An Overview of Tuberculous Spondylitis in a Tertiary Institution in North Central Nigeria (A 10 Year Retrospective Study)
Mancha DG*, Ode MB, Taiwo O, Yilleng SB and Onche II
Department of orthopedics and trauma, Jos University Teaching Hospital, Nigeria
Received Date: 24/05/2024; Published Date: 02/10/2024
*Corresponding author: Mancha DG, Department of orthopedics and trauma, Jos University Teaching Hospital, Nigeria
Abstract
Background: Tuberculous spondylitis has remained a significant health encumbrance in our environment because of the debility it causes. It is a product of dissemination from primary in other parts of the body. Its devastating consequences emanates surreptitiously into the spine and renders its victim inept.
Objective: We highlight the trend in presentation and associated demographics and challenges in the diagnosis and management of patients with tuberculous spondylitis in Jos university Teaching Hospital (JUTH) during the ten-year period from October 2014 to September 2023.
Method: This is a retrospective study of patients treated for tuberculous spondylities from October 2013 to September 2023 in Jos University Teaching Hospital (JUTH). Information was obtained from folders and records in surgical out-patient clinic and from admission and discharge registers and summaries of patients managed in the out-patients clinics, wards and theater records of those treated from October 2014 to September 2023.This was corroborated by card records in the DOTS unit. Patients ages grouped and profiled as young adults (18 -44) years, middle age (45-64) years and older adults from 65 years and above. The data was analyzed using stata version 17
Results: A total number of 432 patients were treated during the period under review with 279 male and 153 female, Male: female ratio of 2.8:1. Age range from 18 to 87 while the mean age is 47.1(+-15.5). Low back pain was the most common symptom while sensation was preserved in all the patients. The mean duration of symptom (back pain) at presentation was 10.9 +-5.9 months. A total of 54(12.8%) patients had gibbus among which young adults were 30(55.6%), middle aged 18 (33.3%) and older adults were 6(11.1%) that had gibbus. There was significant association between gibbus and age and duration of symptoms before presentation. A total of 81(18.8%) patients had either paralysis or paraparesis among which 49(60.4%) were young adults, 24(29.6%) middle aged and 8(9.9%) older adults. Half of the patients had sought services from traditional medication before presentation. Diagnostic profiling was conclusive in 67% of cases while therapeutic trial was instituted among the rest. 255(59.0%) patients were ambulatory while 177 (40.9%) were admitted into the wards. Paralysis was found among 55(12.7%) of the patients, 14(3.2%) developed pressure while 56 (13.0%) patients had concomitant retroviral disease RVD.
Conclusion: Tuberculous spondylitis is still a ravaging scourge in the country and still constitutes a major public health burden in Jos and its environs.
Keywords: Tuberculous spondylitis; Debility
Introduction
Tuberculous spondylitis is a chronic infection involving the spine and adjourning structures with immense tissue destruction that may result in debility and fatal consequences [1,2]. Tuberculosis is a leading cause of death globally with ten million annual new cases and is responsible for 1.8 million deaths in 2018 alone [3-5]. Tuberculous spondylitis is common chronic infectious disease and constitute 50-75% of extra-pulmonary tuberculosis and 4% of all cases [6,7]. Percieal Pott in 1779, was the first patient found to have presented with classically described features with the kind of paralysis of the lower limbs that is frequently accompanied by curvature of the spine [7-9]. Its manifestation can be termed protean in nature due to its tendency to mimic other disease entities. This infectious disease condition has been known to mankind since prehistoric times and the organism has been documented in the remains of the prehistoric skeleton as evident in paleo pathologic specimens of bone, joints and spine remains [9,10].
