Improved Super-Elastic Ti-Ni Alloy Wire for Nonsurgical Treatment of Skeletal Class II Malocclusion Combined with Large Overjet and Gummy Smile Case
Po-Jui Lin, Yuan-Hou Chen, Ching-Yu Yang and Jian-Hong Yu*
Department of Orthodontics, China Medical University Hospital Medical Center, Taichung, Taiwan
Received Date: 27/05/2024; Published Date: 02/10/2024
*Corresponding author: Dr. Jian-Hong Yu, Department of Orthodontics, China Medical University Hospital Medical Center, Taichung, Taiwan
Abstract
The case reported the use of improved super-elastic Ti-Ni alloy wire (ISW), which was developed by Tokyo Medical and Dental University, to correct a case of skeletal Class II malocclusion combined with large overjet and gummy smile. A 13-year-old female with a chief complaint of poor dental alignment and bucked teeth showed up in our clinic for treatment. Clinical examination revealed skeletal Class II relationship profile. Upper anterior teeth proclined with gummy smile and scissors bite over the left posterior teeth can be also noted. First, we used intrusion arch technique with TAD’s (temporary anchorage device) for bite control and gummy smile correction, and used bracket upside down with buccal crown torque for scissors bite correction. The treatment was finished with the improvement of facial appearance and a stable occlusion.
Keywords: Skeletal class II; Gummy smile; ISW; LH
Introduction
Tokyo Medical and Dental University developed improved super-elastic Ti-Ni alloy wire (ISW, also low hysteresis, LH). ISW is endowed with three superior abilities: super-elasticity, shape memory, and damping capacity [1-3]. The wire can be engaged into crowding dentition, and provide early dental torque control.
A Gummy Smile (GS) impacts both aesthetic and psychological well-being, often diminishing self-confidence and causing individuals to hide or restrain their smiles. A smile is classified as a gummy smile when more than 2 mm of gingiva is exposed. This condition can result from various factors, including altered passive eruption of the teeth, dentoalveolar extrusion, vertical maxillary excess, or short or hyperactive lip muscles. Effective treatment for a gummy smile should be tailored based on the underlying cause or causes.
Recently, mini-implants have been employed to address gummy smiles and deep overbites by intruding the upper incisors [4,5]. In 2006, Kim et al [4]. Utilized a segmental intrusive force on the maxillary central incisors with the aid of a mini-implant and segmented wires. In 2010, Lin et al [5]. Introduced a combined technique using skeletal anchorage to manage the vertical dimension and correct gummy smiles of skeletal origin in adult patients with long faces.
The present study aimed to investigate the application of improved super-elastic Ti-Ni alloy wire (ISW) in growing adolescent patients presenting with an Angle Class II malocclusion with large overjet. ISW was considered a clinically useful, effective, simple non-surgical strategy for the treatment of Angle Class II malocclusion.
Case Report
A 13-year-old female came to our clinic with a chief complaint of poor dental alignment and bucked teeth. She refused to have any surgery correction for her skeletal problem. She also denied any major systemic diseases or drug allergies and was considered to be healthy.
Clinical Findings
Clinical examination depicted a skeletal Class II malocclusion with a convex profile and vertical maxilla excess. The patient showed 12.0mm overjet and molars had a Class II dental relationship (Figure 1).
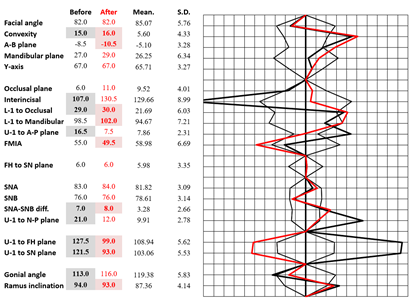
The cephalometric analysis also confirmed the Class II malocclusion with upper incisor protrusion as the main cause (SNA= 83.0 ◦, SNB= 76.0 ◦, ANB= 7.0 ◦) (Figure 2). Vertical relations showed normal mandibular plane angle (FMA= 19.3◦) and the patient had extremely proclined maxillary incisors (U1 to FH= 127.5◦) (Table 1).
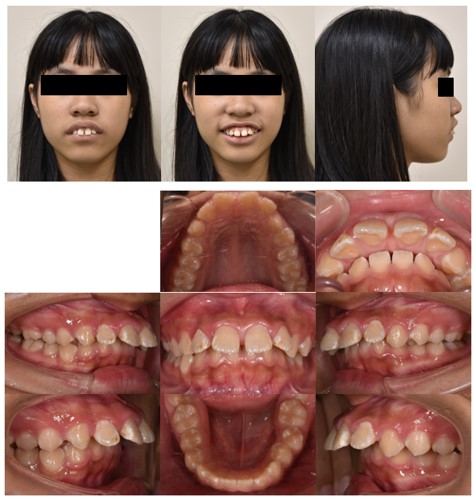
Figure 1: Pretreatment facial and intraoral photographs (13y 0m old).
