A Never-Ending Obstruction: Recurrent Small Bowel Obstruction in a Patient with Adhesions
Yesenia Brito1,*, Jonathan Valdivia1, Ana I Gonzalez1, Henry C Valdivia1, Juaquito Jorge2 and Frederick Tiesenga3
1Saint George’s University School of Medicine, Grenada
2General and Bariatric Surgery, Tiesenga Surgical Associates, Elmwood Park, USA
3General Surgery, West Suburban Medical Center, Chicago, USA
Received Date: 15/06/2024; Published Date: 04/10/2024
*Corresponding author: Yesenia Brito, Saint George’s University School of Medicine, Grenada
Abstract
Small bowel Obstruction (SBO) is a common surgical emergency due to a blockage in the small intestine, preventing liquids and solids from passing through. It can be caused by various factors like adhesions, tumors, hernia, and inflammation. Treatment of SBO can vary from supportive care, such as bowel rest, intravenous fluids, nasogastric decompression, and pain management, to surgical interventions. Exploratory Laparotomy/ laparoscopic is the most common surgical approach for SBO. During this intervention, the surgeon makes an abdominal incision and examines the intestines to identify the source of the obstruction. Prompt medical attention is encouraged, as SBO can be serious and potentially life-threatening if left untreated.
In this case report, we discuss a 39-year-old man who shows the classical clinical complaint of small bowel obstruction, including abdominal pain and distention. The patient’s past medical history includes multiple occurrences of SBO after multiple surgeries that make recurrence likely. The Patient’s symptoms were acutely managed with intravenous fluids, bowel rest, nasogastric tube, and acetaminophen-codeine. He underwent exploratory laparotomy, adhesiolysis, and enteroenterostomy to rectify the obstruction. We expound and emphasize on the vigilance needed to quickly detect and operate on patients with a high likelihood of small bowel obstruction.
Categories: General Surgery; Gastroenterology; Radiology
Keywords: SBO; Adhesions; Abdominal pain; Obstruction
Introduction
Small Bowel Obstruction (SBO) hinders standard passage through the bowel. The cause can be either mechanical or functional bowel obstruction [1]. Mechanical obstruction is due to a structural barrier such as a tumor, hernia, or adhesions. Functional bowel obstruction results from impairment of peristalsis, such as a paralytic ileus [1]. Total SBO involves obstipation, while partial SBO allows a limited amount of air and fluid to pass [2]. The obstruction's presentation occurs with various acute or chronic symptoms, substantially reducing the quality of life and may cause death. Therefore, SBO requires prompt diagnosis to avoid the stated predicaments [3].
SBO is a pathophysiology that entails stasis of luminal contents and gas proximal to the obstruction, leading to increased intraluminal pressures. As a result, gaseous abdominal distention, vomiting, and compression of intestinal veins and lymphatics lead to severe metabolic acidosis and necrosis [4]. Patients with SBO typically present with abdominal pain, constipation, diarrhea, and decreased bowel sounds. Diagnostic imaging is needed to locate the site and assess the obstruction's etiology and complication, aided by laboratory studies such as complete blood count, basic metabolic panel, serum lactate, and C-reactive protein [5]. Stable patients with SBO can undergo abdomen and pelvis computer tomography (CT) with intravenous contrast. Unstable patients can undergo ultrasound or X-ray. Additionally, both need urgent surgical consultation [6]. It is vital to act swiftly to avoid further complications such as bowel perforation or ischemia.
The management of SBO depends on the severity of symptoms and the patient's overall condition. Conservative management calls for bowel rest, intravenous liquids, and nasal decompression [7]. In total SBO, which tends to be more severe, laparotomy and laparoscopy are necessary for definitive treatment [7]. Therefore, to prevent complications and ensure a successful recovery, effective postoperative care and monitoring are essential [7].
Case Presentation
We present a 39-year-old male patient who came to the emergency department (ED) with severe right-sided abdominal pain. The pain started three days prior to his visit and was described as progressive and cramping. Associated symptoms include nausea, yellowish emesis, and a small and hard bowel movement. He previously had multiple bowel obstructions that resolved spontaneously, although nasogastric (NG) tube decompression was required on some occasions. The patient's past medical history is significant for exploratory laparotomy for a gunshot wound eighteen years ago, small bowel obstruction repair seventeen years ago, and inguinal hernia repair eight months ago. The patient denied dizziness, fever, chest pain, and shortness of breath.
