Reconstruction of the Columella in Children: Case Reports of 4 Patients
Fadoua Boughaleb1,2,*, Assia Mouad1,2, Ismail Benomar1,2, Mohamed Rami2, Mohamed Elamine Bouhafs2 and Nawfal Fejjal1,2
1Paediatric plastic Surgery unit - Children's Hospital of Rabat, Morocco
2Faculty of medecine and pharmacy, University Mohammed V, Rabat, Morocco
Received Date: 26/05/2024; Published Date: 01/10/2024
*Corresponding author: Fadoua Boughaleb, Pediatric Surgery Department, Children’s Hospital of Rabat, Ibn Sina University Hospital, Faculty of medecine and pharmacy, University Mohammed V, Rabat, Morocco
Abstract
Introduction: The columella is an important centrofacial aesthetic entity. The substance defect at this level can result from multiple causes and leads to significant functional and psychosocial problems; repairing it is very difficult and must be subject to precise aesthetic imperatives. The ideal reconstruction technique must recreate the contour of the columella, ensure the projection of the nasal tip and maintain the patency of the external valve. The pigmentation and texture of the nasal skin must also be considered, while minimising the morbidity of the donor site.
Patient and Method: A clinical study were carried out on four patients presenting an acquired columellar defect who had undergone reconstruction at the paediatric plastic surgery unit of the children's hospital of Rabat, Morocco.
Results: Four patients aged between 18 months and 16 years old, with a history of prematurity, presenting an acquired columellar defect. The patients had no nasal obstruction or functional limitations. The composite auricular graft was performed in two children, the inferior pedicle nasogenian flap in one child and a double alar margin flap in the fourth. The aesthetic result was considered satisfying by all patients.
Conclusion: The repair of columellar defect is the result of a special alchemy combining anatomical knowledge, artistic sensitivity and surgical technique.
Keywords: Columella; Columellar defect; Reconstruction; Children
Introduction
The columella is an important centrofacial aesthetic entity. It refers to the tissue that links the nasal tip to the nasal base while dividing the nares [1]. Functionally and aesthetically, the columella plays a significant role at the lower border of the nasal septum. The defect at this level can result from multiple causes such as infection, trauma, malignancy, surgical excision of tumors, or may manifest congenitally and leads to significant functional and psychosocial problems [2,3]. We present a case study involving four patients presenting acquired columellar defect.
Patients and Methods
A clinical study was carried out from January 2017 to December 2023 on children under 18 years old presenting an acquired columellar defect who had undergone reconstruction at the paediatric plastic surgery unit of the children's hospital of Rabat, Morocco.
Results
Our study is about four patients,
- two girls aged 7 and 16 years old.
- two boys aged 18 months old and 4 years old.
All the patients had a history of prematurity and requiring several weeks of CPAP assistance in the neonatal intensive care unit, they had necrosis of the columella region related to compression by the intubation tube during the neonatal period, which had progressed to retractile scarring and loss of columella tissue. The patients presented no nasal obstruction or functional limitations.
- For the 4 years old boy who had a deep columellar defect extending to the nasal septum, we opted for an inferior pedicle nasogenian flap. The patient retained a slight obstruction of the right nostril, which will subsequently benefit from degreasing (Figure 1).
- The 16 years old girl presented a superficial columellar defect and underwent a double alar margin flap, with a good healing in 6 months (Figure 2).
- The 7 years old girl (Figure 3) and the 18 months infant had a deep columellar defect extending to the nasal septum, so we performed a composite auricular graft. The aesthetic result for the girl was satisfying after 6 months, while the infant required a 2nd composite graft to fill the defect.