It is acquired as a result of primary or secondary lesion elsewhere in the body (tonsils, gut, kidneys) and conveyed through the vascular, lymphatic or adjourning contiguous structures [9,14]. It is almost always a secondary or tertiary lesion but occasionally beyond this description. Ultimately, it’s devastating consequences is hauled on the spine due the damage it inflicts directly on the vessels or indirectly on the structural and neural framework of the vertebrae. Its genetic susceptibility has been demonstrated in patients associated FokI polymorphysm and the vitamin D receptor gene in Chinese population [1]. Individuals with GA+AA genotype in the dominant model have up to 2.067–fold increase risk of developing tuberculosis of the spine [11]. Its susceptibility to inflict extensive destructive infection resulting in lethal consequences cut across all age groups [12,13]. Its predilection to children and the young actively working age group in their sexually active age impose a great economic burden to a developing country. The condition had become rife and more apparent in the past 3 decades due to increase prevalence of retroviral disease. The developed world was not spared as recrudescence of the disease and increase global migration became apparent [2,14,15,18]. The debilitating consequences and universal spread the disease endeared the WHO to declare it a global emergency in 1996 [16].
The implications of this, is the encumbrance pose by the cost, duration and complexity of treatment plan, its consequences and impact of the choice of treatment can be considered enormous [15]. In our setting, the demographics may be altered by extraneous and exogenous factors. This is because of the unpredictable nature of interference of the risk factors such as immune-suppression, tendency for patients to present late, delay cause by early patronage of non-orthodox practioners, the underlying socio-economic setting, proximity and access to care and affordability of investigative tools which contributes in rendering majority of the victims susceptible to this severe form of the disease [2,17]. These factors may be attributable to ignorance and poverty and prevalence of other diseases which mask or mimic early features and blunt early hallmarks of the ailment.
Diagnosis poses a significant challenge in the early and late course of management due to presence of obvious differentials. The general symptoms of fatigue, night sweats, weakness, cough, diurnal fever, weight loss, pulmonary symptoms and lymphadenopathy may be absent except the presence of low back pain or gibbus [2,13]. Gibbus itself might in this environment be seen in sickle cell spondylodiscitis, hematologic malignancies, multiple myeloma, older patients with osteoporotic vertebral fractures, neglected incomplete cord injuries from wedge compression fractures. Added to these, the endemic status of the disease provides for protean manifestation clinically. In patients with early HIV or even without HIV infection high index of suspicion is required because it manifest similar to the non-retroviral patients [18,19]. In late HIV positive patients however, a more atypical symptoms and signs are exhibited [19]. Specific features include spine instability, axial, radicular pain, nerve root compression, deformities, weakness of the extremities, groin bogginess and sinuses may be noticed.
The definitive diagnosis of tuberculous spondylitis is in the histopathologic tissue biopsy specimen or the isolation of the infective organism from the aspirate of the lesion [18,20]. In this setting the tools required to harvest the specimen especially advance imaging and surgical techniques with instrumentation for minimal invasive access with biopsy needles are lacking. This imposes an extra burden of cost of diagnosis and undue exposure of patient to therapeutic trials as result of lack of direct specimen. New diagnostic methods such nucleic acid amplification, enzyme-linked immune spot assay for interferon gamma (produced by activated T-cells exposed to mycobacterium tuberculosis) are becoming available [21].
With this apparent limitation in diagnosis and difficulty in determining drug susceptibility, inferential methods are made use based on clinical, radiological and anciliary haematoliological and hypersensitivity skin tests [2]. In spite of all these barrages of investigations the test results may still be equivocal [2].
Factors that may modify our decision making, diagnosis treatment outcome include background endemicity, nutritional status, comorbidity, age, gender, interference with other tropical diseases, traditional medications and practices and unprescribed medications obtained over the counter. These however do not undermine the existence of modern and sophisticated investigations such as QuantiFERON, Eliezer, PCR which are available. But the cost renders these tools inaccessible to many. Furthermore, the presence of myriad of metabolic, degenerative, pyogenic infectious and mitotic lesions must be differentiated in order to arrive at suitable diagnosis.
Although resistance is said to be rare in multi drug therapy relapse after completion of therapy often occur and recommencement of therapy had to be recommenced all over again. The effectiveness of this is strengthened by Yeagers observation that prolong use of combine multi antimicrobial therapy has diminished relapse to its lowest limit in history [8,9]. Interestingly these patients had hitherto responded favorably to the multidrug therapy. In our setting these clinical poor responsiveness may be adduced to multidrug resistance or recrudescence. The recurrence has been found to be between 2-5% in a 5 to 10 year follow up [9]. The shortened period ant tuberculous therapy associated with DOTS may be responsible for this happening. While the goal of treatment is the eradication of the disease therapeutically, additional intervention surgically (debridement, decompression and stabilization) may be required in cases that meet the indication.