On examination, vital signs were within normal limits. The patient was alert, cooperative, and in no acute distress. A well-healed midline abdominal laparotomy scar was perceived. The abdomen was mildly distended, with tenderness to palpation, no guarding, masses, or organomegaly. CBC showed mild leukocytosis of 15 without any other significant abnormalities. A CT scan of the abdomen showed dilated loops of small bowel (Figure 1), concerning for small bowel obstruction.
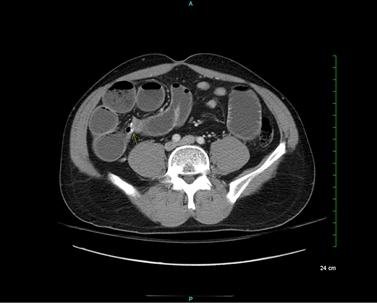
Figure 1: Transition point on the right hemiabdomen (yellow arrow).
The general surgical team was consulted, which ordered an NG tube and a small bowel follow-through (SBFT). The SBFT findings confirmed small bowel obstruction by demonstrating no colonic contrast on five-hour delayed imaging (Figure 2).
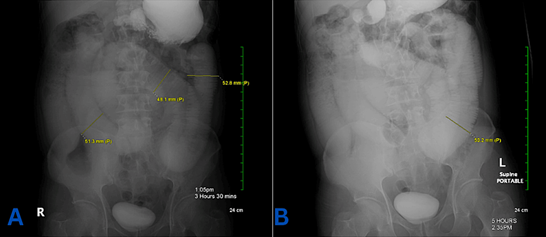
Figure 2: Small bowel obstruction. (A) Diffuse small intestine dilatation. (B) No colonic contract at hour five.
The patient was taken to the operating room (OR), where he underwent an exploratory laparoscopy with adhesiolysis and enteroenterostomy. Upon entering the peritoneal cavity, many adhesions were encountered and lysed. A dilated small bowel transitioning to a completely collapsed small bowel was also visualized. Upon examination of the anastomosis, it was found to have a very small diameter, not allowing any fluid to pass through. A new anastomosis was performed. The bowel was returned to the peritoneal cavity, antibiotic irrigation was applied, and a JP drain was left in the abdomen.
The pathology report displayed focal chronic inflammation, vascular congestion, and reactive changes (Figure 3). No signs of dysplasia or malignancy were reported.
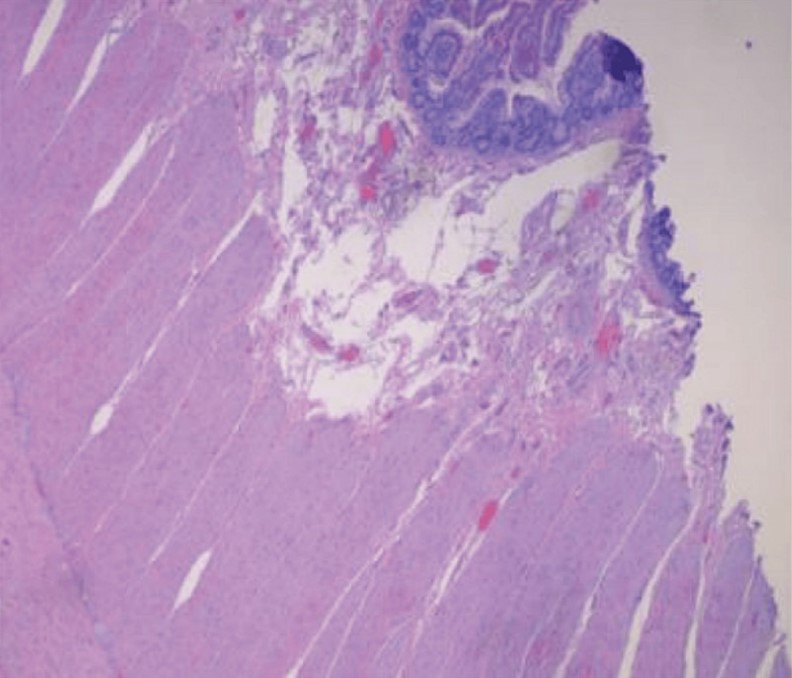
Figure 3: Segment of small bowel tissue with chronic inflammation and vascular congestion.
The patient’s postoperative course was uneventful. On postoperative day three, diet was advanced to clear liquids, and was well tolerated. He denied any nausea, emesis, fever, abdominal pain or any other symptoms similar to the ones he experienced preoperative.