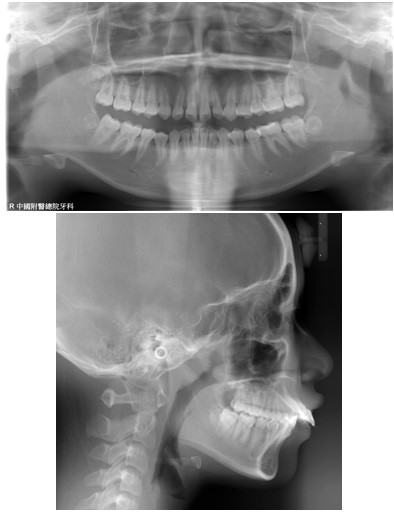
Figure 2: Pretreatment panoramic, lateral cephalometric radiographs (13y 0m old).
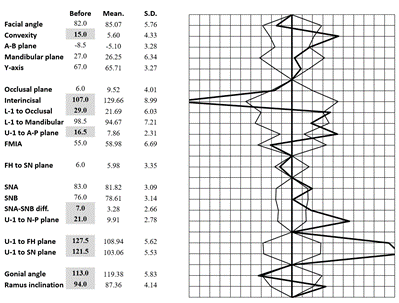
Table 1: Polygon- Before active treatment.
Treatment Objectives
In this patient, Class II malocclusion with large overjet and gummy smile can be noted, and we want to achieve an ideal occlusion of the bilateral Angle’s Class I canine and molar relationship, as well as to correct scissors bite over lower left molar area.
Our treatment objectives were (1) to relieve crowding and eliminate the occlusal interference, (2) to attain an ideal overbite and overjet, (3) to achieve better arch coordination and interdigitation.
Treatment Alternatives
If this patient desires to improve appearance, especially in patients with skeletal class II with vertical maxillary excess and mandible retrognathism, orthognathic surgery should always be first considered. To relieve crowding of lower dentition and decompensate the flaring upper incisors, upper and lower first premolars was needed to be extracted. Le Fort I osteotomy over maxilla and bilateral sagittal split ramus osteotomy (BSSRO) over mandible can correct the sagittal and vertical skeletal discrepancy.
In non-surgery situation, we would apply upper bicuspid extraction protocol to retract her severely proclined upper incisors. We would use temporary anchorage device to achieve maximum anchorage and ISW intrusion arch technique to correct gummy smile and inclination of upper incisors. However, this approach will also compromise the facial appearance. The patient declined the proposal of orthodontic treatment combined with surgery. Therefore, our patient agreed to undergo orthodontic treatment for dental camouflage.
Treatment Progress
After thorough explanation and discussion of the treatment options, the patient agreed to have orthodontic treatment without surgical approach. Before orthodontic treatment, upper first premolars were extracted. Full mouth DBS was done with preadjusted edgewise metal brackets, Micro-arch, Roth type (Tomy company, Tokyo, Japan).
By then, the preliminary leveling and alignment in both arches were gradually achieved. We used stopper and elastic chain for #35 de-rotation (Figure 3). The anterior bite turbo was bonded to correct deep overbite (Figure 4). With anterior bite turbo, we also can eliminate interference of occlusion to correct scissors bite over lower left molar region.
We used temporary anchorage devices to retract upper incisors and preventing upper molars from protraction. (Figure 5) And then, we also used intrusion arch technique with temporary anchorage devices to intrusion upper incisors and correct both gummy smile and deep overbite (Figure 6). After 36 months active treatment, full mouth bracket was deboned.
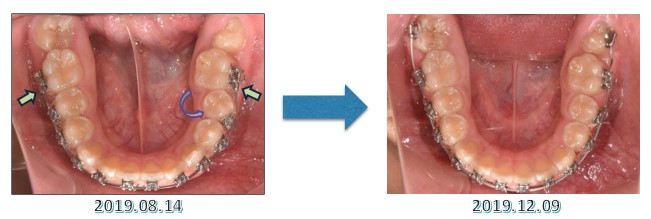
Figure 3: Progressive intraoral photographs (12 months).
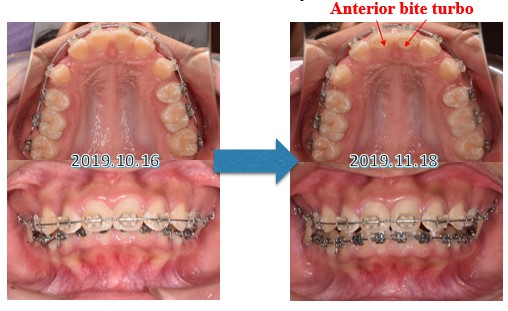
Figure 4: Progressive intraoral photographs (14 months).