Methodology
This is a retrospective study of all consecutive patients treated for tuberculous spondylitis in orthopedic surgical out-patients clinic, those admitted via the emergency unit and those reviewed in the DOTS unit of Jos university Teaching Hospital from September 2013 to September 2023.Identification of patients was made in their folders, soe operation registers, and follow up reviewed in the DOTS unit. The data obtained was reviewed for demography, date of commencement of treatment, radiological attributes, associated morbidity, treatment modality, follow up and outcome. Admission was offered based on the severity of symptoms and co morbidity. Patients were routinely treated with anti-tuberculous chemotherapy. The data was analyzed using STATA
Patients and methods: This is a retrospective study of patients treated for tuberculous spondylities from October 2013 to September 2023 in Jos University Teaching Hospital (JUTH). Information was obtained from folders and records in surgical out-patient clinic and from admission and discharge registers and summaries on the wards and the theater records of those treated from October 2013 to September 2023.This was corroborated by records in the DOTS unit. Patients age grouped as young adults (18 -44) years, middle age (45-64) years and old adults from 65- and above. Ages of the patients are profiled into young adults (18-44), middle age (45-64) and older adults (65- and above).
Results
A total number of 432 patients were treated during the period under review with 279 male and 153 female, Male: female ratio of 2.8:1. Age range from 18 to 87 while the mean age is 47.1(+-15.5) years. Retroviral disease was found among 55(13%) patients. Those within 18-44 age group had statistically significant association with number of gibbus at p-value 0.05 18. Others were 6 for middle age and 6 for older adults. The same age group (18-44) had statistically significant association with number of patients with paralysis (49) at p-value 0.05, middle age was 24, older adults were 8. Low back pain was the most common symptom and its mean duration is 10.9(+-5.9) months. This duration of symptom has significant association with paralysis. Sensation was preserved in all patients. A total of 54 patients had gibbus among which young adults were 30,18 were middle aged and 6 older adults. A total of 83 patients were paralyze among them 49 were young adults, 24 middle aged and 10 older adults. Half of the patients had sought services from traditional medication before presentation. Diagnostic profiling was conclusive only in 67% of cases while therapeutic trial was instituted among the rest. patients that were ambulatory were 255 and those admitted ab initio were 175.
Table 1: Characteristics of Patients with TB Spine.
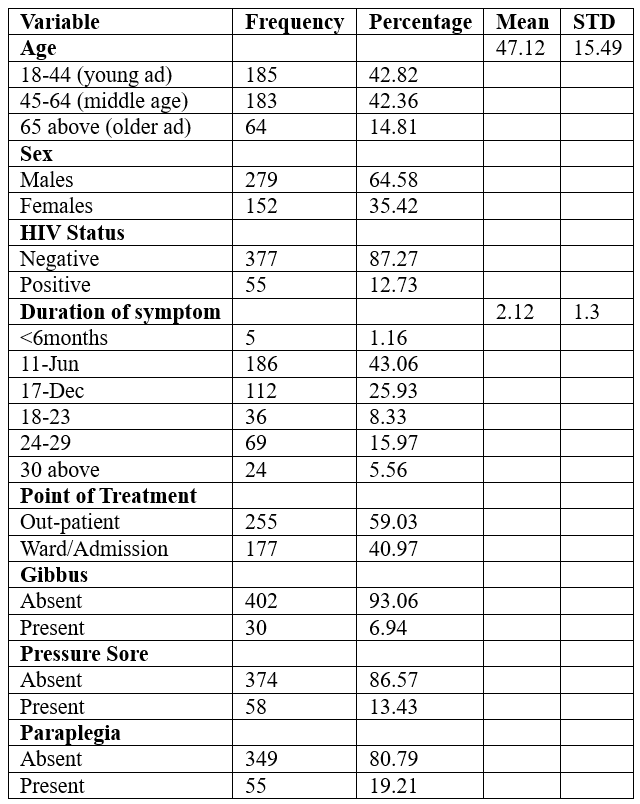
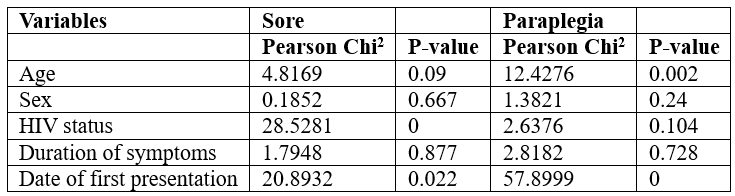
Table 2: Correlation between Variables and Outcomes.
