Necrotizing Fasciitis at Injection Site about a Case
Amine Bachar, Zakaria Essaidi, Zarhouni Baallal Malik*, Khalid El hattabi, Fatima zahra Bensardi, El Bakouri Abdelillah, Bouali Mounir and Abdelaziz Fadil
Service des Urgences Chirurgicales Viscérales, CHU Ibn Rochd, Université Hassane II, Faculté de Médecine et de Pharmacie (FMPC), Casablanca, Morocco
Received Date: 06/05/2024; Published Date: 26/09/2024
*Corresponding author: Zarhouni Baallal Malik, Service des Urgences Chirurgicales Viscérales, CHU Ibn Rochd, Université Hassane II, Faculté de Médecine et de Pharmacie (FMPC), Casablanca, Morocco
Summary
Necrotizing fasciitis is a rare infection of the skin and deep subcutaneous tissues, spreading along the fascia and fatty tissue. It is mainly caused by the group A streptococcus Streptococcus pyogenes but also by other bacteria such as Vibrio vulnificus, Clostridium perfringens or Bacteroides fragilis. Necrotizing fasciitis is a real medical and surgical emergency. In this work, we report a very rare observation of abdominal parietal gangrene occurring in a 70-year-old obese patient with type 2 diabetes for 20 years on insulin who consulted the emergency room for pain in the left iliac fossa. She was conscious 13/15 on the Glascow scale, tachycardic, febrile (39.5°C), and her capillary blood sugar was 3.28 g/L with 2 acetone crosses on the urine strip. Abdominal examination noted a warm erythematous-erosive plaque in the right iliac fossa centered by well-limited necrosis. The patient’s companion reported that she had been injecting insulin at this same location for 5 years. The biological assessment showed hyperleukocytosis at 18,500/mm3, CRP at 180 mg/L.
Abdominal ultrasound and CT scan showed thickening of the abdominal wall without abscesses or deep collections. The diagnosis was that of necrotizing fasciitis.
This patient was treated with broad-spectrum antibiotic therapy with flattening and wide excision. The patient died on postoperative day 2 in the intensive care unit.
Keywords: Necrotizing fasciitis; Abdominal wall; Postoperative; Streptococcus
Introduction
Necrotizing fascitis is a rare infection of superficial or deep skin tissues. The increase in its incidence is increasing following the increase in the prevalence of some risk factors, notably glycemic imbalance and obesity.1 The mortality rate of this infection is high, with rapid progression towards septic shock and multiorgan failure. The infection can be fatal and requires emergency medical and surgical treatment. The abdominal location of necrotizing fascitis is among the rarest. It is all the more exceptional after repetitive insulin injections in the same place, as in our patient. Therapeutic education and learning the rules of asepsis, particularly among the elderly and people of low socio-economic level, are of fundamental importance.
Patient and Observation
This is a 70-year-old patient who has a history of : android obesity and insulin-dependent diabetes who has been taking insulin for 20 years. The patient consulted the university emergency reception service of the IBN ROCHD University Hospital in Casablanca for diffuse and very intense abdominal pain. Physical examination in the emergency room upon admission found a conscious patient 13/15, febrile (temperature 39° 5), pain with a visual analog scale (VAS) level of 5 and asthenic. Cardiovascular examination found sinus tachycardia at 120 beats per minute and arterial hypotension at 8050 mm Hg with normal cardiopulmonary auscultation.
Abdominal examination notes diffuse abdominal tenderness with the presence of a warm erythematous-erosive plaque in the right iliac fossa centered by well-limited necrosis (Figure 1). On biology, we found acute renal failure with a urea of 15 mmol/l and a creatinemia of 210 umol/. The blood count noted hyperleukocytosis at 18,500 elements/mm3 with a predominance of polynuclear neutrophils (12,500 elements/mm3). CRP is 180 mg/l, blood sugar is 3.28 g/L. An emergency abdominal-pelvic scan showed extensive abdominal parietal gangrene without intra-abdominal septic focus (Figure 2). The patient was immediately admitted to the intensive care unit. She had volume expansion.
