Efficacity of Endourologic Management for Ureteral Stenosis in Renal Transplant Patient
Doumer A, Safwate R*, Seffar A, Moataz A, Dakir M, Debbagh A and Aboutaeib R
Urology Departement, IBN Rochd University Hospital, Casablanca, Morocco
Received Date: 26/03/2024; Published Date: 01/10/2024
*Corresponding author: Safwate Reda, Urology Departement, IBN Rochd University Hospital, El Azhari 2 Rue 41 N°145 El Oulfa. Casablanca, Morocco
Abstract
Ureteral Stenosis (US) is a commun complication in Kidney Tansplant (KT) patients, usually appears within 3 months of surgery. The constant development of endoscopic techniques in urology has made it possible to manage this complication using an endoscopic approach. In this observation, we present the case of a 58-year-old patient who underwent renal transplantation. The immediate postoperative course was unremarkable, but 2 months later the patient developed pain in the right iliac fossa (transplant site). A CT scan revealed ureterohydronephrosis without any passage of contrast product into the bladder, with stenosis of the terminal part of the ureter.
Keywords: Ureteral stenosis; Kidney transplant; Endoscopic; JJ descent
Introduction
Ureteral Stenosis (US) occurs in approximately 5% of Kidney Transplant (KT) patients, rising to 10% within 5 years [1]. This condition stands out as the most prevalent long-term urological complication [2]. Consequently, prompt diagnosis and intervention are essential.
US becomes apparent within the initial 3 months after KT and is chiefly attributed to ureteral ischemia.
The primary treatment for these patients has been the open surgical approach, particularly in instances of complex, mid-third, or proximal ureteral stenosis (US) [3,4]. This method is favored for its connection to improved renal graft survival [5]. While surgical reconstruction has evolved with the introduction of robot-assisted US repair, even minimally invasive approaches may carry non-negligible complications [6]. With recent advancements in endourological instrumentation, an endoscopic approach utilizing percutaneous balloon dilatation or flexible antegrade ureteroscopy and holmium laser incision has emerged as a viable alternative for stenosis measuring less than 3 cm.
Objective: Our aim was to assess the efficacy and safety of endourological interventions in managing Ureteral Stenosis (US) among Kidney Transplant (KT) patients.
Case Report
Mr A.B, aged 57 years, father of 4 daughters, Chronical Kidney Disease with Hemodialysis since 2016 with 3 sessions per week on right radial arteriovenous fistula.
Clinical examination: weight 73kg, height 175cm => BMI 22.9kg/m2
No residual diuresis, rest of examination unremarkable.
Ultrasound showed small kidneys And the CT scan a bilateral polycystic kidney disease on nephritic kidneys.
The Donor was a 58 years old male with no particular history, victim of a stroke causing severe brain injuries, renal function at the time of collection was 5.4 g/l of plasmatic creatinine.
The Graft exploration revealed a single artery and a single vein, The cold ischemia time was 17H33, the warm ischemia time 01H30 with a venous time of 40min and an arterial time of 39min.
We observed a delayed recovery of graft function, the patient began to resume diuresis from day 11, with progressive improvement in renal function.
During the 21th day, the patient presented with sudden anuria and then resumed diuresis.
The JJ catheter was removed after 52 days post renal transplantation.
The patient's diuresis subsequently stopped at 60 days with pain in the right iliac fossa, Examination showed a conscious, stable patient, no oedema, tenderness in the right iliac fossa, at the biology the renal function slightly reduced and CT scan revealed a renal graft of normal size, secreting and excreting within normal timescales, site of uretero pyelo caliciale dilatation with stenosing retraction of the terminal part of the ureter (Figure 1).
The patient was taken to the surgery room and underwent endoscopic treatment with ureterectomy and descent of the JJ by anterograde visualization (Figure 2).