DIscussion
Tuberculosis is of the spine is responsible for large percentage of non-traumatic compressive myelopathies resulting in paraparesis and paraplegia in Nigeria, India and Ethiopia and the most common cause death from an infectious disease word wide [17-19,31]. This study presents the largest cache of (432) patients with tuberculosis of the spine in a Nigerian tertiary institution in a 10 year study. In UCH Ibadan 9 cases were reported in period of six years (1966-1972), in Ilorin 50 patients reported in a 10 year (2001-2009). In Kano it constituted 44% of the 98 patients treated within 4 years (2006-2009) as a cause of non-traumatic paraplega in Murtala Mohammed hospital. Even among children in same kano, only26 children were noted in four years (2001-2004). Suffice to state that only 32 patients were admitted and treated in 5 years (1995-2000) in Jos University Teaching Hospital for tuberculous spondilitis [2]. All these show the poor patronage of health facilities by patients despite enormous premium placed on strategies for TB eradication and the fact that these centers lie within endemic area. This also show that progress in prevention of tuberculosis is slow [20]. These large number of patients in Jos is a function of increase in awareness and increased health seeking behaviors of the populace. It also reveals there is a large number of reservoirs of the disease in the communities. Poor patronage of established facilities for treatment and escape in routine diagnosis of extra-pulmonary tuberculosis may be among the reasons for poor patronage in other centers [15,20]. Hence the need for more vigorous health education campaigns and public enlightenment across the country.
Another major reason for the ever-increasing number of patients is the persistence of existing hallmarks and determinants of its prevalence such as poverty, HIV infection, diabetics, under nutrition, and smoking. Others include extreme of age and alcoholism. Out of these smoking and alcoholism are vices common among male young adults. It is worthy of note that Nigeria is responsible for 4.4% and among the 8 countries that contribute three quarters of the world’s tuberculous affliction [20].
The gross preponderance of male gender portrays this infectious disease as one that inflicts the large number of the work force as men constitute majority of outdoor labor force. They are also the major bread winners of the families and are veritable custodians that bore the burden of the communities. Male preponderance could also be trace to their social habits, practices and occupations which make them more vulnerably exposed to outdoor influences [21]. Women tendency to seek early medication is predicated on their caregiver, home maker roles and their tendency to protect their children and themselves. Perhaps the tight schedules of men tend to render them less conscious of their health needs. This is consistent with the findings in our center over 20 years ago and in Kano [2,17]. However, in Ilorin, Port Harcourt and Enugu female preponderance is marginal and almost equal [16,22,32]. Although this may not be explained only on grounds of exposure alone the cumulative stress and economic forces acting takes a great toll on the immune status of most of the men.
The mean age of our patient (47.1±15.5 years) is skewed toward middle age category. In Owerri (South East, Nigeria) however, majority falls among a little younger age with the mean age of 38.5+-4.4. What is peculiar and important to this age groups is that the age group constitute the strongest, most productive ,most vibrant and literate segment of the society. It also signifies that the productive age group are most exposed and made vulnerable to this infectious disease with great antiquity.
This study highlighted a significant association between young adult age group with the preponderance of gibbus, retroviral disease and the most severe stage of the disease, paralysis and pressure sore.
While gibbus provides a lead pointer to diagnosis its presence in the younger age group may be explained by the great amount of action of forces exerted by the para-spinal muscles of the trunk on the disease or weak vertebrae during spasms. This is particularly significant as it is associated with the muscles surrounding the lumbar spine which we found as the most affected segment of the spine. Again, this part of the trunk resides the most powerful group of muscles responsible for keeping an individual upright and explains further the existence of gibbus in the lumbar region than other sections of the spine. The young may also be difficult to confine since they spend a great amount of their time working in pursuit of their livelihood.