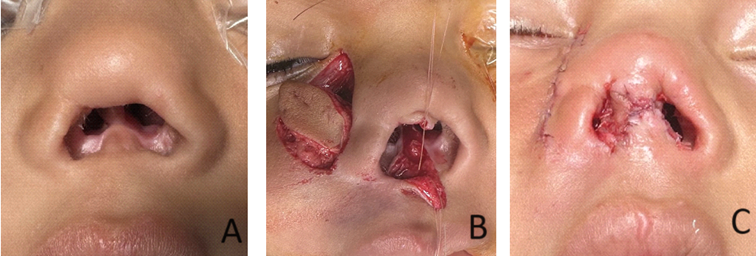
Figure 1: Images showing the nasogenian flap used in a deep columellar defect in our 4 years old boy (A: before surgery, B: peroperative view, C: postoperative result).
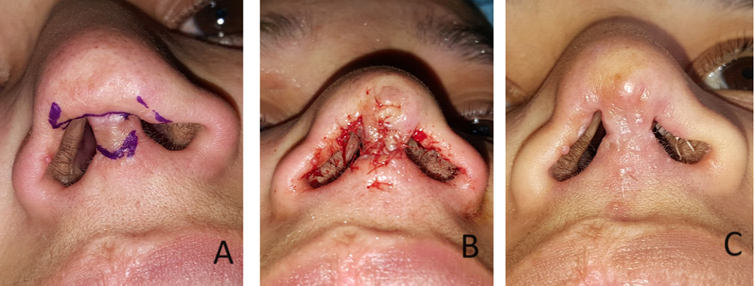
Figure 2: Images showing the double alar margin flap in our 16 years old patient (A: before surgery, B: peroperative view, C: 6 months follow-up result).
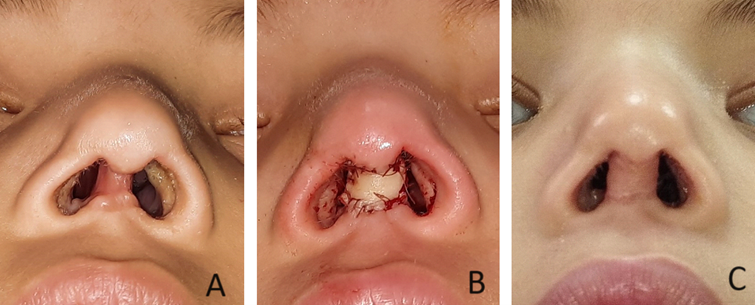
Figure 3: Images showing the composite auricular graft used in our 7 years old girl (A: before surgery, B: peroperative view, C: 6 months follow-up result).
Discussion
Several techniques have been described in the literature for columellar reconstruction. These methods encompass skin grafting, composite grafting, and various types of local flaps [4]. Nevertheless, the visibility of donor site scarring resulting from these techniques might be as prominent as the initial defect, contingent upon factors such as the patient's age [4,5]. In children, labial and nasofacial incisions are particularly difficult to conceal [4,6].
The literature discusses various techniques for columellar reconstruction, such as full-thickness skin grafts, local random pattern flaps, regional flaps, and composite grafts. Direct primary closure and skin grafts are seldom suitable, except for superficial defects. Flap coverage, often requiring adjunctive cartilage or composite grafts, is frequently necessary due to the composite nature of the columella. Chondrocutaneous auricular composite grafts are effective for providing cartilaginous support with compatible, non-hair-bearing skin [7,8]. These grafts are useful for columellar defects, although meticulous technique and ideal conditions are crucial for success. Local random pattern flaps offer advantages in terms of vascularization, with various options described for columellar reconstruction, including upper lip flaps, alar margin flaps, and nasal septal flaps, among others. Regional flaps, such as the forehead flap, may be utilized when local tissue is insufficient [9].
Composite flap procedures, like the preauricular flap, provide both external coverage and internal support without relying on a well-vascularized bed [10,11]. The optimal reconstructive approach depends on factors such as the cause of the defect, the involved components of the columella, and donor site availability [9].
For isolated columellar defects without significant scarring or vascular compromise, a 2-stage reconstruction with bilateral nasal sill flaps coupled with an auricular composite graft is recommended [12]. This approach involves forming the external columellar outline with nasal sill flaps in the first stage, followed by placement of a chondrocutaneous graft from the helical root to enhance the desired contour of the new columella in the second stage. This method is particularly suitable for patients with high aesthetic demands willing to undergo multiple stages for optimal results. The resulting scars are camouflaged, and the procedure addresses both functional and aesthetic concerns [9,13,14].
