Deep Cerebral Haematoma Due to a Road Accident in a Child: An Unsual Case
Sanae Jellal*, Nazik Allali, Rachida Chehrastane, Sara Zenjali, Jihane El Houssni, Lina Belkouchi, Siham El Haddad and Latifa Chat
Department of Pediatric Radiology, Children Hospital of Rabat, Mohammed V University Rabat, Morocco
Received Date: 28/05/2024; Published Date: 02/10/2024
*Corresponding author: Sanae JELLAL, Radiology Department, Children Hospital of Rabat, Ibn Sina University Hospital, Faculty of Medicine and Pharmacy of Rabat, Morocco
Abstract
Head injury in children accounts for a large number of emergency department visits and hospital admissions each year and remains a major cause of death and disability in children over 1 year of age. Falls are the most common type of injury, followed by motor-vehicle–related accidents [1]. Furthermore, child abuse remains a major cause of head trauma in children under 2 years of age.
Severe head trauma in children is less frequent than in adults, and the mortality rate is also lower [2].
Intracerebral hematomas are unusual in children and may be the result of focal brain injury or penetrating trauma. Most often they involve the temporal and frontal lobes. Many intracerebral hematomas can be treated conservatively. Those with significant mass effect or shift may require evacuation if clinically indicated. Repeated CT in high-risk lesions is recommended [3].
Case Report
The patient was an 11-year-old child who had been involved in a high-kinetic road traffic accident, and a brain scan revealed a deep cerebral haematoma, (Figure1) with foci of haemorrhagic contusions and meningeal haemorrhage. An additional cerebral MRI was ordered to investigate the aetiology, which revealed a voluminous capsulo-lenticulo-caudate and right thalamic haematoma, with heterogeneous signal, hyperintense in T1, hypointense in T2 and FLAIR and SWI a signal with blooming artefact without diffusion restriction (Figure 2, 3).
It is surrounded by a patch of peri-lesional oedema, with T2 and FLAIR hypersignals extending to the midbrain and homolateral hypothalamic region.
It exerts a mass effect on the homolateral lateral ventricle and V3, which are laminated, and on the midline, which is deviated to the left.
MRI also revealed multiple punctate signal anomalies above and below the tentorial level, the majority of which showed a T2 and FLAIR hypersignal and SWI a signal with blooming artefacts (oedemato-haemorrhagic) and others with a T2 hypersignal with diffusion restriction (oedematous) in relation to diffuse axonal lesions.
This is associated with the presence of foci of haemorrhagic contusions and individualisation of subarachnoid haemorrhage.
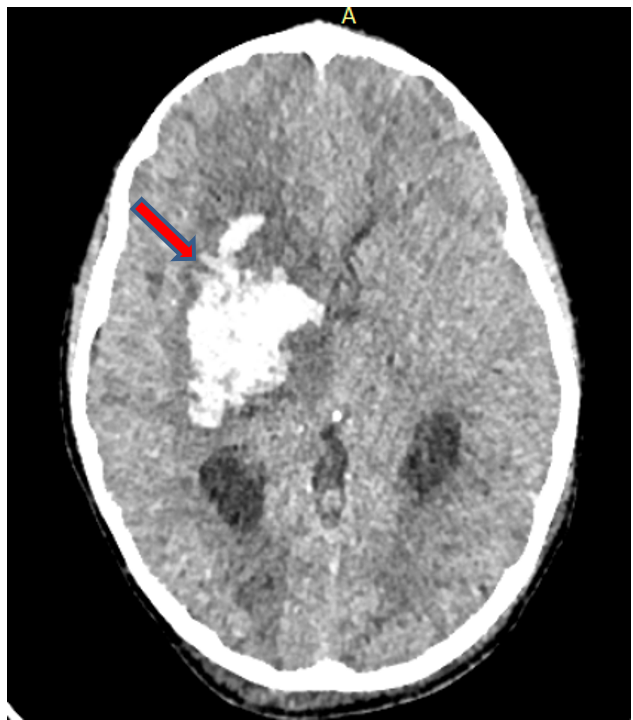
Figure 1: Injection-free CT scan showing a deep capsulo-lenticulo-caudate and right thalamic cerebral haematoma.