The high prevalence of retroviral disease among this group is not strange since they constitute the most sexually active, sociable and outgoing age group with high propensity to engage in risky experimental activity. Most adventures and associations of marriages are often conducted among this age group. In addition true characters of adulthood manifest in these age group too.
It is however surprising that these age group manifest the most severe form of morbidity in form of paralysis. This may be as a result of the impact of the high number of the collapsed vertebrae (gibbus) or the association with retroviral disease among them.
Prolong delay in presentation is unique among patients with tuberculous spondilities as this is also recorded in Enugu (South East Nigeria) where 70.2% patients presented within 24 months of onset of the symptoms [32]. The implication of this prolong duration of symptoms at presentation is that there is significant association between duration of symptoms at presentation and severity of the disease as they constitute the largest number of admissions, highest number of paralyzed patients and development of pressure sores. The large number of admissions among this group reveals the demographic propensity and index of developing the severest form and debility. This prolong delay in presentation may also arise because diagnosis of extrapulmonary tuberculosis can be almost always challenging and could often be delayed [33]. Besides, the most common symptom (back pain) is a confounding feature among other common disease conditions although other multifaceted factors contributing to this delay may suffice.
Tuberculous spondylitis is ever increasing in our setting particularly due to deteriorating socioeconomic status of the citizens, large reservoir of the disease and poor health seeking behaviors. The preponderance of the disease among young adults implies that the prevention and treatment must be targeted among this group carried out concurrently. The frontline physicians must embark on regularly training workshops in order to have a high index of suspicion. From the era of non-routinely done spine surgeries to the present era in which routine surgeries can be performed not much has changed because the cost of spine surgery, absence of readily available minimal access surgical diagnostic tools renders both the patientand the surgeon from accessing the game changing surgical input.
References
- Gark RK, Somvanshi DS. Spinal tuberculosis: A Review. The j spinal cord medicine, 2011; 34(5): 440-454.
- Nwadiaro HC, Legbo JN, Ukoli C, Opaluwa AS, Onche II. Treaties on tuberculous spondylities. Nig. J orthopedic and trauma, 2002; 1(2): 76-81.
- World Health Organization. Global Tuberculosis Report 2022.World Health Organization; Geneva, Switzerland: 2022.
- . MacNeil A, Glaziou P, Sismanidis C, Date A, Maloney S, Floyd K. Global Epidemiology of Tuberculosis and Progress Toward Meeting Global Targets—Worldwide, 2018. MMWR Morb. Mortal. Wkly. Rep, 2020; 69: 281–285.
- Glassman I, Nguyen KH, Gless J, Alcantara C, Booth M, Venketaraman V. Pathogenesis and diagnostic challenges and risk factors of Potts disease. PMC clinic and practice, 2023; 13(1): 155-165.
- Luk KDK. Spinal tuberculosis. Curr. Opin. Oetho, 2000; 11: 196-201.
- Viswanathan VK, Subramanian S. Pott Disease.Stat Pearls Publishing; Tampa, FL, USA, 2022.
- Tuli SM. Anterior approach to the cervical spine. Indian J Orthop, 1979; 13: 23-33.
- Tuli SM. Tuberculosis of the spine: A historical review. Clinical orthopedics and related research, 2007; 460: p29-38
- Lichtor J, Lichtor A. Paleopathologic evidence suggesting pre-Columbian tuberculosis of spineJ Bone joint surg am,1957; 39: 1938-1939.
- Li T, Wang L, Gou C, Zhang H, Xu P, Shaohua L, et al. Polymorphysms of SLC11A1(NRAMP1) rs17235409 associated with and susceptibility to s-pinal tuberculosisin a sourhern Han Chinese population. Infect Genet Evol. Science direct, 2022; 98.
- Benzagmout M, Boujraf S, Chakour K, Chaoul ME, Potts disease in children. Surg. Neu. Int, 2011.