Satisfactory post-operative outcome
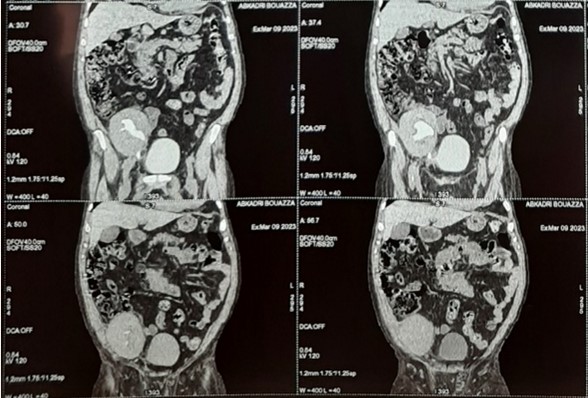
Figure 1: CT scan images showing the ureteral stenosis.
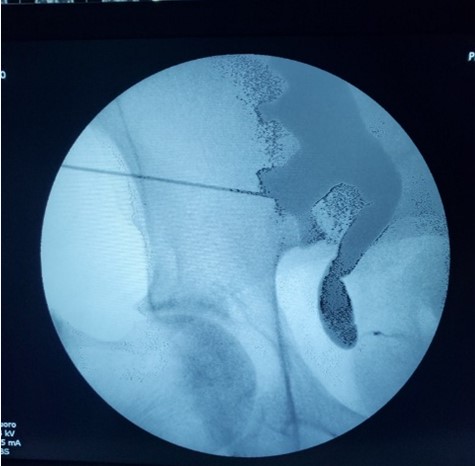
Figure 2: Renal and ureteral anterograd opacification before the stent descent.
Discussion
Presently, selecting the most effective treatment for Ureteral Stenosis (US) in Kidney Transplant (KT) patients remains a topic of ongoing debate. While minimally invasive approaches have been employed for over 30 years [5], their significance has been revitalized with the advent of new technologies, particularly the utilization of various lasers in endourology [4].
Kristo et al. [2] reported a 100% success rate with a median follow-up of 24 months, but it's important to note that their study focused solely on short ureteral stenoses (US) with an average length of 2.8 mm. In our study, we extended the scope to include longer US with a median length of 10 mm
in contrast, previous studies have reported success rates for surgical reconstruction around 77% [6], which is comparable to the success achieved through endoscopic management.
However, surgical reconstruction tends to involve more intricate strictures and cases that have already proven resistant to endoscopic interventions—over half of the cases in our study had previously failed balloon dilation
A recent systematic review, encompassing 34 studies and 385 patients with distal ureteral strictures after kidney transplant, indicated success rates for surgical reconstruction reaching as high as 85.4% when utilized as the primary treatment and up to 93.1% as a secondary treatment following unsuccessful endoscopic interventions. In the same study, the endourological approach exhibited success rates of 64.3% and 75.5% for primary and secondary treatments, respectively. [7,8]
In 2017, Gil-Sousa et al. [5] presented a comprehensive 10-year experience at a single center regarding Ureteral Stenosis (US) after Kidney Transplantation (KT). Their study covered both reconstructive and endoscopic treatments, revealing no significant differences based on the length of stenosis, the duration between transplant and stenosis occurrence, or the location of the stenosis. However, a notable trend emerged, indicating a higher success rate for stenosis measuring less than 1.5 cm and early management within 3 months, particularly when utilizing balloon dilatation—findings consistent with our results.
Concurrently, He et al. [10], in line with considerations of stenosis length, proposed a classification system for US with three grades: (1) graft function deterioration and hydronephrosis on ultrasound without an obvious stricture on a pyelogram; (2) focal (< 1 cm) distal ureteral stenosis at the ureteral anastomotic site; and (3) long segment (> 1 cm) distal ureteral stenosis extending to the proximal ureter or pelvis.
Juaneda et al. [11] conducted a study that revealed a correlation between a short time to diagnosis after kidney transplantation (KT) and a previous acute rejection episode, predicting the success of endourological treatment for ureteral strictures. These findings align closely with our own results, where early-onset stenosis (within the first 3 months) was associated with the success of endoscopic management.
At present, the European Association of Urology (EAU) guidelines on Kidney Transplantation (KT) offer recommendations for ureteral stenosis (US) management, taking into account factors such as timing, stricture anatomy (including length and location), patient characteristics, and surgeon preferences [10]. However, the guidelines do not currently address the shape of the stenosis and its potential impact on the success rate of endoscopic treatment for US.
