Percutaneous Endovascular Therapy of Blunt Trauma Related Renal Artery Thrombosis: A Case Report
Yen-Wei Chen1,2, Chao-Wen Chen3, Nai-Yu Chi1,2, Ching-Tang Chang1,2, Tzu-Chieh Lin1,2, Tsung-Han Lin1,2, Tsung-Hsien Lin1,2,4 and Po-Chao Hsu1,2,4,*
1Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
2Division of Cardiology, Department of Internal Medicine, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung, Taiwan
3Division of Trauma and Surgical Critical Care, Department of Surgery, Kaohsiung Medical University Hospital, Kaohsiung Medical University, Kaohsiung City, Taiwan.
4Department of Internal Medicine, Faculty of Medicine, School of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
Received Date: 11/06/2024; Published Date: 04/10/2024
*Corresponding author: Dr. Po-Chao Hsu, Division of Cardiology, Department of Internal Medicine; Kaohsiung Medical University Hospital, 100 Tzyou 1st Road, Kaohsiung. 80708, Taiwan, ROC
Abstract
Renal vascular injury is a rare complication following blunt trauma. Herein we reported a 15-year-old male who suffered from renal artery thrombosis after a motorcycle accident. Initial assessments revealed multiple fractures and bilateral renal infarctions. Emergent angiography showed significant stenosis and total occlusion in the renal arteries. The patient underwent successful angioplasty and stent placement in the left renal artery. Post-intervention, the patient exhibited substantial improvement, with urine output exceeding 2000 ml per day and normalization of creatinine levels within 22 days. Dual antiplatelet therapy was administered post-procedure. This case highlights the effectiveness of percutaneous endovascular therapy in managing blunt trauma-induced renal artery thrombosis and underscores the importance of early intervention to restore renal function in young patients.
Introduction
Renal vascular injury was a rare complication followed with blunt trauma. Within all etiology, blunt trauma related renal artery thrombosis comprised about 40% of all cases [1]. Revascularization by any means had been debated for a long time since revascularization didn’t always lead to improvement of renal function [2]. Percutaneous endovascular therapy had rising since 1995. As the technology became mature, endovascular therapy gain more expectation [3]. Herein, we presented a young adolescent with blunt trauma related renal artery thrombosis, whose renal function improved very well after percutaneous endovascular treatment.
Case Presentation
This 15 years old male adolescent without any underlying systemic disease had a traffic accident on February 2, 2023. He was riding a motorcycle with helmet use and bumped into a car with transient conscious lost for minutes. His conscious improved on ambulance without memory loss. He was sent to a district hospital immediately. Initial survey included chest Computed Tomography (CT), brain CT and limbs plain films, showing no intracranial hemorrhage, right 9-11th rib fracture with minimal pneumothorax, left maxillary bone fracture, left humeral fracture and left proximal ulnar fracture with elbow dislocation. No cervical or lumbar spine fracture was found. He was then transferred to our hospital for further treatment.
At our hospital, he presented with mild hypotension, tachycardia, conscious clear and oriented. In addition to wound pain, he complained abdomen pain and low back pain. Lab data showed elevated liver enzyme and creatinine (1.3mg/dL). Emergency department doctors kept transfusion, aggressive hydration and arranged abdomen CT, which showed liver laceration with both lobe of liver, adjacent hematoma, splenic laceration and bilateral renal infarction. There were wedge shape poor enhance lesion in right kidney and whole left kidney was hypointense. Small caliber of bilateral renal artery was found, thus acute renal artery thromboemobolism, dissection was highly suspected (Figure 1). Therefore, cardiovascular department was consulted for emergent angiography.
Initial angiography showed 40-50% stenosis over upper side branch of right renal artery. However, left renal artery angiography showed 100% total occlusion (Figure 2A). We further performed angioplasty with 2x15mm, 2.5x15mm balloon over left renal artery and then inserted a bare metal stent (2.75x22mm) over it (Figure 2B, 2C). After intervention, left renal artery revealed patent blood flow. He was then admitted to our pediatric intensive care unit for further monitoring. He had more than 2000ml urine output per day without regular diuretic use. No electrolyte imbalance was found. His creatinine kept rising since admission up to 3.6mg/dL and passed peak on February 8, 2023. Dual-antiplatelet with aspirin 100mg and clopidogrel 75mg once daily was also used after improvement of his bleeding condition. The patient was then discharged with creatinine back to 1.04mg/dL.

