Incidental Discovery of an Intrauterine Device After 30 Years of its Placement
El Hattabi Khalid*, Essaidi Zakaria, El kinani Siham, Bouali Mounir, El Bakouri Abdelilah, Bensardi Fatima Zahra and Fadil Abdelaziz
Department of visceral surgery, University Hassan II, Faculty of Medicine and Pharmacy of Casablanca, CHU Ibn Rochd, University of Hassan II, Casablanca, Morocco
Received Date: 10/04/2024; Published Date: 25/09/2024
*Corresponding author: El Hattabi Khalid, Department of visceral surgery, University Hassan II, Faculty of Medicine and Pharmacy of Casablanca, CHU Ibn Rochd, University of Hassan II, Casablanca, Morocco
Abstract
The Intrauterine Device (IUD) is one of the most effective and widely used contraceptive methods in the world, with around 100 million users. Perforation remains exceptional after IUD insertion, but is one of the most serious complications. We report the case of an 83-year-old female patient who had undergone IUD insertion 30 years ago and was admitted for a type I hydatid cyst of segment VIII. A thoraco-abdomino-pelvic CT scan revealed the presence of a type I hydatid cyst of the liver in segment VIII, without visualization of the IUD. Intraoperative exploration of the peritoneal cavity revealed the presence of an IUD embedded in the omentum in the right parietocolic gutter.
In the light of our review of the literature, we emphasize the efficacy and safety of the IUD when the technique and indications are strictly respected, but also call attention to rare complications of IUD insertion, and highlight the importance of intraoperative exploration, whatever the diagnosis.
Keywords: Intraperitoneal; Intrauterine device; Laparoscopy; Migration
Introduction
Intrauterine device contraception is one of the most widely used methods in the world, with around 100 million users. It's a simple, effective and reversible method, with a Pearl index of less than 1 per 100 female years. Its contraceptive action is directed at the fallopian tubes and spermatozoa, as well as the uterine cavity. However, their side effects, complications and contraindications must be known in order to optimize their action [1,2]. Perforation is one of the rarest and most serious complications, and can lead to migration of the IUD into the various neighbouring organs. Migration into the rectouterine pouch, omentum, mesentery, colon and bladder has been described [2]. We report a new case of IUD migration into the peritoneal cavity, discovered incidentally 35 years after insertion during intraoperative exploration during surgery for a hydatid cyst of the liver.
Patient and Observation
This is an 83-year-old patient, multiparous, having had her vaginal deliveries menopausal 20 years ago and wearing an IUD for 35 years, who was neglected by the patient, followed for complete arrhythmia by atrial fibrillation under anticoagulant and antiarrhythmic drugs.
Admitted to our department for management of a hydatid cyst in the segment VIII of the liver classified type I.
Clinically, the patient presented with right hypochondrium pain of the heaviness type with no other associated signs, and had no gynecological symptoms. Clinical examination revealed slight tenderness in the right hypochondrium, and no evidence of an intra-vaginal IUD wire. Abdominal ultrasonography revealed a type I hydatid cyst in segment VIII of the liver (Figure 1), without visualization of the IUD.

Figure 1: Segment VIII type I hydatid cyst.
Thoracic-abdominal-pelvic CT scans showed a cystic formation in segment VIII of the liver (Figure 2) and did not describe the presence of IUDs, even though the images showed spontaneously hyperdense material (Figure 3). Hydatid serology was negative at 0.117.
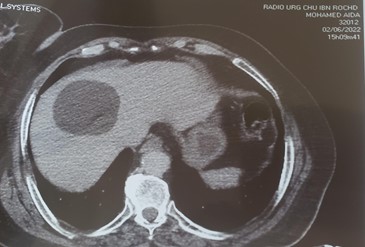
Figure 2: Cystic formation in segment VIII of the liver.

Figure 3: Spontaneously hyperdense material.
Intraoperative exploration revealed the presence of a Lippes loop IUD embedded in the omentum (Figure 4), which was removed without incident after its detachment from the omentum. The patient was seen again one month and 3 months later, and is in good health.


Figure 4: Lippes loop IUD embedded in the omentum.
Discussion
The IUD is one of the most widely used long-term reversible contraceptive methods in the world. But like any foreign body, it can present complications [3], notably migration after uterine perforation, which remains rare, and even rarer is a peritoneal localization. According to recent studies, this represents a rate of between 1.3 and 1.8 per 1000 [4].
Most authors report no suggestive signs [5], and perforation is diagnosed in only 14% of cases [6]. The first sign of migration is the disappearance of landmark threads.
The perforation rate seems to depend on the practitioner's qualifications and, above all, on the number of insertions performed [6]. Statistically significant risk factors for perforation have been identified: in the case of post-partum insertion, the relative risk of perforation is 11.7 within 3 months, and 13.2 within 4 to 6 months of delivery; in the case of insertion in a patient with a history of termination of pregnancy by uterine aspiration or curettage, the RR is 2.1, with a higher risk the more immediate the post-abortal insertion [6].
It's only at a more advanced stage that the symptomatology becomes more demonstrative: abdominal pain (30%) and unwanted pregnancy (25%) [6]. When the IUD is outside the uterine cavity, it may be located either in the pelvis or abdomen, and in order of frequency: in the omentum, rectus sigmoidum, peritoneum, bladder, appendix, small intestine, adnexa and iliac vein [7].
Clinical diagnosis is not always obvious, and further investigations are required to locate the device, including endovaginal ultrasound, CT scan or magnetic resonance imaging [6]. The WHO recommends surgical removal of migrated IUDs using minimally invasive methods, including hysteroscopy, cystoscopy, colonoscopy or laparoscopy, depending on the location of the IUD [8].
Conclusion
IUDs are effective contraceptive measures, and the majority of patients with uterine perforation due to IUD migration are asymptomatic. Diagnosis relies on thorough gynecological analysis and appropriate radiological imaging.
Conflicts of interest: The authors declare having no conflicts of interest for this article.
Ethical Approval: I declare on my honor that the ethical approval has been exempted by my establishment.
References
- Boudineau M, Multon O, Lopes P. Contraception par dispositif intra-utérin. Encycl Méd Chir- Gynécologie, 2001; 738-A-09: 7.
- Zouhal A, el Amrani N, Bensaid F, et al. Migration intra-vesicale d′un dispositif intra-uterin a propos d′un cas.Rabat, Maroc: Maternité Universitaire des Orangers, 2000-2001.
- Verim L, Akbaş A, Erdem MR. Intravesical Migration and Calcification of Intrauterin Device: A Case Report and Review of the Literature. J UrolSurg, 2020; 2(4): 197-199.
- Arslan A, Kanat-Pektas M, Yesilyurt H, Bilge U. Colon penetration by a copper intrauterine device: a case report with literature review. Arch GynecolObstet, 2009; 279(3): 395-397.
- Cuillier F, Ben Ghalem S, Haffaf Y. Stérilet appendiculaire:une exceptionnelle complication. J GynecolObstetBiolReprod, 2003; 32: 55-57.
- Cristinelli S, Nisolle M, Foidart J-M, « Le cas clinique du mois. Sterilet en position annexielle: une complication rare ».Rev Med Liege, 2006; 61(11): 747-749.
- El Kettani NE-C, Dafiri R. Imagerie de la migration des dispositifs intra-utérins. FeuillRadiol, 2007; 47(3): 159–166.
- Mamadou Bissiriou Bah, et Al Migration of an Intra Uterine Device (IUD) on a Bilharzian Bladder: An Exceptional Fact About a Case, International Journal of Clinical Urology, 2020; doi: 10.11648/j.ijcu.20200402.14.