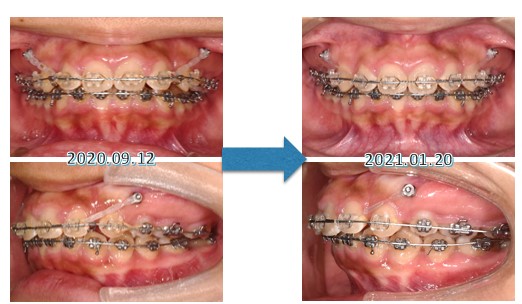
Figure 5: Progressive intraoral photographs (24 months).

Figure 6: Progressive intraoral photographs (29 months).
Results
After 36 months of therapy, adequate overbite, overjet and coordinated dental midline were achieved. The facial profile of the patient was greatly improved. Before orthodontic treatment, the patient’s both upper and lower lip was protrusive to the esthetic line. After orthodontic treatment, we could find out that both the patient’s upper lip and lower lip are on the esthetic line. Overall, the patient was satisfied with her profile improvement and smile arc (Figure 7).
The cephalometric analysis indicated almost all parameters had greatly improved (Figure 8). Due to anterior bite turbo and molar extrusion, mandibular plane angle was increased (27.0°→29.0°) (Figure 9, Table 2).
Because patient refused to accept invasive surgery, we can only correct the anteroposterior relationship with camouflage. At the end of treatment, we gave the patient a circumferential retainer at the upper arch, a Hawley retainer at the lower arch, and an auxiliary clear plastic retainer for retention.

Figure 7: Post-treatment facial and intraoral photographs (16y 01m old).
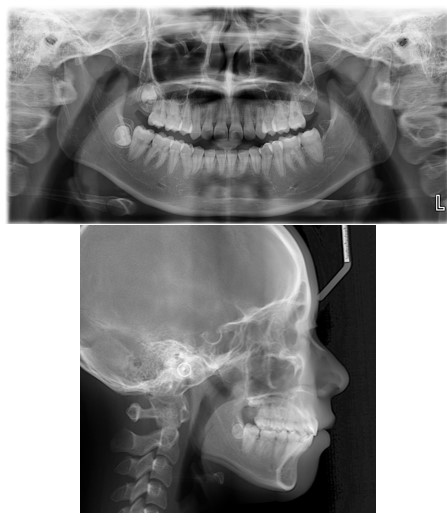
Figure 8: Post panoramic, lateral cephalometric radiographs (16y 01m old).
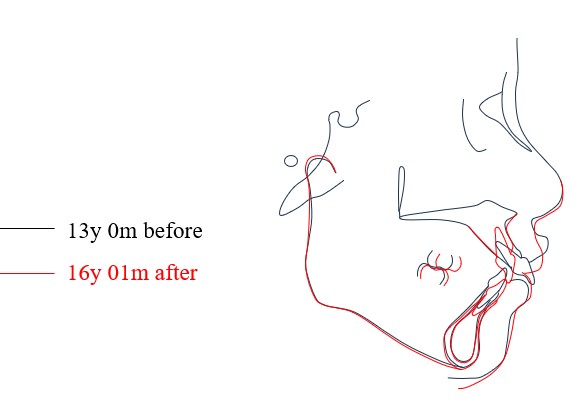
Figure 9: Superimposition of pretreatment and post-treatment.
Table 2: Polygon-Before and after active treatment.
Discussion
The correction of Gummy Smiles (GS) has garnered significant attention in orthodontic literature due to its multifaceted impact on patients' aesthetics and psychological well-being. A gummy smile, characterized by the exposure of more than 2 mm of gingiva, can lead to diminished self-confidence and altered social interactions. Various etiologies contribute to this condition, including altered passive eruption of teeth, dentoalveolar extrusion, vertical maxillary excess, and hyperactive or short upper lip muscles. Effective management of a gummy smile necessitates a thorough understanding of its underlying causes to tailor appropriate treatment plans [4,5].
To correct scissors bite, torque control of upper and lower molars are substantially important. We used # 47 bracket at tooth 27 and # 37 bracket upside down at tooth 37 for torque control. In the meantime, we used vertical offset to eliminate occlusal interference (Figure 10).
Rotated tooth is always regarded a malocclusion that requires management by an orthodontist. A rotated premolar might lead to some occlusal problems in mastication. There are many ways to de-rotate a single tooth. In this case, we used stoppers mesial to tooth 36 for anchorage reinforcement, together with the use of elastic chain to have tooth 35 de-rotated (Figure 11).