Figure 1: Abdominal computed tomography showed wedge shape poor enhanced lesion over right kidney and hypodense left kidney with small caliber of renal artery.

Figure 2A. Left renal artery angiography showed total occlusion.

Figure 2B. Angioplasty was then performed over left renal artery.
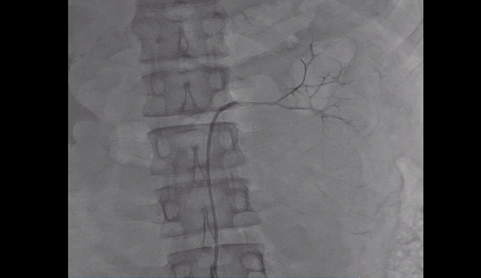
Figure 2C. Left renal artery flow improved after intervention.
Discussion
Renal infarction is a rare ischemic event caused by complete or partial occlusion of the main renal artery [4]. Bourgault et al. presented a case series, collected retrospectively between 1989 to 2011 including 94 cases [5]. In the study, they classified the etiology of renal infarction into 4 groups: cardiac group, renal injury, hypercoagulable group and idiopathic group. However, trauma related renal artery infarction wasn’t mentioned specifically. In 2019 Ana et al.’s systemic review, cardiac or aortic embolism was responsible for 45.4% of the reported cases, which was the leading cause [6].
Among blunt abdomen trauma cases, renal injury was not uncommon, about 1-5% [7]. However, blunt trauma with renal vascular injury was rare, about 0.05-0.08% [8, 9]. Tracing back the history of blunt trauma related renal artery injury, the earliest case had been reported in 1861 by Von Recklinghausen [10]. Increasing cases was found during early 1900s. In 1927, Neuburger hypothesized trauma causing renal artery spasm leading to further infarction. However, thrombosis of main artery had been demonstrated by Barney and Mintz through autopsy in 1933 [10]. Clark D.E. in 1981 had demonstrated 10 such cases and review 240 cases from previous literature, the renal vascular injuries could be described as avulsion in 12% of cases, laceration in 4% of cases, thrombosis in 44% cases, intimal flap in 7% and arterial spasm in 4% of cases [1]. There were 2 possible mechanisms of blunt trauma induce renal artery thrombosis [11]. First, the acute deceleration caused stretching of renal artery, leading to intima disrupt, exposing the endothelium and initiated thrombotic cascade. This concept was support by the observation that left renal artery was more vulnerable to such blunt trauma compared to right renal artery, which was surrounded by inferior vena cava and duodenum, causing less motion [12,13]. Hass et al. demonstrated similar concept that left renal artery injury was more common than right side with a ratio of 1.4:1-1.2:1. He also explained by the more acute angle of left renal artery to abdomen aorta, causing more stretching during blunt injury [14]. Second, it was believed that renal vessels had been compressed against vertebral body, causing intimal damage [13]. Currently, abdomen dynamic contrast CT could detect the occlusion of renal artery accurately [13,15].
