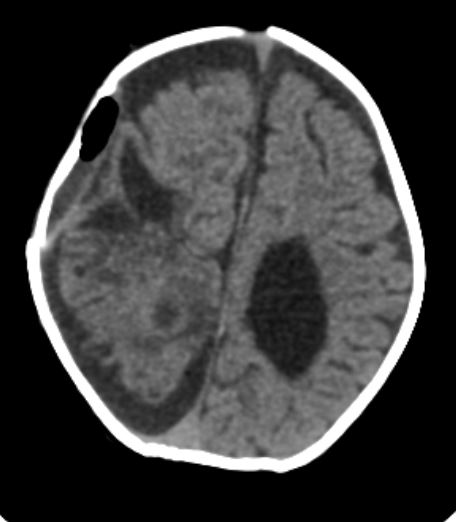
Figure 5: Post-operative CT brain at high parietal section, showing adequate drainage of abscess and reduced white matter edema and mass effect. The anterior fontanelle is lax.
Post-operative CT (Figures 3, 4, 5) showed adequate abscess drainage with reduction in white matter edema and mass effect. Biopsy of the excised tissue showed no signs of granuloma, giant cells or necrosis however it did show features of chronic inflammation. Periodic acid Schiff on the pus sample did not highlight any fungal elements. Ziehl-Neelsen staining, liquid culture and GeneXpert test for Mycobacterium tuberculosis were also negative. Gram staining of the pus showed gram negative bacilli and the pus culture isolated Citrobacter koseri. The pus culture also showed antibiotic sensitivity to Meropenem, Amikacin, Cefoperazon/Sulbactam, Ceftriaxone, Ciprofloxacin, and Piperacillin Tazobactum. The deep seated abscess in the right parieto-occipital region (Figure 3) was treated with sensitive antibiotics as the capsule wall was partially excised to facilitate the action of antibiotics.
Course of Illness and Outcome
On day 1 of admission, the child was started on Cefotaxime IV, metronidazole IV and Vancomycin IV empirically. On Post-operative day 1, child was started on nasogastric feeds which was tolerated well. Sedation was stopped and child was extubated to room air. Post extubation, the respiratory rate was 38 breaths/minute, heart rate was 123 beats/minute, blood pressure was 95/52 mmHg and SpO2 was 99% on room air. A PICC line was inserted in view of need for prolonged duration of antibiotics. Upon receiving pus culture and sensitivity reports, the antibiotic regimen was changed to Meropenem and continued for 14 days. By Post-operative day 3, the scalp darin was removed, the child was accepting direct breast feeding and the sensorium was normal. Over the next few days, neurological evaluation showed that hemiparesis had improved on the left side from MRC 3/5 to 5/5. The child showed spontaneous eye opening, was cooing and crying, and moving all 4 limbs spontaneously resulting in an improvement in the Paediatric GCS to E4V5M6. On Post-operative day 20, the child was discharged with instructions for the parents to watch out for danger signs and a regular follow up schedule to assess the neurological status.
Discussion
The larger abscesses were all excised and drained however, the deep-seated abscess was not amenable to complete excision due to its close proximity with the ventricle and the midbrain, hence partial excision of only the lateral part of the capsule was done to facilitate treatment by antibiotics. Any attempt to excise the medial wall of the deep-seated abscess would have drastically increased the chances of ventriculitis and sepsis. Antibiotic therapy in the case of Citrobacter koseri infection should be very aggressive because of the increased risk of long-term neurological sequelae compared to meningitis or abscesses caused by other organisms [6]. In addition to that if Citrobacter koseri causes systemic infection or meningitis, Ciprofloxacin and Meropenem can be considered for treatment [7]. Medical management of brain abscesses is also dependent on various factors. Medical management can be successful by itself if treatment is begun in early cerebritis stage before the encapsulation process can be completed or in case the diameter of the abscesses is small. Usually, the mean size for cutoff is considered to be 3 cm. In most cases, medical management alone is not preferred and surgical treatment is vital as the abscesses commonly show significant mass effect, increase intracranial pressure, cause poor neurological conditions, or show close proximity to ventricles increasing the likelihood of interventricular septum rupture. These are a few of the emergent conditions that strongly indicate a need for surgical management. A combination of timely surgical management along with aggressive antibiotic therapy is the best course of action in treating Citrobacter koseri brain abscess and reducing the possibility of long-term neurological complications.
Conclusion
In conclusion, brain abscess can present with acute or rapid onset neurological deficit and should be treated promptly with surgical drainage of the abscess, via burr hole or craniotomy, along with organism specific antibiotics with intensive care and support.
Conflict of Interest Statement: Dr Ashwin Rai has been working as a Senior Resident in the Department of Neurosurgery at JIPMER for the last 3 years. Dr Aditya Rai has recently graduated from SLIMS. The authors have no conflicts of interest to declare.
Funding Sources: No funding was required for the production of this manuscript.
Author Contributions: Dr Ashwin Rai contributed towards conceptualizing the manuscript and gathering the data. Dr Aditya Rai and Dr Ashwin Rai both contributed towards compiling, writing and editing the manuscript.
Patient Informed Consent: The necessary patient informed consent was obtained in this case.
References
- Terence I Doran. The Role of Citrobacter in Clinical Disease of Children: Review, Clinical Infectious Diseases, 1999; 28(2): Pages 384–394, https://doi.org/10.1086/515106.
- Marecos CV, Ferreira M, Ferreira MM, et al. Sepsis, meningitis and cerebral abscesses caused by Citrobacter koseri Case Reports, 2012; 2012: bcr1020114941.
- McPherson C, Gal P, Ransom JL. Treatment of Citrobacter koseri infection with ciprofloxacin and cefotaxime in a preterm infant. Ann Pharmacother, 2008; 42(7): 1134-1138. doi: 10.1345/aph.1L008.
- Li J, Musser JM, Beltran P, Kline MW, Selander RK. Genotypic heterogeneity of strains of Citrobacter diversus expressing a 32-kilodalton outer membrane protein associated with neonatal meningitis. J Clin Microbiol, 1990; 28(8): 1760-1765. doi: 10.1128/jcm.28.8.1760-1765.1990.
- Dattatraya Muzumdar, Sukhdeep Jhawar, Goel A. Brain abscess: An overview, International Journal of Surgery, 2011; 9(2): Pages 136-144. https://doi.org/10.1016/j.ijsu.2010.11.005.
- Rodrigues J, Rocha D, Santos F, João A. Neonatal Citrobacter koseri Meningitis: Report of Four Cases. Case Rep Pediatr, 2014; 2014: 195204. doi: 10.1155/2014/195204.
- McPherson C, Gal P, Ransom JL. Treatment of Citrobacter kosen Infection with Ciprofloxacin and Cefotaxime in a Preterm Infant. Annals of Pharmacotherapy, 2008; 42(7-8): 1134-1138. doi:10.1345/aph.1L008.

