A Rare Case Report of Isolated Left Sided Partial Anomalous Pulmonary Venous Connection with Right Meandering Pulmonary Vein
Subramony H*, Ruba P, Arivukarasan, Eswar subbaiyan and Tamilselvan
Department of General Medicine, Apollo Main Hospital, Greams road, India
Received Date: 13/04/2024; Published Date: 09/09/2024
*Corresponding author: Dr. Subramony H, MBBS, MD General Medicine, MRCP, Department of General Medicine, Apollo Main Hospitals, Greams road, Chennai, India
Abstract
Isolated partial anomalous pulmonary venous connections with intact atrial septum are a relatively rare condition [1]. Meandering pulmonary vein is a very uncommon pulmonary venous anomaly with less than 20 reported cases [2]. Here we present a case of incidental diagnosis of isolated left sided anomalous pulmonary venous connection with right meandering pulmonary vein in a middle-aged man who was asymptomatic with no hemodynamic effects on right heart, presently intervention deferred. Is intervention required?
Keywords: Isolated PAPVC; Meandering pulmonary vein; Asymptomatic
Introduction
PAPVC is characterized by drainage of one or more pulmonary veins into right atrium or systemic circulation instead of left atrium [3]. Normal pulmonary venous pattern with four pulmonary veins and different ostia is present in 60-70% of the population whereas 38% of the population were found to have anomalous pulmonary venous variation [4]. One fourth of pulmonary blood flow is contributed by each pulmonary vein [3]. The most common vein involved in PAPVC is right upper pulmonary vein [4]. Origin of PAPVC from left sided pulmonary veins occur in 3-8% of the cases [5]. Presence of at least 2 aberrant connecting veins in PAPVC causes significant shunting [3]. Left to right occurs similar to atrial septal defect/ventricular septal defect/patent ductus arteriosus [4]. Patient with isolated PAPVC is usually asymptomatic [1]. Anomalous pulmonary vein with a tortuous intrapulmonary course although eventually draining normally into left atrium constitutes meandering pulmonary vein [2].
Case Report
53 years old male known case of type 2 diabetes mellitus presented with the chief complaints of non-healing ulcer over the right foot for the past 3 months. He denied any history of breathing difficulty, palpitation, abdominal distension or swelling of legs. On examination patient was conscious and oriented. Vitals examination showed Blood pressure- 130/80 MMHG, pulse rate- 82/minute, Respiratory rate- 16/min, Temperature- 98 Fahrenheit and JVP – not elevated. There was no hepatomegaly or ascites. His baseline blood investigations revealed anemia, elevated blood glucose and HbA1C. Right lower limb arterial Doppler study was normal. On routine evaluation Chest X-ray PA view was done which showed dilated and tortuous pulmonary vascular markings on the right side (Figure 1). Transthoracic echocardiography- two-dimensional M mode with color Doppler showed ejection fraction of 66%, with no evidence of right atrial or ventricular dilation and pulmonary hypertension. In view of incidental finding on the chest x-ray 640 slice computed tomography of pulmonary angio was done which showed partial anomalous pulmonary venous return with left upper lobe pulmonary vein draining into the left brachiocephalic vein (Figure 2). Dilation and tortuosity of the right lobe pulmonary veins are noted in the right lung parenchyma (Figure 3). Few branches of right upper lobe pulmonary vein are noted joining the tortuous branches of right lower lobe pulmonary vein and draining into the left atrium through right inferior pulmonary vein suggestive of meandering pulmonary vein (Figure 4-7).

Figure 1: Arterial and venous connections of all the four chambers of heart.
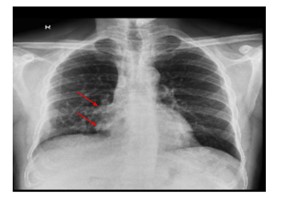
Figure 2: Chest x-ray PA view showing dilated and tortuous pulmonary markings on the right side.

Figure 3: Electrocardiography of the patient.

Figure 4: Two-dimensional M mode trans echocardiography showing normal sized Right atrium and ventricle.