Notably, a study by Gaya et al. [13] in 2023 provides a rationale for considering stenosis shape. The study found that ureteroenteric anastomotic strictures were more likely to be successfully managed endoscopically when the strictures were less than 1 cm (16.8% vs. 4.4%, p < 0.001) and exhibited a duckbill-shaped configuration (16.7% vs. 3.1%, p < 0.001). This aspect of stenosis shape could be a valuable consideration in refining guidelines for optimizing the success of endoscopic management in US cases.
Conclusion
Given the satisfactory long-term outcomes and the safety profile of these procedures, we advocate for considering endoscopic treatment as the primary therapeutic option for specific Kidney Transplant (KT) patients experiencing Ureteral Stenosis (US). Particularly, individuals with a short and duckbill-shaped stenosis diagnosed within 3 months of KT appear to be the most suitable candidates for this approach.
Conflicts of interest: The authors declare no conflicts of interest.
References
- Kinnaert P, Hall M, Janssen F, Vereerstraeten P, Toussaint C, van Geertruyden J. Ureteral stenosis after kidney transplantation: true incidence and long-term followup after surgical correction. J Urol, 1985; 133: 17–20.
- Kristo B, Phelan MW, Gritsch HA, Schulam PG. Treatment of renal transplant ureterovesical anastomotic strictures using antegrade balloon dilation with or without holmium:YAG laser endoureterotomy. Urology, 2003; 62: 831–834.
- Praz V, Leisinger HJ, Pascual M, Jichlinski P. Urological complications in renal transplantation from cadaveric donor grafts: A retrospective analysis of 20 years. Urol Int, 2005; 75: 144–149.
- Deininger S, Nadalin S, Amend B, Guthoff M, Heyne N, Königsrainer A, et al. Minimal-invasive management of urological complications after kidney transplantation. Int Urol Nephrol, 2021; 53: 1267–1277.
- Gil-Sousa D, Oliveira-Reis D, Teves F, Príncipe P, Castro- Henriques A, Soares J, et al. Ureteral stenosis after renal transplantation-a single-center 10-year experience. Transplant Proc, 2017; 49: 777–782.
- Arpali E, Al-Qaoud T, Martinez E, Redfield RR, Leverson GE, Kaufman DB, et al. Impact of ureteral stricture and treatment choice on long-term graft survival in kidney transplantation. Am J Transplant, 2018; 18: 1977–1985.
- Buffi NM, Lughezzani G, Hurle R, Lazzeri M, Taverna G, Bozzini G, et al. Robot-assisted surgery for benign ureteral strictures: experience and outcomes from four tertiary care institutions. Eur Urol, 2017; 71: 945–951.
- Streem SV, Novick AC, Steinmuller DR, Zelch MG, Risius B, Geisinger MA. Long-term efficacy of ureteral dilation for transplant ureteral stenosis. J Urol, 1988; 140: 32–35. https://doi.org/10.1016/ S0022-5347(17)41477-7.
- Kwong J, Schiefer D, Aboalsamh G, Archambault J, Luke PP, Sener A. Optimal management of distal ureteric strictures following renal transplantation: a systematic review. Transpl Int, 2016; 29: 579–588.
- He B, Bremner A, Han Y. Classification of ureteral stenosis and associated strategy for treatment after kidney transplant. Exp Clin Transplant, 2013; 11: 122–127. https:// doi.org/10.6002/ECT.2012.0179.
- Juaneda B, Alcaraz A, Bujons A, Guirado L, Díaz JM, Martí J, et al. Endourological management is better in earlyonset ureteral stenosis in kidney transplantation. Transplant Proc, 2005; 37: 3825–3827.
- Breda A, Budde K, Figueiredo A, Lledó García E, Olsburgh J, Regele H, et al. Renal Transplantation EAU Guidelines on, 2022.
- Gaya JM, Territo A, Basile G, Gallioli A, Martínez C, Turco M, et al. Optimizing decision-making process of benign uretero-enteric anastomotic stricture treatment after radical cystectomy. World J Urol, 2023; 41.

