Acute Intestinal Occlusion Due to a Double Location Gastric and Ileal Trichobezoar
Essaidi Z, Barigou Y*, Majd A, Bouali M, El Bakouri A, Bensardi F, Elhattabi K and Fadil A
Department of Medicine, Faculty of medicine and pharmacy Casablanca, Morocco
Received Date: 11/04/2024; Published Date: 30/09/2024
*Corresponding author: Youssef Barigou, Department of Medicine, Faculty of medicine and pharmacy Casablanca, Morocco
Abstract
Trichobezoar is a rare condition that typically results from the accumulation of hair in the stomach and is often associated with psychiatric disorders.
In this article, we report the case of a 27-year-old female patient who presented to the emergency department with signs of bowel obstruction, including cessation of bowel movements and gas, accompanied by bilious vomiting, diffuse abdominal pain.
A CT scan revealed ileal distension upstream of an intraluminal formation of heterogeneous mixed density with air bubbles, and a second gastric formation with similar characteristics, suggesting a double localization of the bezoar.
The patient underwent surgery, during which two trichobezoars were extracted, one located in the ileum 2.20 meters from the duodenojejunal junction and the other in the stomach.
The postoperative course was uneventful, and the patient was referred for psychiatric follow-up upon discharge.
Keywords: Trichobezoar; Gastric obstruction; Ileal obstruction; CT; Acute intestinal obstruction
Introduction
Trichobezoar is a rare condition [1], resulting from the ingestion of hair, fur, or fibers from carpets or rugs [2].
Cases of double gastric and intestinal localization have been reported in the literature [3].
In this article, we report a case of trichobezoar occlusion with double gastric and ileal localization in a 27-year-old female patient.
Case Report
A 27-year-old patient presented to the emergency department with symptoms of bowel obstruction, including cessation of bowel movements and gas, bilious vomiting and diffuse abdominal pain. On examination, she had a distended and tympanic abdomen, with palpation revealing a firm mobile mass in the epigastric region measuring approximately 10 cm in diameter.
An emergency abdominal X-RAY showed hydro-aerial levels.
This was supplemented by an abdominal CT scan, which revealed significant distension of the intestinal bowel loops (diameter 50 mm) with hydro-aerial levels, upstream of a transitional level with an intraluminal formation. This formation, oval-shaped and well-defined, exhibited heterogeneous mixed pseudo-fatty density, containing air bubbles, measuring 51 x 36 mm and extending over 60 mm, consistent with a bezoar. A similar formation was identified in the gastric region, measuring 82 x 45.5 mm and extending over 100 mm.

Figure 1: plain abdominal radiography showing hydroaerial levels.
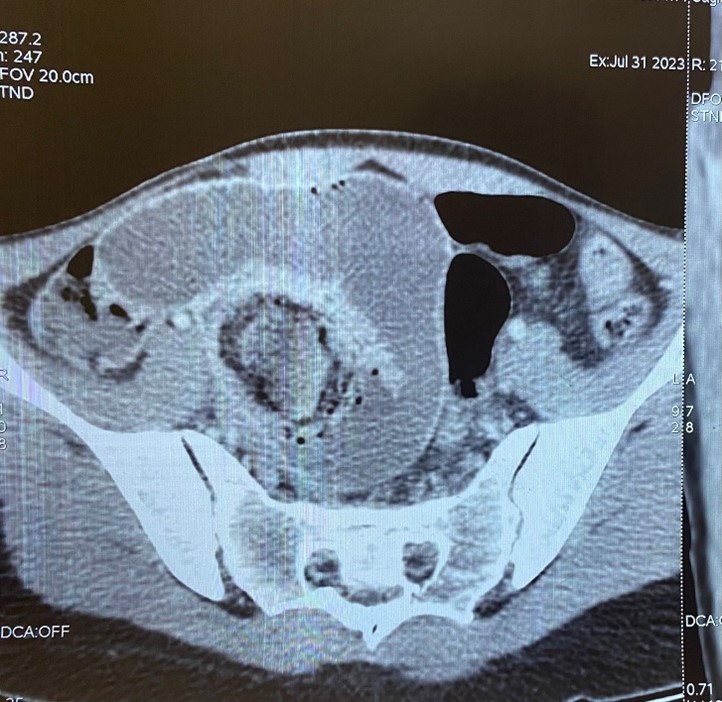
Figure 2: CT image of intestinal endoluminal formation (bezoar).