Current treatment options for acute renal infarction included catheter direct thrombolysis, systemic thrombolysis, anticoagulation and surgery [4]. However, the role of revascularization by any means hadn’t been well established. Mulayamkuzhiyil Saju suggested revascularization was indicated in following circumstances: complete occlusion of main or major segmental renal artery < 6 hours duration, solitary kidney, or significant reduction of GFR from baseline (<50ml/min GFR); partial occlusion of main or major segmental renal artery of <24 hours duration or had persisted hypertension, flank pain, renal failure; a renal infarction associated with arterial dissection [4, 16-18]. However, if we narrowed down the population to blunt trauma related renal artery injury, the optimal approach was less clear due to small sample size. Jaws A. also mentioned the preference of conservative treatment because of delay in diagnosis and that revascularization not always resulted in return of renal function [2]. Open surgical revascularization had seldom been done due to poor preserved renal function rate, about 14-29% from previous literature [19]. For less invasiveness and maturing tools, percutaneous endovascular revascularization had risen, gaining more expectation. Percutaneous endovascular revascularization by stent placement following blunt trauma related renal injury had first been demonstrated in 1995 [3]. Yu-Wei Tsao had reported similar case that the renal function successfully improved after thrombosuction and stent placement in 2016, as first case been reported in Taiwan [20]. In 2017, Jahangiri, Y. had collected 54 cases undergone percutaneous endovascular revascularization for blunt trauma related renal arterial thrombosis [21]. Most cases had stent placement with 2 cases for PTA alone, 1 for thrombosuction alone and 1 for thrombolysis alone. The time to intervention interval lasts about 4-12 hours in general with 48 hours. Technical success was achieved in 88.9% cases and clinical success in 75% cases after 6 months follow-up. 6 technical failure cases had following 3 reasons: failed recanalization (3 cases), failed guidewire passage (2 cases) and persistent notch between stents (1 case) [22-24]. Within technical success group, 12 clinical failure cases showed persistent occlusion of the renal artery (10 cases) and renal artery dissection (2 cases) [23, 25-34]. During sub-group analysis, predictors of clinical success included total occlusion of renal artery on presentation and post-procedure anti-platelet treatment (aspirin, clopidogrel or both), while time to intervention didn’t cause significant difference [21].
In our case, we demonstrated a case with blunt trauma related renal artery thrombosis successfully treated by endovascular therapy. After angioplasty and stent placement with post-procedure dual-antiplatelet, his renal function gradually improved and creatinine level completely returned to baseline in 22 days. Though the time to intervention didn’t play important role in previous study [21] , we believed that prompt intervention before tissue necrosis still posed significant role leading to dramatic improvement of renal function in our case.
Conclusion
Our case highlights the efficacy of prompt percutaneous endovascular intervention in managing blunt trauma-induced renal artery thrombosis, particularly in young patients. It underscores the potential of such minimally invasive techniques to restore renal function and emphasizes the importance of early intervention before the onset of tissue necrosis.
References
- Clark DE, Georgitis JW, Ray FS. Renal arterial injuries caused by blunt trauma. Surgery, 1981; 90(1): p. 87-96.
- Jawas A, Abu-Zidan FM. Management algorithm for complete blunt renal artery occlusion in multiple trauma patients: case series. Int J Surg, 2008; 6(4): p. 317-322.
- Whigham CJ, Jr Bodenhamer JR, Miller JK. Use of the Palmaz stent in primary treatment of renal artery intimal injury secondary to blunt trauma. J Vasc Interv Radiol, 1995; 6(2): p. 175-178.
- Mulayamkuzhiyil Saju J, Leslie SW. Renal Infarction, in StatPearls. Treasure Island (FL) relationships with ineligible companies. Disclosure: Stephen Leslie declares no relevant financial relationships with ineligible companies, 2023.
- Bourgault M, et al. Acute renal infarction: a case series. Clin J Am Soc Nephrol, 2013; 8(3): p. 392-398.
- Pizzarossa AC, Merola V. Etiology of renal infarction. A systematic review. Rev Med Chil, 2019; 147(7): p. 891-900.
- Singh S, Sookraj K. Kidney Trauma, in StatPearls. Treasure Island (FL) ineligible companies. Disclosure: Kelley Sookraj declares no relevant financial relationships with ineligible companies, 2023.
- Sangthong B, et al. Management and hospital outcomes of blunt renal artery injuries: analysis of 517 patients from the National Trauma Data Bank. J Am Coll Surg, 2006; 203(5): p. 612-617.
- Zheng Z, Dong M, Hu K. A preliminary evaluation on the efficacy of ozone therapy in the treatment of COVID-19. J Med Virol, 2020; 92(11): p. 2348-2350.
- Lichtenheld FR, Franklin SS, Serenati QJ. Renal infarction due to trauma. J Urol, 1961; 85: p. 710-713.
- Tillou A, et al. Renal vascular injuries. Surg Clin North Am, 2001; 81(6): p. 1417-1430.