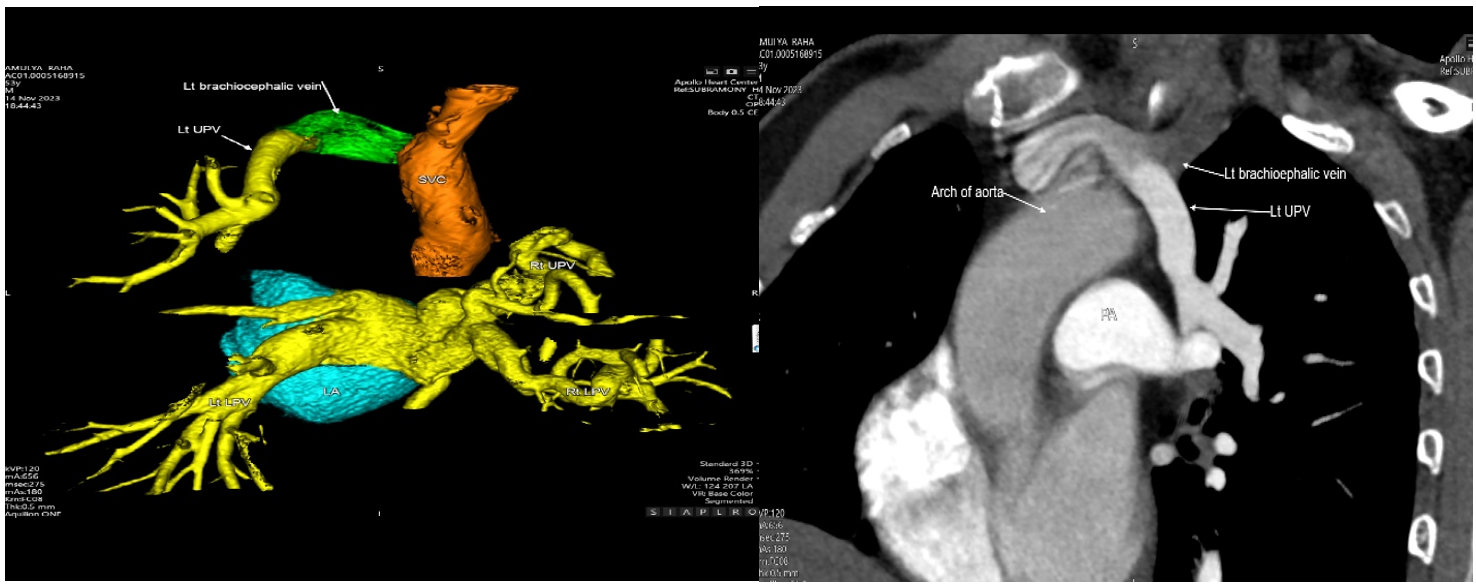
Figure 5: 640 slice CT Pulmonary Angiogram showing left upper pulmonary vein draining into the brachiocephalic vein.

Figure 6: 640 slice CT pulmonary Angiogram showing dilated right lower pulmonary vein.
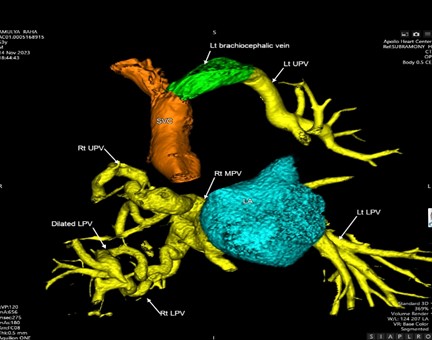
Figure 7: 640 slice CT Pulmonary angiogram showing meandering right pulmonary vein [branches of right upper lobe vein draining into right lower pulmonary vein].
Discussion
In our case patient had isolated left sided PAPVC with right meandering pulmonary vein. Both of them are rare presentations of pulmonary venous anomaly.
Embryology of pulmonary veins is a complicated process. Blood returning from the lung buds initially drain into the splanchnic plexus which in turn eventually drains into paired cardinal and umbilic vitelline veins. Right superior vena cava is formed from the right cardinal system whereas left cardinal system mostly disappears and may potentially develop into left superior vena cava in less than 1% of the population. Inferior vena cava, portal venous system and ductus venosus develop from umbilic vitelline veins. A primitive common pulmonary vein is formed from the outpouching of dorsal wall of left atrium. Gradually common pulmonary vein communicates with the portion of splanchnic plexus. Pulmonary venous connection to the cardinal and umbilicovitilline veins gradually involute and gets incorporated into left atrium to form four separate pulmonary veins. Pulmonary venous anomalies develop as a result of failure of this process [6].