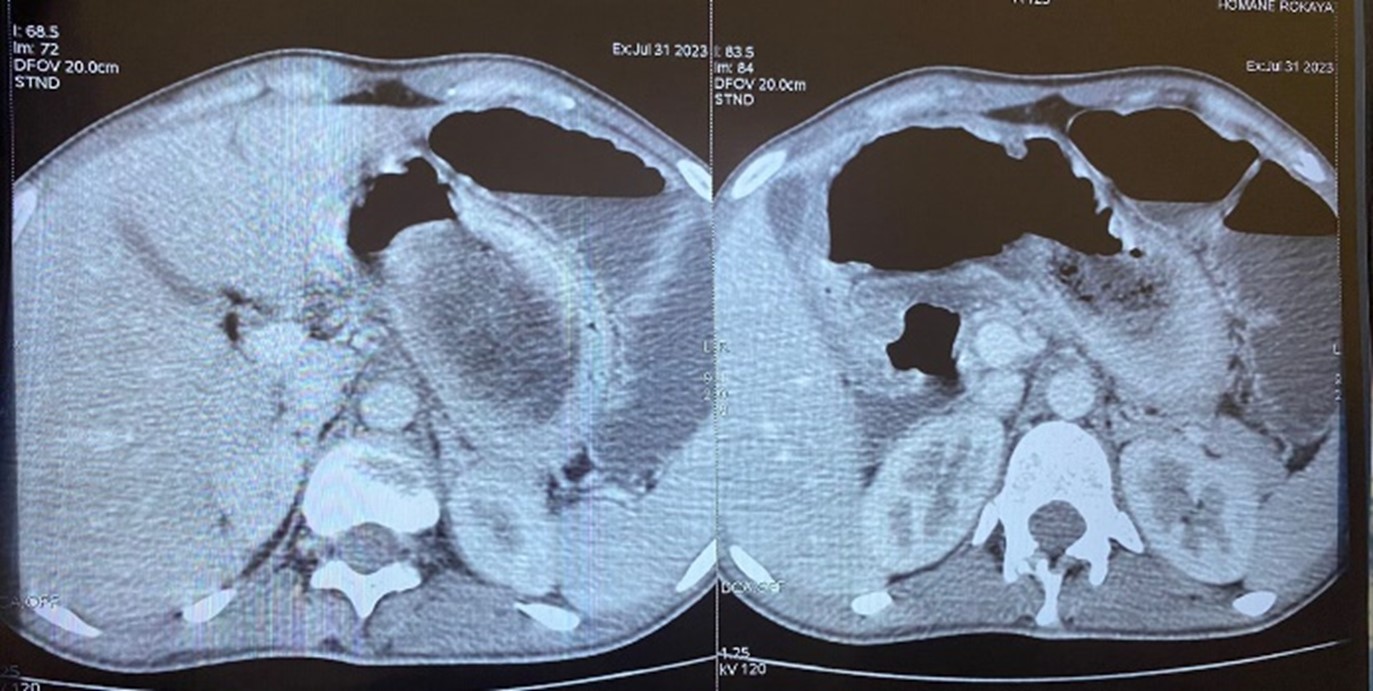
Figure 3: CT image of intra-gastric formation (bezoar).
The patient reported that she had suffered from trichophagia since childhood.
The patient was admitted to the surgical emergency department, where laboratory tests revealed a hemoglobin level of 16.7 g/dl and normal electrolyte levels.
She underwent exploratory laparotomy, which confirmed the presence of two trichobezoars: one located at the duodenojejunal angle measuring 5 cm in diameter at 2.20 meters, causing a 5 cm upstream intestinal distension, and the other measuring 12 cm in diameter in the stomach.
Both trichobezoars were surgically removed, and the patient's postoperative course was uneventful, and the patient was subsequently referred for psychiatric treatment.

Figure 4: Image of intra-intestinal trichobezoar.

Figure 5: Image of the dual location of the trichobezoar in the gastric and intestinal tracts.
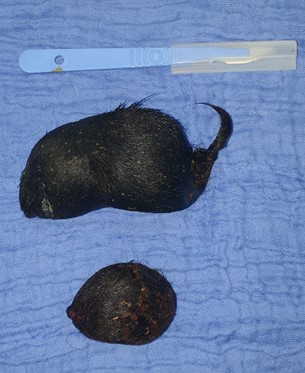
Figure 6: Image of both trichobezoars after extraction.