- Leowattana W, Leowattana P, LeowattanaT. Tuberculosis of the spine. World J orthop, 2023; 14(5): 275-293.
- Risher KA, et al. Age patterns of HIV incidence in east and southern Africa: a modeling analysis of observational population-based cohort study. Lancet HIV, 2021; 8(7): e429-e4439.
- Saunders K. Diagnosis of TB in the presence of HIV-a view from a rural hospital. Africa Health, 2001; 2-8.
- Solagberu BA, Ayorinde RO. Tuberculosis of the spine in Ilorin, Nigeria. East Afr J Med, 2001; 78(4): 197-199.
- Owolabi LF, Ibrahim A, Samaila A. A Profile and outcome of nontraumatic paraplegiain Kano,North western NigeriaAnn Afric Med, 2011; 10(2): 86-90.
- Chaurasia RN, Verma A, Joshi D, Misra S. Etiological spectrum of non-traumatic myelopathies:experience from tertiarycenter.J assoc. Pphysicians India, 2006; 54: 445-448.
- Fidele NJ. Amanuel A. Spectrum of non traumaticmyelopathies in Ethiopean patients.:hospital based retrospective study. Spinal cod, 2016; 54(8): 604-608.
- Chikaya J, Khan M, Ntoumi F, Aklillu F, Fatima R, Nathan PM. Global tuberculosis report 2020- Reflections on the global TB burden, treatment and prevention methods. International j Infectious disease, 2021; 113: S7-S12.
- Nwene EK. Tube4rculosis and gender in Nigeria, Sex differences in diagnosis and treatment outcome of TB and TB HIV infected patients.Gender assessment in Nigeria. Texila int J public Health, 2016; 4(4).
- Ekere AU, Yellowe BE, Echem RC. Conservative management of Tuberculous spondilitis in a developing country. Nig J Medicine, 2005; 14(4): 386-389.
- Das B, Puet TA, Watanakunakorn C. Tuberculosis of the spine (Potts Disease) presenting as compression fractures.Spinal cord, 2002; 40(11): 604-608.
- Dunn RN, Husien MB. Spinal tuberculosis :A review of current management. Bone Joint J, 2018; 100 B (4): 425-431.
- World health organization. Tuberculosis: A global emergency. Geneva: WHO, 1994.
- Rasouli MR, Mirkoohi M, Vacaro AR, Yarandi KK, Rahimi-Movaghar V. Spinal tuberculosis:Diagnosis and Management.Asian spine J, 2012; 6(4): 294-308.
- Shanmuganathan R, Ramachandran K, Shetty AP, Kanna AP. Active tuberculosis of spine: Current udates.N American spine soc. J, 2023; 100267.
- Saunders K. Diagnosing TB in the presence of HIV- a review from a rural hospital. Africa Health, 2001; 23: 2-6.
- Banwat ED. Pulmunary tuberculosis and extensively drug resistance tuberculosis Current trends. Jos J medicine, 2007; 2(1): 17-24.
- Wang JY, Chou C, Lee L, et al. Diagnosis of tuberculosis by an enzyme-linked immunospot assay for interferon gamma.Emer.infect Dis, 2007; 13: 553-558.
- World health organization. Stop TB annual report 2001. Geneva. WHO, 2002.
- Iyidobi EC, Nwadinigwe CU, Ekunife RT. Management of musculoskeletal tuberculosis in Enugu.J Tropical Medicine and Surgery, 2013; 1: 7.
- Talbot JC, Bismil Q, Sarayala D, Newton DA, Freizel RM, et al. Musculoskeletal Tuberculosis in Bradford.A six year review,Ann R Coll Surg Engl, 2007; 89: 405-409.
- Dookie N, Ngema SL, Perumal R, et al. The changing paradigm of drug resistant tuberculosis treatment:Success ,pitfalls and future perspectives.Clin Microbiol Rev, 2022; 35(4): e00180-19.
- Li K, Liu B, Zhang O. Recurrent spinal tuberculosis with HIV Infection after surgery: A rare case of Recurence and drug resistance. Dove press. Back to J –infection and drug resistance, 2023; 16: 7827-7833.