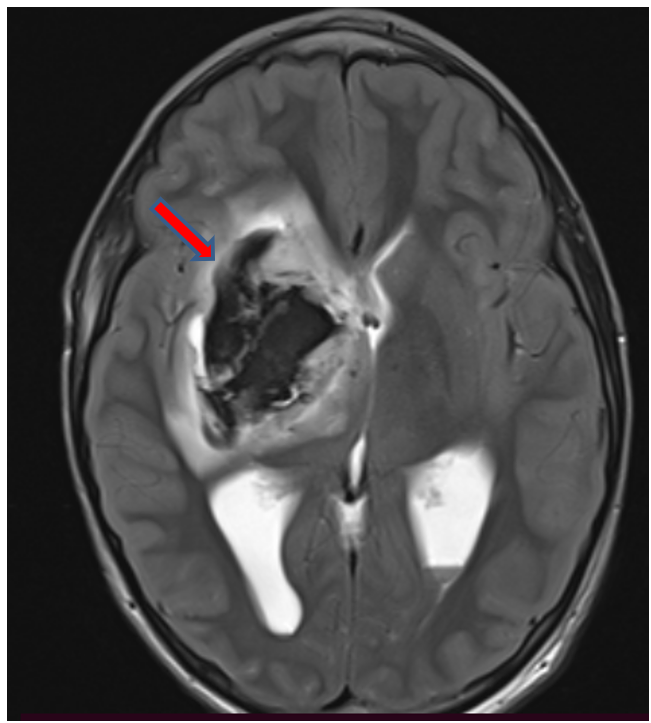
Figure 2: Cerebral MRI on axial T2 showing a right capsulo lenticulo caudate and thalamic cerebral haematoma with T2 hyposignal.
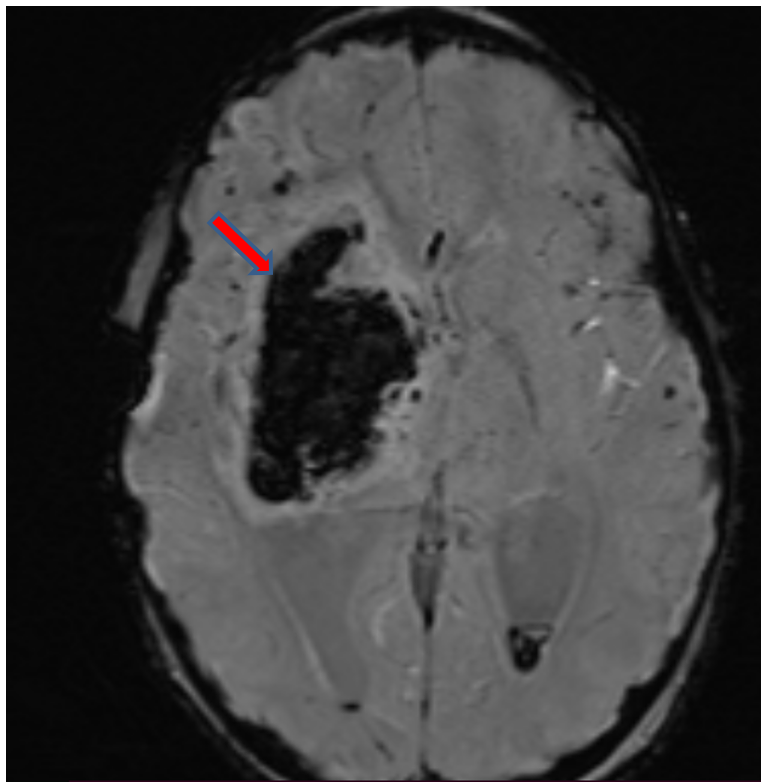
Figure 3: Cerebral MRI on SWI sequence showing a right capsulo lenticulo caudate and thalamic cerebral haematoma with SWI asignal.
References
- Adirim TA, Wright JL, Lee E, Lomax TA, Chamberlain JM. Injury surveillance in a pediatric emergency department. Am J Emerg Med, 1999; 17: 499–503.
- Kumar R, Mahapatra AK. The changing “epidemiology” of pediatric head injury and its impact on the daily clinical practice. Childs Nerv Syst, 2009; 25: 813–823.
- Durham SR, Liu KC, Selden NR. Utility of serial computed tomography imaging in pediatric patients with head trauma. J Neurosurg, 2006; 105: 365.