One of the major challenges while treating Class II malocclusion is correction of deep overbite. We used anterior bite turbo for immediate bite opening and for flattening lower Curve of Spee. Without occlusal interference, we could correct scissors bite and perform de-rotation much more easily. In the meantime, we used long Class II intermaxillary elastics to extrude the posterior teeth, and reverse ISW Curve to flare out and intrude the lower anterior teeth (Figure 12).
For gummy smile treatment, we might perform “intrusion of the upper anterior teeth” to correct. With intrusion arch technique and Temporary Anchorage Device (TAD’s), we could control the amount of intrusion more precisely. (Figure 13).
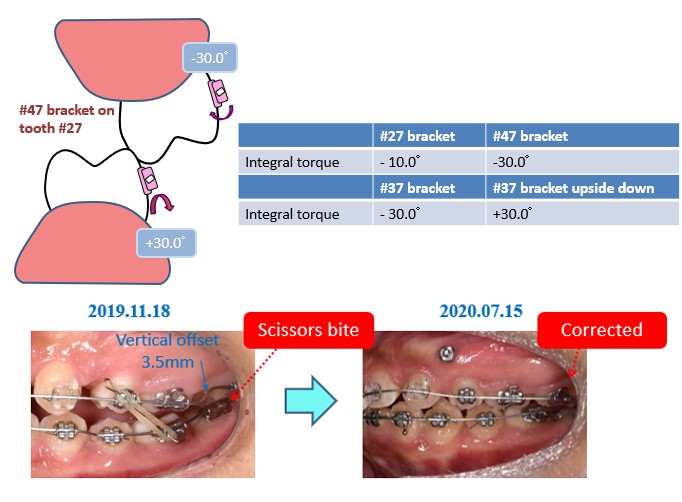
Figure 10: Scissors bite correction.
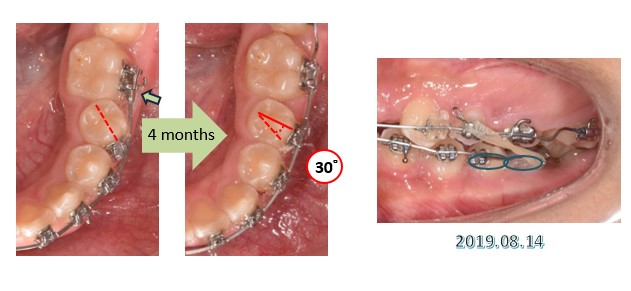
Figure 11: Tooth 35 de-rotation.

Figure 12: Anterior bite turbo for deep overbite correction.
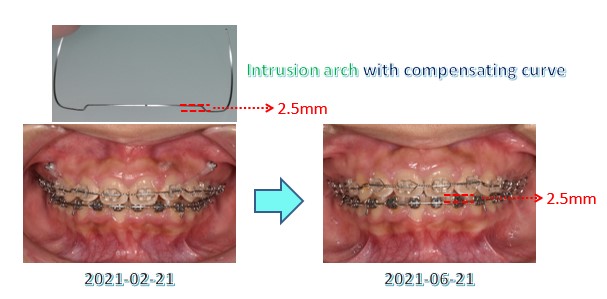
Figure 13: Intrusion arch technique.
Conclusion
In this case, we corrected poor dental alignment by rapid leveling and intrusion arch technique of using ISW and temporary anchorage devices. ISW can provide an efficient and easy approach to correct this particular malocclusion. After 36 months of treatment, a desirable esthetic outcome was achieved. This patient was pleased with the final treatment result.
References
- Miura F, Mogi M, Okamoto Y. New application of super elastic NiTi rectangular wire. J Clin Orthod, 1990; 24(9): 544-552.
- Miura F, Mogi M, Ohura Y, Hamanaka H. The super-elastic property of the Japanese NiTi alloy wire for use in orthodontics. Am J Orthod Dentofacial Orthop, 1986; 90(1): 1-10.
- Iramaneerat K, Hisano M, Soma K. Dynamic analysis for clarifying occlusal force transmission during orthodontic archwire application: difference between ISW and stainless-steel wire. J Med Dent Sci, 2004; 51(1): 59-65.
- Kim TW, Kim H, Lee SJ. Correction of deep overbite and gummy smile by using a mini-implant with a segmented wire in a growing Class II Division 2 patient. Am J Orthod Dentofacial Orthop, 2006; 130: 676–685.
- Lin JC, Liou EJ, Bowman SJ. Simultaneous reduction in vertical dimension and gummy smile using miniscrew anchorage. J Clin Orthod, 2010; 44(3): 157-170.