Discussion
A Small bowel obstruction is a common condition that accounts for approximately 20% of all hospital admissions for abdominal pain [8]. The etiology of SBO is multifactorial, involving both intrinsic and extrinsic factors [9]. The principal intrinsic cause of SBO is intussusception, while the primary extrinsic causes are adhesions and hernias [9]. Intra-abdominal adhesions account for approximately 75% of SBO cases [9]. Adhesions occur as a consequence of previous surgery [9].
Constipation, nausea, vomiting, bloating, and abdominal pain are the most common symptoms in patients with SBO [6]. The abdominal pain is usually crampy, intermittent, and located in the central or lower abdomen [6]. Patients may also experience distension of the abdomen with an increase in girth and discomfort. SBO may be associated with a complete obstruction, leading to the absence of bowel movements, dehydration, and electrolyte imbalances [6]. The severity of the symptoms depends on the extent and duration of the obstruction, as well as the underlying cause [6].
While conservative management is often the first line of treatment, this approach is often insufficient as there is a high risk for SBO recurrence [10]. Conservative management for SBO includes bowel rest, fluid resuscitation, nasogastric tube placement for abdominal decompression, correcting electrolyte imbalance, and regular bowel monitoring [11]. Although recurrent SBO is more prevalent in the older population, it can also present in relatively young people [12]. It has been reported that recurrence rates in affected patients are approximately 20% [12]. The recurrence rate of SBO following surgery may be influenced by the type of adhesions present [13]. Specifically, the presence of diffuse adhesions appears to be associated with a greater likelihood of recurrence compared to the presence of single-band adhesions [13]. Lorentzen et al. demonstrated a recurrence rate of 12% among their study participants over 2.2 years of follow-up. They reported that multiple/matted adhesions (P = 0.046) and fascial dehiscence (P = 0.009) were associated with an increased risk of recurrence [14]. Patients who suffer from such instances are frequently afflicted with underlying conditions like adenocarcinoma [15]. These patients are more vulnerable to severe SBO, which can increase mortality [15].
SBO complications can be serious and even life-threatening if left untreated. One potential complication is bowel ischemia, which occurs when there is a lack of blood supply to the bowel, leading to tissue damage and potentially necrosis [8]. Additionally, SBO can lead to bowel perforation, which can cause peritonitis and sepsis [8]. In some cases, SBO may also lead to dehydration, electrolyte imbalances, and renal failure [8]. If left untreated, these complications can worsen and ultimately result in death. Therefore, promptly diagnosing and managing SBO is crucial to prevent these potential complications.
This case report describes a young male with a history of exploratory laparotomy following a gunshot wound, small bowel obstruction, and inguinal hernia repair. As stated above, patients with prior laparotomy are more likely to develop SBO, but the evidence of such recurrence in patients without comorbid conditions needs to be further examined [12]. Despite age and comorbid conditions, patients with a history of intra-abdominal operations or trauma should receive immediate diagnosis and surgical treatment if they present with symptoms of intestinal obstruction. Moreover, it is imperative that these patients are closely monitored and followed up in order to prevent recurrences and complications of SBO.
It is essential for clinicians to be aware of the possibility of rare presentations of SBO. This case will enrich clinical practice and management of SBO. It highlights the significance of prompt diagnosis and treatment, irrespective of a patient's age or medical history. This will lead to a better management of recurrent SBO in the future. We recommend exercising caution in patients with a history of previous SBO and monitoring them frequently in the outpatient clinic. Consequently, persistent SBO and its complications could be prevented or detected early. Prophylactic measures, such as early mobilization and the use of adhesion barriers, may reduce the incidence of postoperative adhesion-related SOB. Seprafilm, a type of adhesion barrier, has been shown to significantly lower the incidence of adhesive small-bowel obstruction requiring reoperation compared to no-treatment patients: 1.8 percent versus 3.4 percent (P < 0.05) [16]. This finding represents an absolute reduction in adhesive small-bowel obstruction requiring reoperation of 1.6 percent and a relative reduction of 47 percent [16]. A multidisciplinary approach involving close monitoring, early diagnosis, and individualized treatment plans is necessary for optimal SBO outcomes.
Conclusion
Small Bowel Obstruction (SBO) continues to be a major clinical concern in the United States. When treating SBO, it is crucial to understand the etiology, pathophysiology, as well as patient’s history to tailor a successful treatment outcome. NG tube for bowel decompression, intravenous fluid hydration, and adequate pain control are standardized approaches for treating SBO. In the case of a complicated obstruction, the patient will need to undergo emergent surgery.