Discussion
Trichobezoar is the most common form of bezoar, accounting for 0.15% of gastrointestinal foreign bodies, with a strong female predominance and peak incidence between the ages of 10 and 19 [4].
It is often associated with psychiatric disorders [4].
Diagnosis can be difficult due to its low prevalence [4].
Trichobezoar is a rare cause of acute intestinal obstruction.
Symptoms vary depending on the location of the bezoar, with the most frequent location being gastric [1], although a double location may be found in a few patients.
Symptoms of bezoar are anorexia, epigastric discomfort, nausea, vomiting, progressive intolerance to solid foods, weight loss and weakness, when food can still bypass the bezoar. However, symptoms usually develop gradually and insidiously, and the diagnosis is made many years after the onset of trichotillomania [5].
A complication may be the mode of revelation of this pathology. These may include upper digestive haemorrhage due to parietal ulceration, gastric or intestinal mechanical obstruction, gastric or intestinal perforation with peritonitis or subphrenic abscess, digestive fistula [6].
Clinical examination may reveal a patch of alopecia in some cases, but in the majority of cases a well-limited, smooth, firm, painless, mobile, non-pulsatile epigastric mass [2].
Diagnosis can be confirmed in a number of ways, based on oeso-gastro-duodenal fibroscopy, which allows visualization of the trichobezoar, and is also of therapeutic interest, enabling endoscopic extraction of small trichobezoars [6,7].
Imaging diagnosis is based on CT scans, which have both diagnostic and prognostic value [2].
It reveals an intraluminal, ovoid, mobile and heterogeneous mass with no attachment to the intestinal wall, and the presence of air bubbles dispersed within the mass, as well as dilatation of the upstream loops [8].
Therapeutic management depends on the presence or absence of complications such as occlusion. For small trichobezoars, endoscopic treatment remains the best option, but surgery has its place in therapeutic management for voluminous forms, as well as intestinal localization, as in the case of our patient [1].
Laparotomy with gastrotomy is recommended to remove the trichobezoar from the stomach [9] or enterotomy to remove the trichobezoar from the intestine.
Therapeutic management also includes psychiatric support to prevent recurrence [10].
Conclusion
Trichobezoar is a rare pathology, with a strong female predominance, and is often associated with psychiatric disorders.
It is often asymptomatic, but manifests itself after a complication, as in the case of our patient who presented with a trichobezoar occlusion with both gastric and intestinal localization.
Therapeutic management involves removal of the trichobezoar either endoscopically or surgically, and psychological support is an essential part of the treatment.
References
- Mazine K, Barsotti P, Elbouhaddouti H, Mouaqit O, Benjelloun E, et al. Trichobézoard gastroduodénal: à propos d’un cas [Gastroduodenal trichobezoar: about a case]. Pan Afr Med J, 2018; 30: 25. French. doi: 10.11604/pamj.2018.30.25.12239.
- Mouffak A. Article Case report Cause rare d ’ occlusion mécanique chez l ’ enfant : à propos d ’ un cas, 2021.
- Characteristics CT, García-aguayo J, Martínez M, Gil P. Gastrointestinal Bezoars, 2001; 65–69.
- Ceaux E, Binet A, Lefebvre F. ´ ale re ´ cidivante par trichobe ´ zoar Occlusion ile chez une enfant de 5 ans, 2014; 1375–1379.
- Alsafwah S, Alzein M. Small bowel obstruction due to trichobe- zoar : role of upper endoscopy in diagnosis, 2000; 52(6): 4–6.
- Ousadden A, Mazaz K, Mellouki I, Taleb KA. Le trichobézoard gastrique : une observation The gastric trichobezoar : one case report, 2004; 129: 237–240.
- Michaud L. Ingestion de corps e Recommandations du Groupe francophone ´ patologie , gastroente ´ rologie et nutrition d ’ he ´ diatriques pe, 2009; 54–61.
- Billaud Y, Pilleul F, Valette PJ. Mechanical small bowel obstruction due to bezoars: correlation between CT and surgical findings. J Radiol, 2002; 83(5): 641–646.
- Surgery P, Ohnesorge S, Surgery P, Medicine N, Zochowski K, Medicine N, et al. Department of Gastrointestinal and Paediatric Surgery Oslo University Hospital Susanne Ohnesorge, specialty registrar in paediatric surgery. The author has completed the ICMJE form and declares no conflicts of interest.
- Paparoupa M, Schuppert F. Medical images, 2016; 91: 275–276.