PAPVC was initially described by Winslow in 1739 as persistence of embryonic anastomosis between systemic and pulmonary venous plexus [3]. Prevalence of PAPVC is around 0.4-0.7%. It can be right sided, left sided or bilateral [4]. PAPVC is predominantly associated with atrial septal defect [7]. 85% of PAPVC were associated with sinus venosus ASD whereas 10-15% were associated with secondum ASD [4]. Shunt hemodynamics is predicted based on the quantity and caliber of pulmonary veins and other associated cardiopulmonary defects [3]. Isolated PAPVC’S on long term may develop pulmonary hypertension and right ventricular dilation which needs follow up [1]. Diagnosis of PAPVC should be considered in the setting of trans thoracic echocardiography showing right heart dilation in the absence of congenital heart disease [3]. Trans thoracic echocardiography is less sensitive- as one third cases of PAPVC were left undiagnosed [3]. Trans esophageal echocardiography is preferred than TTE in view of its high sensitivity and efficacy [4]. Multidetector computed tomography and magnetic resonance imaging are the most efficient methods of imaging [4]. Velocity encoded phase contrast magnetic resonance imaging can be utilized in accurately quantifying the ratio of pulmonary to systemic blood flow [6]. Surgical repair has been found beneficial in left sided PAPVC, right heart enlargement, patients with tricuspid regurgitation and clinical symptoms [8]. Meandering pulmonary vein was first described by Goodman et al [9]. Meandering pulmonary vein is often confused with scimitar syndrome when it occurs on the right side as both show prominent vertically running vascular shadow on chest radiograph [2]. Majority of meandering pulmonary veins have been reported on the right side [2]. Differential diagnosis of meandering pulmonary veins includes classical scimitar syndrome, pulmonary varix, pulmonary malformations and pulmonary nodules [10]. Surgical intervention should take into account of the nature of PAPVC, it’s contribution to overall clinical picture, underlying co-morbid conditions, shunt index severity, patient’s life expectancy and complications associated with PAPVC repair [11].
- PAPVC of left sided pulmonary veins is unusual.
- Isolated PAPVC- PAPVC without atrial septal defect or other congenital heart defects.
- Presence of meandering right upper lobe pulmonary vein.
- Absence of clinical features of pulmonary hypertension.
Above 4 peculiarities made us to present this case.
Author’s contribution: Subramony H, Ruba, Eswar, Arivukarasan and Tamilselvan contributed towards literature search, data collection and drafting of the article, while Subramony H and Ruba contributed towards important content writing and final editing of the article.
Funding: None
Patient’s consent: Telephonic consent was obtained from the patient in view of any anonymity.
Conflict of interest: None
Ethical approval: Not required
References
- Shah AH, Oechslin E, Benson L, Crean AM, Silversides C, Bach Y, et al. Long-Term Outcomes of Unrepaired Isolated Partial Anomalous Pulmonary Venous Connection with an Intact Atrial Septum. Am J Cardiol, 2023; 201: 232-238. doi: 10.1016/j.amjcard.2023.05.049.
- Lee M, Jeon KN, Park MJ, Bae K. Meandering pulmonary veins: Two case reports. Medicine (Baltimore), 2020; 99(16): e19815. doi: 10.1097/MD.0000000000019815.
- Seecheran RV, Dookie T, Seecheran VK, et al. Partial Anomalous Pulmonary Venous Connection: A Great Imitator? Journal of Investigative Medicine High Impact Case Reports, 2020; 8. doi:10.1177/2324709620933425
- Verma AK, Sethi S, Kohli N. Partial anomalous pulmonary venous connection: state-of-the-art review with assessment using a multidetector computed tomography angiography. Pol J Radiol, 2022; 87: e549-e556. doi: 10.5114/pjr.2022.120513.
- Kumar T, Patra S, Ramalingam R, Agrawal N, Agarwal A, Manjunath CN. Pulmonary hypertension due to presence of isolated partial anomalous pulmonary venous connection: A Case report. J Cardiovasc Dis Res, 2013; 4(4): 239-241. doi: 10.1016/j.jcdr.2014.01.002.
- Dillman JR, Yarram SG, Hernandez RJ. Imaging of pulmonary venous developmental anomalies. AJR Am J Roentgenol, 2009; 192(5): 1272-1285. doi: 10.2214/AJR.08.1526.
- Sahay S, Krasuski RA, Tonelli AR. Partial anomalous pulmonary venous connection and pulmonary arterial hypertension. Respirology, 2012; 17(6): 957-963. doi: 10.1111/j.1440-1843.2012.02180.x.
- El Bardissi AW, Dearani JA, Suri RM, Danielson GK. Left-sided partial anomalous pulmonary venous connections. Ann Thorac Surg, 2008; 85(3): 1007-1014. doi: 10.1016/j.athoracsur.2007.11.038.
- Murat Serhat Aygun, Mustafa Calik, Saniyae Goknil Calik. Meandering pulmonary vein: very rare incidental finding. doi: 10.4103/ejop.ejop_4_18
- Sneha Harish C, Dixit R, Agarwal A, Garg A. Meandering pulmonary vein: A case report. J Radiol Case Rep, 2020; 14(3): 7-13. doi: 10.3941/jrcr.v14i3.3799.
- Khalil C, Mosleh W, Ibrahim A, Young H, Corbelli J. A Partial Anomalous Pulmonary Venous Connection in a Severely Symptomatic Patient, Is Surgery Always Recommended? Cureus, 2018; 10(7): e2962. doi: 10.7759/cureus.2962.