Potential complications of all columellar reconstruction procedures include partial or complete graft or flap loss, scar contracture, and contour abnormalities. These complications can lead to decreased tip projection, compromised airway patency, and unsatisfactory aesthetic outcomes. Graft survival is primarily determined by size, with general consensus suggesting that grafts larger than 10 mm are unsuitable for nasal reconstruction due to metabolic demands and recipient site vascularity [9]. Some studies have proposed postoperative cooling to improve graft survival by reducing metabolic requirements, but the evidence supporting this is limited [15]. Additionally, to account for inevitable contraction, the harvested graft should be slightly larger than the columellar defect. Transient narrowing of the nasal base and decreased tip projection may occur postoperatively, but typically resolve over time [14].
Conclusion
The reconstruction of columellar loss of substance requires a unique blend of anatomical understanding, artistic perception, and surgical skill.
Conflict of interests: The authors have no conflict of interests to declare.
References
- Hennekam RC, Cormier-Daire V, Hall JG, Méhes K, Patton M, Stevenson RE, Elements of morphology: standard terminology for the nose and philtrum, Am. J. Med. Genet. Part A, 2009; 149(1): 61–76.
- Ayhan M, Sevin A, Aytug Z, Gorgu M, Erdogan B. Reconstruction of congenital and acquired columellar defects: clinical review of 38 patients, J. Craniofac. Surg, 2007; 18(6): 1500–1503.
- Mavili ME, Akyürek M. Congenital isolated absence of the nasal columella: reconstruction with an internal nasal vestibular skin flap and bilateral labial mucosa flaps, Plast. Reconstr. Surg, 2000; 106(2): 393–399.
- Sherris DA, Fuerstenberg J, Danahey D, Hilger PA. Reconstruction of the nasal columella. Arch Facial Plast Surg, 2002; 4: 42–46.
- Di Santo D, Trimarchi M, Galli A, Bussi M. Columella reconstruction with an inferiorly-based philtral advancement flap in a cocaine abuser. Indian J Plast Surg, 2017; 50: 96–99.
- Demir Z, Ozdil K, Karamursel S, Yuce S, Oktem F, Celebioglu S. Reconstruction of the columella with bilateral nostril sill flaps. Ann Otol Rhinol Laryngol, 2006; 115: 239–242.
- Brown JB, Cannon B: Composite free grafts of two surfaces of skin and cartilage from the ear. Ann Surg, 1946; 124: 1101-1107.
- Maves MD, Yessenow RS. The use of composite auricular grafts in nasal reconstruction. J Dermatol Surg Oncol, 1988; 14: 994-999.
- Pan Kristen S, Brian S Pan. "Columellar reconstruction in children." Operative Techniques in Otolaryngology-Head and Neck Surgery, 2018; 29(2): 61-65.
- Liu F, Xu H, Wang T, et al. Columella lengthening by a vascularized preauricular flap. Aesthetic Plast Surg, 2013; 37: 232-239.
- Benito-Ruiz J, Raigosa M, Yoon TS. Columella reconstruction using a free flap from the first web space of the foot. Ann Plast Surg, 2012; 69: 279-282.
- Pan BS, Vu AT, Rapp SJ, et al. Reconstruction of the isolated columellar defect: A novel 2-stage technique and review of the literature. J Oral Maxillofac Surg, 2017; 75: 822-827.
- Cronin TD. Lengthening columella by use of skin from nasal floor and alae. Plast Reconstr Surg Transplant Bull, 1958; 21: 417-426.
- Demir Z, Ozdil K, Karamursel S, et al. Reconstruction of the columella with bilateral nostril sill flaps. Ann Otol Rhinol Laryngol, 2006; 115: 239-242.
- Conley JJ, Vonfraenkel PH. The principle of cooling as applied to the composite graft in the nose. Plast Reconstr Surg, 1946; 17: 444-451.