Our patient presented with a classic case of SBO. This is an example of clinical victory in the management of recurrent SBO. His bowel function was restored to optimal function as a result of timely and effective management, thus preventing further complications. SBO is a common and primary clinical issue nevertheless, with the right and timely approach, there is hope for a successful clinical outcome.
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case.
Competing Interests: None
Grant Information: None
Author Contributions:
Yesenia Brito: Concept and design of study, acquisition of data, drafting article, revising article. Guarantor Author.
Jonathan Valdivia: Concept and Design of study, drafting article intellectual content, revising article.
Ana I Gonzalez: Acquisition of data, drafting article, revising article.
Henry C Valdivia: Acquisition of data, drafting article, revising article.
Frederick Tiesenga and Juaquito Jorge: Final Approval, Intellectual Content, revising article
References
- Griffiths S, Glancy DG. Intestinal obstruction. Surgery, 2016; 35: 3. 1016/j.mpsur.2016.12.005.
- Rami Reddy SR, Cappell MS. A Systematic Review of the Clinical Presentation, Diagnosis, and Treatment of Small Bowel Obstruction. Curr Gastroenterol Rep, 2017; 19: 28. 1007/s11894-017-0566-9
- De U. Small bowel obstruction Clin Colon Rectal Surg, 2020; 33: 175-181. 1055/s-0040-1712947
- Fevang BT, Fevang J, Stangeland L, Soreide O, Svanes K, Viste A. Complications and deaths after surgical treatment for small bowel obstructions: A 35-year institution experience. Ann Surg, 2000; 231: 529-537. 1097/00000658-200004000-00012
- Hayden GE, Sprouse KL. Bowel Obstruction and Hernia. Emerg Med Clin North Am, 2011; 29: 319-345. 1016/j.emc.2011.01.004
- Maglinte DD, Kelvin FM, Fitzgerald EF, et al. Acute small bowel obstruction: comparison of CT and Barium studies. Radiology, 1997; 205: 721-726. 1148/radiology.205.3.9393541
- Di Saverio S, Coccolini F, Galati M, et al. Bologna Guidelines for Diagnosis and Management of Adhesive Small Bowel Obstruction (ASBO): 2017 Update of the Evidence-Based Guidelines from the World Society of Emergency Surgery ASBO Working Group. World J Emerg Surgery, 2018; 13: 24. 1186/s13017-018-0188-4
- Delabrousse E, Lubrano J, Sailley N, Aubry S, Mantion GA, Kastler BA. Small-Bowel Obstruction from Adhesive Bands and Matted Adhesions: CT Differentiation. American Journal of Roentgenology, 2009; 192(3): 693-697. 2214/AJR.08.1550
- Mullan CP, Siewert B, Eisenberg RL. Small bowel obstruction. AJR Am J Roentgenol, 2012; 198: 105-117. 2214/ajr.10.4998
- Markogiannakis H, Messaris E, Dardamanis D, et al. Acute mechanical bowel obstruction: clinical presentation, etiology, management and outcome. World J Gastroenterol, 2007; 13(3): 432-437. 3748/wjg.v13.i3.432
- Hwabejire JO, Tran DD, Fullum TM. Non-operative management of adhesive small bowel obstruction: Should there be a time limit after which surgery is performed? American Journal of Surgery, 2018; 215: 1068-1070. 1016/j.amjsurg.2018.03.010
- Foster NM, McGory ML, Zingmond DS, Ko CY. Small bowel obstruction: a population-based appraisal. J Am Coll Surg, 2006; 203: 170-176. 1016/j.jamcollsurg.2006.04.020
- Sakari T, Christersson M, Karlbom U. Mechanisms of adhesive small bowel obstruction and outcome of surgery; a population-based study. BMC Surgery, 2020; 20: 62. 1186/s12893-020-00724-9
- Lorentzen L, Øines MN, Oma E, Jensen KK, Jorgensen LN. Recurrence After Operative Treatment of Adhesive Small-Bowel Obstruction. Journal of Gastrointestinal Surgery, 2018; 22: 329-334. 1007/s11605-017-3604-x
- Fleites O, Pelenyi SS, Lee CK, et alPersistent Small Bowel Obstruction due to Small Bowel Adenocarcinoma: A Case Report. Cureus, 2021; 13: 20233. 7759/cureus.20233
- Fazio VW, Cohen Z, Fleshman JW, et al. Reduction in Adhesive Small-Bowel Obstruction by Seprafilm® Adhesion Barrier After Intestinal Resection. Diseases of the Colon & Rectum, 2006; 49(1). 10.1007/s10350-005-0268-5