With isotonic saline then required intubation, mechanical ventilation and the introduction of norepinephrine as a catecholamine. The patient was also treated with empirical broad-spectrum parenteral antibiotic therapy with ceftriaxon 2G and amikacin at a dose of 1 gram per day and metronidazole 1.5 grams per day intravenously. A surgical indication was made. On exploration, areas of necrosis were observed in the subcutaneous tissues with pockets of pus (collapsed). The necrosis occurs in the rectus abdominis muscle with damage to the posterior aponeurotic sheath and the broad muscle of the abdomen. By location (Figure 2). A wide resection of the necrotic tissues was carried out followed by abundant washing with saline with Betadine and diluted hydrogen peroxide. The patient was transferred to the intensive care unit. The germs found in the bacteriological samples and in the blood cultures are Enterococçus Faecalis sensitive to amoxicillin and Escherichia Coli multi sensitive.
The evolution was rapidly unfavorable with the onset of a state of shock refractory to norepinephrine with multi-organ failure. The patient died on D2 postoperatively.

Figure1: Image showing necrotizing faciitis at the starting point of the right iliac fossa.

Figure 2: Post-operative image after debridement.
Discussion
Necrotizing fascitis is a necrotizing bacterial dermohypodermitis affecting by definition the superficial fascia associated or not with muscular damage (myonecrosis, gas gangrene) [3,5]. Rarely encountered in our practice, there are very few data concerning the epidemiology of necrotizing fasciitis [5]. For invasive streptococcal A infections, 5 to 10% of forms with fasciitis are described in the USA and the Canada [3,5].
Group A Streptococcus-hemolytia.ue (streptococcal fascicitis) and Clostridium perfringens (gas gangrene) are the pathogens causing this pathology [1,3]. It is most often polymicrobial (40 to 90% of cases) in patients with risk factors [6]. The infection begins with necrosis of the hypodermis with vascular thrombosis. The necrosis subsequently extends to the underlying superficial aponeurosis then secondarily to the dermis [3]. The germs secrete enzymes responsible for liquefactive necrosis of the superficial fascia and toxins which spread throughout the organism causing septicemia [4]. The factors recognized risks are : Age > 50 years, diabetes as in the case of our patient (25 to 30% of cases), peripheral vascular disorders (36%), chronic alcoholism and drug addiction (15 to 20%), immunodepression (cancers, immunosuppressive treatments, chemotherapy) [3,6]. Alr are often found as an aggravating factor. A study in pediatrics found a relative risk of fasciitis when using ibuprofen. The child during chickenpox [5]. The clinical presentation of necrotizing fasciitis is very often telling. The pain is initially at the forefront without necessarily cutaneous signs, associated with a high fever [5). At an advanced stage, signs of sepsis appear, skin lesions (erythema, hemorrhagic bullous lesion, gas gangrene) with hypoesthesia [5,7].
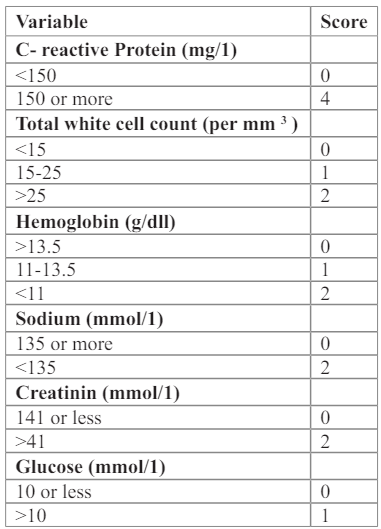
Standard biological examinations have a dual interest : to assess the general impact of severe sepsis on the different organs and to establish a diagnostic score called LRINEC (Laboratory Rişk Indicator, for Necrotizing Fasciitis) (Table 1). A score greater than 8 is strongly predictive of necrotizing fasciitis (PPV = 93.4%) [4, 5]. Bacteriological culture of infected tissues is useful for adapting antibiotic therapy [1]. Standard x-rays are often more sensitive than clinical examination to detect gas in the soft tissues. The reference examinations are the spiral CT scan and the MRI allowing to see thickening of the fascia, heterogeneity of the fat and the presence of gas [5]. These examinations also allow an assessment of the extension of the lesions which is well correlated with surgery.