- Dinchman KH, Spirnak JP. Traumatic renal artery thrombosis: evaluation and treatment. Semin Urol, 1995; 13(1): p. 90-93.
- Bruce LM, et al. Blunt renal artery injury: incidence, diagnosis, and management. Am Surg, 2001; 67(6): p. 550-554; discussion 555-556.
- Haas CA, Spirnak JP. Traumatic renal artery occlusion: a review of the literature. Tech Urol, 1998; 4(1): p. 1-11.
- Kawashima A, et al. CT evaluation of renovascular disease. Radiographics, 2000; 20(5): p. 1321-1340.
- Silverberg D, et al. Acute renal artery occlusion: Presentation, treatment, and outcome. J Vasc Surg, 2016; 64(4): p. 1026-1032.
- Ouriel K, et al. Acute renal artery occlusion: when is revascularization justified? J Vasc Surg, 1987; 5(2): p. 348-355.
- Lim JL, Lau KK, Lim AKH. Successful rescue from kidney failure with delayed catheter-directed intervention after catastrophic bilateral kidney paradoxical thromboembolism. BMJ Case Rep, 2022; 15(2).
- Singh O, et al. Isolated renal artery thrombosis because of blunt trauma abdomen: report of a case with review of the literature. Urol Int, 2011; 86(2): p. 233-238.
- Yu-Wei Tsao S-HC, Jiann-Hwa Chen, Wei-Lung Chen. Renal artery thrombosis induced by blunt abdominal trauma : A case report and literature review. Resuscitation & Intensive Care Med, 2016; 1(2016): p. 192-195.
- Jahangiri Y, Ashwell Z, Farsad K. Percutaneous renal artery revascularization after prolonged ischemia secondary to blunt trauma: pooled cohort analysis. Diagn Interv Radiol, 2017; 23(5): p. 371-378.
- Long JA, et al. Traumatic dissection of the renal pedicle. Modalities of management in adults and children. Prog Urol, 2004; 14(3): p. 302-309; discussion 308.
- Lopera JE, et al. Traumatic occlusion and dissection of the main renal artery: endovascular treatment. J Vasc Interv Radiol, 2011; 22(11): p. 1570-1574.
- Springer F, et al. Delayed endovascular treatment of renal artery dissection and reno-vascular hypertension after blunt abdominal trauma. Cardiovasc Intervent Radiol, 2011; 34(5): p. 1094-1097.
- Merrot T, et al. Trauma of the renal pedicle in children. Report of 2 cases of late revascularization with endovascular prosthesis. Prog Urol, 2000; 10(2): p. 277-281.
- Lutkevich C, et al. Percutaneous transluminal angioplasty of an acute traumatic renal artery occlusion. Tenn Med, 2000; 93(4): p. 140-141.
- Delarue A, et al. Major renal injuries in children: the real incidence of kidney loss. J Pediatr Surg, 2002; 37(10): p. 1446-1450.
- Flugsrud GB, Brekke M, Roise O. Endovascular stent in the acute treatment of blunt renal arterial injury. J Trauma, 2005; 59(1): p. 243-245.
- Hsu W, Mitchell SE, Kim HS. Renal artery stenting for intimal flap injury in a 2-year-old child after blunt abdominal trauma. South Med J, 2006; 99(8): p. 884-887.
- Guillen G, et al. Five years of renal trauma in a paediatric trauma center: new tools in the diagnostic and therapeutic process. Cir Pediatr, 2007; 20(4): p. 209-214.
- Breyer BN, et al. Endovascular management of trauma related renal artery thrombosis. J Trauma, 2008; 64(4): p. 1123-1125.
- Civy AM, et al. Bilateral traumatic dissection of the renal arteries. Ann Fr Anesth Reanim, 2008; 27(9): p. 727-730.
- Kushimoto S, et al. Traumatic renal artery occlusion treated with an endovascular stent--the limitations of surgical revascularization: report of a case. Surg Today, 2011; 41(7): p. 1020-1023.
- Abu-Gazala M, et al. Endovascular management of blunt renal artery trauma. Isr Med Assoc J, 2013; 15(5): p. 210-215.