Table 1: Score de LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis).
The treatment of necrotizing fascitis consists of early and complete debridement of infected and necrotic tissue in order to limit the extension of the infectious process [5,6]. Reconstructive surgery can only be considered after healing and control. Of the infection [1]. In our case, wide resection of the necrotic tissues was carried out then abundant saline washing with Betadine and iluted hydrogen peroxide. Reconstruction surgery would have been planned if the progression. Was favorable later [3].
No randomized study has proven the effectiveness of hyp⁷erbaric oxygen therapy (HBOT) in the management of necrotizing fasciitis. Only experimental data support HBOT in gas gangrene [5,9]. The complementary use of VAC (Vacuum Assisted Closure) in this indication appears promising to accelerate healing. The results obtained are close to those observed with an aeration system described by Kostantinoy 3).
Antibiotic therapy is the second pillar of treatment for necrotizing fasciitis [5]. Antibiotics are most often complementary to surgical treatment because local penetration is insufficient due to vascular thrombosis responsible for necrosis of the deep planes. The goal of antibiotic treatment is to limit the progression of the infection [3,5,10]. Intensive treatment of septic shock resuscitation is of course a fundamental objective. Corticosteroid therapy, even at the dosages of opotomy replacement therapy, as well as the place of activated protein C are discussed given the budding and hemorrhagic problems. Enteral nutrition must be early and high in calories (40 to 45 kcal/.kg/.d) in order to promote healing. Glutamine and intravenous immunoglobulin therapy may be offered by analogy with the management of severe burns, but there are no studies in necrotizing fasciitis [1, 5]. Its prognosis depends on two main factors : the early diagnosis and initial treatment. A delay of less than or more than 24 hours between diagnosis and surgery is associated with a mortality rate of 36% and 70% respectively [3].
Conclusion
Conflicts of interest: The authors declare no conflict of interest.
Author contributions: All authors contributed to the conduct of this work. All authors also declare that they have read and approved the final version of the manuscript.
References
- Sonali Prabhakar Khadakkar, Vivek V Harkare. Necrotising Fasciitis of the Neck and Anterior Chest Wall. Indian J Otolaryngol Head Neck Surg, 2011; 63(Suppl 1): S87–S89.
- Ameziane L, El Bardouni A, Mahfoud M, et al. La Fasciite Nécrosante. Médecine du Maghreb, 1997; 66: 23–25.
- David Jérémie Birnbaum, Xavier Benoit D'Journo, Jean Philippe Avaro, et al. Fasciite nécrosante de la paroi thoracique. Chirurgie Thoracique Cardio-Vasculaire, 2009; 13: 49–52.
- Chin-Ho Wonga, Yi-Shi Wangb. The diagnosis of necrotizing fasciitis. Current Opinion in Infectious Diseases, 2005; 18(2): 101–106.
- Hervé Dupont. Pathologies infectieuses.France: MAPAR; Fasciites Nécrosantes, 2007.
- David B Safran, William G Sullivan. Necrotizing Fasciitis of the Chest Wall. Ann Thorac Surg, 2001;v72(4):v1362–1364.
- Julian E Losanoff, James W Jones, Bruce W Richman. Necrotizing Soft Tissue Infection of the Chest Wall. Ann Thorac Surg, 2002; 73(1): 304–306.
- Hunald F, Samison LH, Rakotoarijaona A, Ranaivozanany A. Multiples incisions étagées et tunnelisées de la gangrène de fournier extensive, Médecine d. Afrique Noire, 2006; 53(1).
- José Dario Frota Filho, Carlos Drews, Paulo Leães, et al. Postoperative Necrotizing Fasciitis of the Thorax in Cardiac Surgery. Arq Bras Cardiol, 2001; 76(3): 250–254.
- Si-Hyun Kim, Kyoung Ho Roh, Young Kyung Yoon, et al. Necrotizing fasciitis involving the chest and abdominal wall caused by Raoultella planticola. BMC Infectious Diseases, 2012; 12: 59.

